LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide is a once-weekly injectable medication approved for type 2 diabetes and chronic weight management, offering patients flexibility in administration timing. Many patients wonder whether tirzepatide should be taken in the morning or at night for optimal results. According to FDA prescribing information, tirzepatide can be administered at any time of day, with or without meals, as its extended half-life maintains stable therapeutic levels regardless of injection time. The best timing depends on individual lifestyle, tolerability, and adherence patterns. Understanding how to optimize your injection schedule can enhance treatment consistency and help manage potential side effects effectively.
Quick Answer: Tirzepatide can be administered at any time of day, morning or night, as its pharmacokinetic profile maintains stable therapeutic levels with once-weekly dosing regardless of injection time.
Tirzepatide is a once-weekly injectable medication approved by the FDA for the treatment of type 2 diabetes mellitus (marketed as Mounjaro) and chronic weight management in adults with obesity or overweight with weight-related comorbidities (marketed as Zepbound). It represents a novel class of glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, making it the first dual incretin receptor agonist available in clinical practice. Tirzepatide is not indicated for patients with type 1 diabetes.
The medication works through multiple complementary mechanisms to improve glycemic control and promote weight loss. By activating GIP receptors, tirzepatide enhances insulin secretion in a glucose-dependent manner, meaning insulin release occurs primarily when blood glucose levels are elevated, thereby reducing the risk of hypoglycemia. Simultaneously, GLP-1 receptor activation suppresses glucagon secretion, slows gastric emptying, and reduces appetite through central nervous system pathways that regulate satiety. This dual action results in improved postprandial and fasting glucose levels, along with significant reductions in body weight.
Tirzepatide is administered subcutaneously once weekly at doses ranging from 2.5 mg to 15 mg, with gradual dose escalation recommended to minimize gastrointestinal adverse effects. The medication has a half-life of approximately five days, allowing for consistent therapeutic levels with weekly dosing. Clinical trials have demonstrated robust efficacy, with A1C reductions of 1.9% to 2.4% and weight loss of approximately 15% at 5 mg and 20-21% at 10-15 mg of baseline body weight in the SURMOUNT-1 trial. Understanding the pharmacokinetics of tirzepatide helps inform optimal timing strategies for administration.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
The FDA-approved prescribing information for tirzepatide states that the medication can be administered at any time of day, with or without meals, providing significant flexibility for patients. There is no official recommendation favoring morning versus evening administration, as the pharmacokinetic profile of tirzepatide—with its extended half-life and once-weekly dosing—maintains stable therapeutic levels regardless of injection time. This flexibility represents an important practical advantage, allowing patients to choose a schedule that best fits their lifestyle and daily routine.
Many healthcare providers suggest that patients select a consistent day and time each week that aligns with their schedule and helps ensure adherence. Some patients prefer morning administration because it allows them to incorporate the injection into their morning routine, making it easier to remember. Morning dosing may also be preferred by individuals who want to monitor for potential side effects during waking hours when they can more easily manage symptoms or seek medical attention if needed.
Conversely, some patients opt for evening or nighttime administration, particularly if they experience gastrointestinal side effects such as nausea. Taking tirzepatide before bed may allow patients to sleep through initial side effects, though individual responses vary and there is limited evidence on the optimal timing to minimize specific symptoms. Additionally, evening dosing may be more convenient for individuals with busy morning schedules or those who prefer to administer injections in the privacy of their home after work.
Ultimately, the "best" time is the one that promotes consistent weekly administration. The American Diabetes Association emphasizes in its Standards of Care that medication adherence is a critical determinant of treatment success, and choosing a convenient, memorable time significantly enhances long-term compliance with tirzepatide therapy.
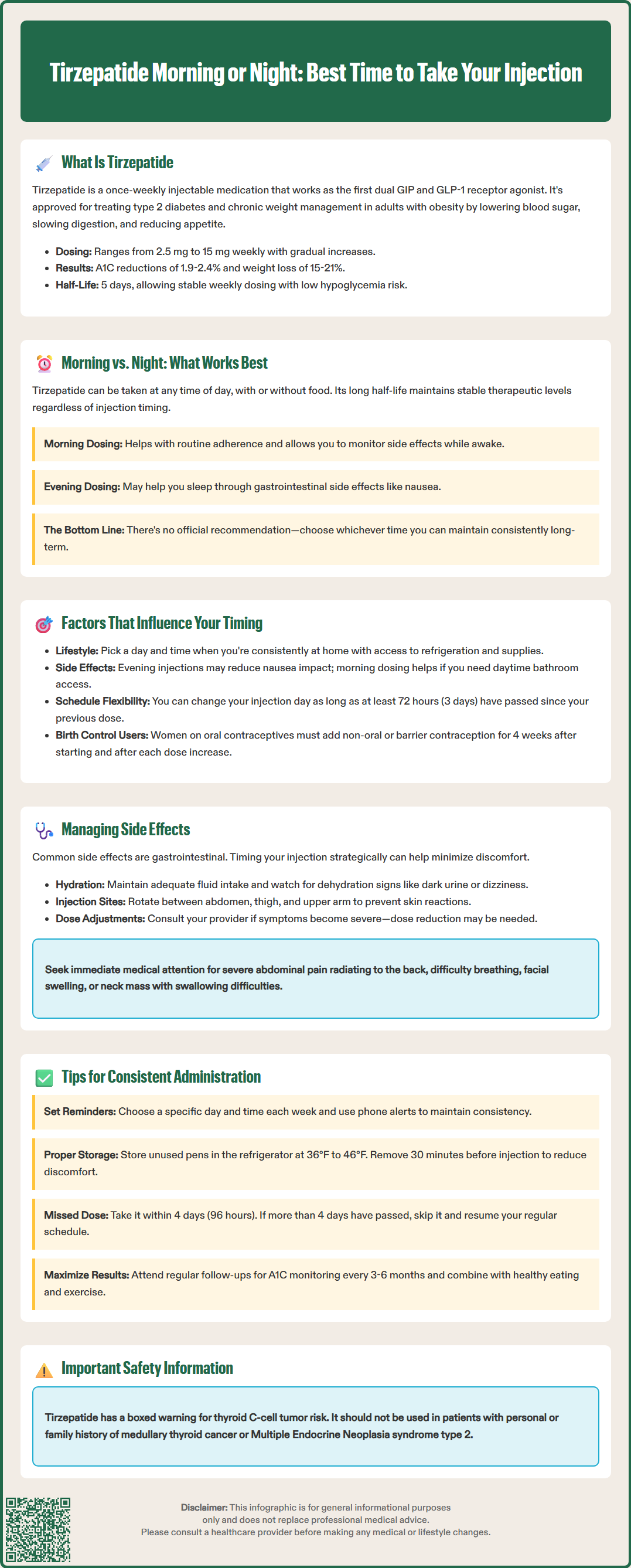
Several individual factors should be considered when determining the optimal injection time for tirzepatide. Personal schedule and routine consistency are paramount—patients should select a day and time when they are typically at home or in a comfortable setting where they can safely prepare and administer the injection. For example, individuals who travel frequently for work may prefer weekend mornings when they are more likely to be at their primary residence with access to proper refrigeration and injection supplies.
Gastrointestinal tolerability patterns can significantly influence timing preferences. Tirzepatide commonly causes nausea, vomiting, diarrhea, and decreased appetite, particularly during dose escalation. Patients who experience pronounced nausea may prefer evening administration, while those who experience minimal gastrointestinal effects may prefer morning dosing to avoid any potential sleep disruption. It is important to note that gastrointestinal side effects typically diminish over time as the body adapts to the medication.
Meal timing and eating patterns may also play a role in decision-making. While tirzepatide can be taken with or without food, some patients find that administering the injection before a meal helps them remember their dose, while others prefer dosing at a time unrelated to eating to avoid potential nausea associations. Additionally, patients should consider their work schedule and social commitments—choosing a time when they can comfortably manage potential side effects without disrupting important activities.
Patients using oral contraceptives should be aware that tirzepatide may reduce the effectiveness of these medications, particularly during initiation and dose escalation. The FDA label recommends using a non-oral contraceptive method or adding a barrier method for 4 weeks after starting tirzepatide and after each dose increase. Patients taking insulin or sulfonylureas should be monitored for hypoglycemia, and dose reductions of these medications may be necessary. Tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis.
If a patient needs to change their injection day, the FDA label permits this as long as the new dose is administered at least 72 hours (three days) after the previous injection.
Strategic timing of tirzepatide administration may help some patients manage common adverse effects, particularly gastrointestinal symptoms that occur during initial treatment and dose escalation. According to the FDA prescribing information, nausea, diarrhea, and vomiting are among the most common side effects, with rates varying by dose. While some patients report that evening administration helps them manage nausea by potentially sleeping through some symptoms, evidence for specific timing recommendations is limited, and responses vary considerably between individuals.
For patients experiencing diarrhea or abdominal discomfort, morning administration may be preferable, as it allows symptoms to manifest during daytime hours when patients have easier access to bathroom facilities and can manage hydration more effectively. Patients should be counseled to maintain adequate fluid intake and monitor for signs of dehydration, including dark urine, dizziness, or decreased urination, which warrant medical evaluation. Severe dehydration may increase the risk of acute kidney injury. If gastrointestinal symptoms become severe or persistent, dose reduction or temporary treatment interruption may be necessary, and patients should consult their healthcare provider.
Injection site reactions—including erythema, pruritus, or mild pain—are generally mild and transient but can be minimized through proper injection technique. Rotating injection sites among the abdomen, thigh, and upper arm reduces the risk of lipohypertrophy and localized reactions. Upper arm injections should be administered by a caregiver. Patients should avoid injecting into areas with active skin conditions, bruising, or scarring.
Patients should be educated about serious adverse effects requiring immediate medical attention, including:
Pancreatitis: severe abdominal pain radiating to the back, persistent vomiting
Hypersensitivity reactions: rash, difficulty breathing, facial swelling
Gallbladder disease: right upper quadrant pain, fever, jaundice
Thyroid C-cell tumors (boxed warning): neck mass, dysphagia, hoarseness, persistent dyspnea
Regular follow-up with healthcare providers ensures appropriate monitoring and timely intervention if adverse effects occur.
Establishing a reliable routine is essential for maximizing the therapeutic benefits of tirzepatide and maintaining optimal glycemic control and weight management outcomes. Patients should select a specific day of the week and time of day for their injection, using calendar reminders, smartphone alarms, or medication tracking apps to ensure they do not miss doses. Consistency in timing helps establish a habit and reduces the likelihood of inadvertent dose omission, which can compromise treatment efficacy.
Proper storage and preparation are critical for medication safety and effectiveness. Tirzepatide pens should be stored in the refrigerator at 36°F to 46°F (2°C to 8°C) in the original carton to protect from light. Unused pens may be kept at room temperature (up to 86°F or 30°C) for up to 21 days. Patients should remove the pen from the refrigerator 30 minutes before injection to allow it to reach room temperature, which can reduce injection discomfort. Tirzepatide pens are for single use only and should be discarded after one injection. Patients should never freeze tirzepatide or use medication that has been frozen, as this can alter its efficacy.
Before injection, patients should inspect the solution, which should be clear and colorless to slightly yellow. Do not use if the solution contains particles or appears cloudy. When administering, patients should rotate injection sites among the abdomen, thigh, or upper arm (with caregiver assistance for upper arm injections). Used pens should be disposed of in an FDA-cleared sharps container or a puncture-resistant container.
If a dose is missed, patients should administer it as soon as possible if fewer than four days (96 hours) have passed since the missed dose. If more than four days have elapsed, patients should skip the missed dose and resume their regular schedule with the next planned injection. Taking two doses within three days of each other is not recommended due to increased risk of adverse effects.
Patients should maintain open communication with their healthcare team, reporting any challenges with administration, side effects, or concerns about efficacy. Regular follow-up appointments allow for assessment of glycemic control (A1C monitoring every 3-6 months), weight trends, and adjustment of tirzepatide dosing as needed. Combining tirzepatide with lifestyle modifications—including a balanced, calorie-appropriate diet and regular physical activity—optimizes treatment outcomes and supports long-term metabolic health.
Some patients report that evening administration may help them sleep through initial nausea, though evidence for specific timing recommendations is limited and individual responses vary considerably. The most important factor is choosing a consistent time that promotes adherence.
Yes, you can change your injection day or time as long as the new dose is administered at least 72 hours (three days) after the previous injection, according to FDA labeling. Consistency with your new schedule is important for maintaining adherence.
Tirzepatide can be administered with or without meals, as food does not significantly affect its absorption or efficacy. Patients should choose a timing approach that best supports their adherence and tolerability preferences.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.