LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

The best time of day to take tirzepatide for weight loss is not specified by FDA guidelines, as clinical evidence shows the medication works effectively regardless of when you inject it. Tirzepatide (Zepbound) is a once-weekly injectable medication that maintains steady therapeutic levels due to its approximately five-day half-life. While timing flexibility exists, consistency matters most—choosing the same day and approximate time each week optimizes adherence and treatment outcomes. Some patients prefer evening administration to sleep through potential gastrointestinal side effects like nausea, though no research definitively proves one timing superior to another.
Quick Answer: There is no specific best time of day to take tirzepatide for weight loss, as FDA guidelines and clinical trials show the medication is effective regardless of injection timing.
Tirzepatide is a once-weekly injectable medication approved by the FDA for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. Marketed under the brand name Zepbound for weight loss, tirzepatide is also approved as Mounjaro for type 2 diabetes management. This dual-action medication represents a significant advancement in pharmacotherapy for metabolic conditions.
The mechanism of action involves dual agonism at both glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptors. By activating these incretin pathways, tirzepatide enhances insulin secretion in a glucose-dependent manner, suppresses inappropriate glucagon release, and slows gastric emptying. These effects collectively reduce appetite and increase satiety, leading to decreased caloric intake. The SURMOUNT clinical trials demonstrated average weight loss of 15–22% of body weight over 72 weeks, with higher percentages observed at the maximum 15 mg dose.
Tirzepatide is administered subcutaneously once weekly at doses ranging from 2.5 mg (starting dose) up to 15 mg for weight management. The medication requires gradual dose escalation every four weeks to minimize gastrointestinal side effects. Patients typically begin noticing appetite suppression within the first few weeks of treatment, with progressive weight loss occurring over several months. The medication works best when combined with lifestyle modifications including reduced-calorie diet and increased physical activity, as recommended by clinical guidelines. Tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2), and is not approved for use in children or adolescents under 18 years of age.
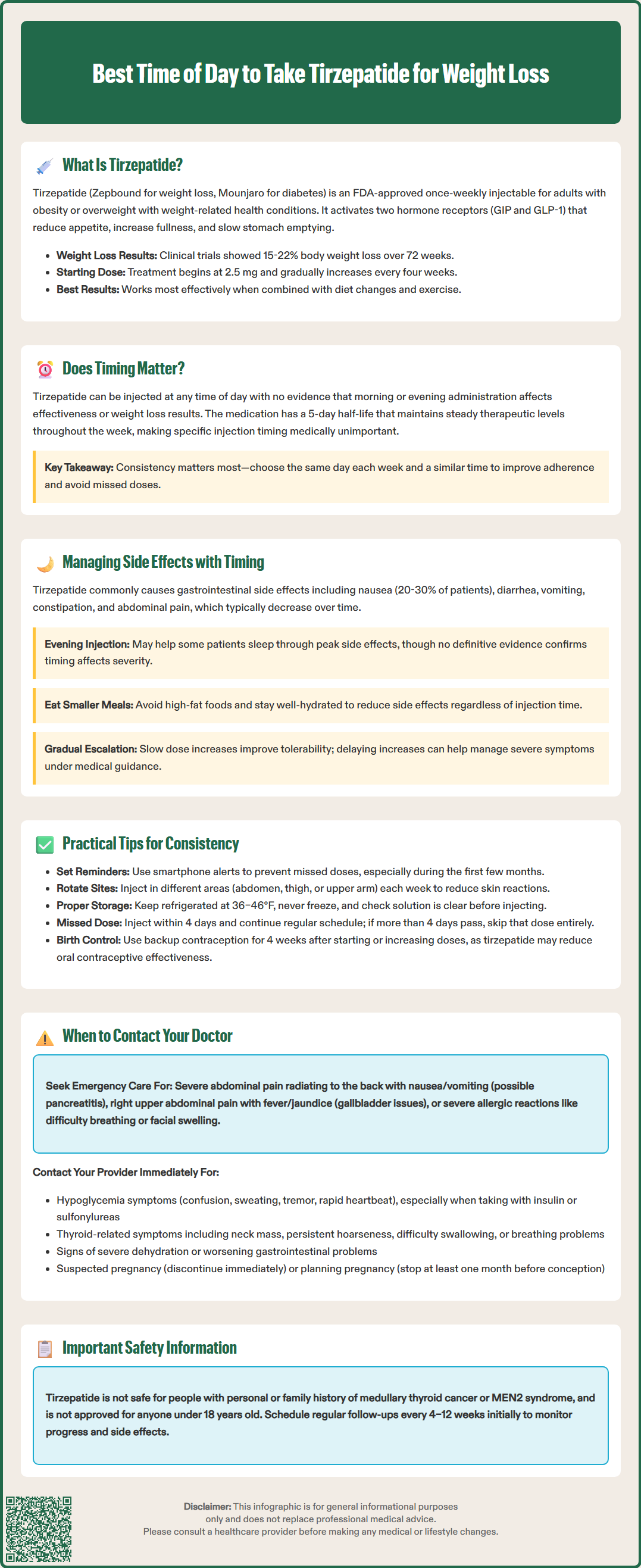
The FDA-approved prescribing information for tirzepatide does not specify a particular time of day for administration, and there is no official evidence demonstrating superior efficacy based on injection timing. Clinical trials that established tirzepatide's effectiveness allowed participants to inject the medication at any time of day, provided they maintained consistency with their chosen weekly schedule. This flexibility reflects the medication's pharmacokinetic profile, with a half-life of approximately five days that maintains steady therapeutic levels regardless of administration time.
Some healthcare providers suggest that patients may benefit from choosing a consistent day and approximate time each week to optimize adherence and minimize the risk of missed doses. As tirzepatide is administered subcutaneously, meal timing does not affect absorption or efficacy. However, individual patient factors may influence the optimal timing choice. For instance, patients who experience nausea—one of the most common adverse effects—might prefer evening administration so that peak side effects occur during sleep.
There is no published research comparing morning versus evening administration for efficacy or tolerability outcomes. The lack of timing-specific guidance in clinical practice reflects the medication's sustained action and stable plasma concentrations achieved with weekly dosing. Patients should select a time that aligns with their routine and facilitates consistent adherence, which is the most critical factor for achieving weight loss goals. Healthcare providers typically emphasize that maintaining the same day each week is more important than the specific hour of injection. If a patient needs to change their weekly injection day, the FDA label advises ensuring at least 3 days between doses.
While there is no definitive evidence linking injection timing to side effect severity, clinical experience suggests that strategic timing may help some patients manage gastrointestinal adverse effects more comfortably. The most common side effects of tirzepatide include nausea (reported in 20–30% of patients), diarrhea, vomiting, constipation, abdominal pain, and decreased appetite. These effects are typically most pronounced during dose escalation and often diminish with continued use as physiologic adaptation occurs.
Some clinicians recommend evening or bedtime administration for patients experiencing significant nausea, allowing them to sleep through the period when side effects may be most noticeable. The medication's effect on gastric emptying is most pronounced after the initial doses and tends to diminish over time with continued treatment. This gastric-slowing effect contributes to both the therapeutic benefit and gastrointestinal side effects.
Patients should be counseled that side effects are generally dose-dependent and transient. The FDA label recommends a gradual dose escalation schedule specifically to improve tolerability. If gastrointestinal symptoms are severe or persistent, delaying dose escalation or temporarily reducing the dose may be appropriate, as guided by the prescribing healthcare provider. Adequate hydration, smaller meal portions, and avoiding high-fat foods can help mitigate side effects regardless of injection timing. Patients experiencing severe or persistent vomiting or diarrhea should be monitored for dehydration and potential acute kidney injury. Patients experiencing severe abdominal pain should seek medical evaluation promptly, as tirzepatide carries warnings for acute pancreatitis, though this remains a rare complication.
Adherence to the weekly injection schedule is essential for achieving optimal weight loss outcomes with tirzepatide. Establishing a consistent routine significantly improves medication compliance. Patients should select a specific day of the week that aligns with their schedule—many choose the same day they attend weekly commitments or have predictable routines. Setting smartphone reminders or calendar alerts can help prevent missed doses, particularly during the initial months of treatment.
The injection can be administered in the abdomen, thigh, or upper arm, and patients should rotate injection sites weekly to minimize local reactions such as redness, itching, or induration at the injection site. Proper injection technique is critical: the medication should be stored in the refrigerator (36–46°F) until use, though it may be kept at room temperature (up to 86°F/30°C) for up to 21 days if needed. The pen should be protected from light and should never be frozen. Patients should inspect the solution before each injection—it should be clear and colorless to slightly yellow. Any discoloration or particulate matter indicates the medication should not be used.
If a dose is missed, the FDA label provides clear guidance: if fewer than four days have passed since the missed dose, inject as soon as possible and resume the regular weekly schedule. If more than four days have passed, skip the missed dose and administer the next dose on the regularly scheduled day. When changing the weekly injection day, ensure at least 3 days between doses. Never double doses to compensate for a missed injection. Patients should maintain a log of injection dates and any side effects experienced, which can be valuable information for healthcare provider visits. Used pens should be disposed of properly in a sharps container and never shared with others.
Women using oral contraceptives should be aware that tirzepatide may reduce the effectiveness of these medications. The FDA recommends using a non-oral contraceptive method or adding a backup method for 4 weeks after initiating tirzepatide and for 4 weeks after each dose increase.
Patients should maintain regular follow-up with their healthcare provider throughout tirzepatide therapy, typically every 4–12 weeks initially, then less frequently once stable. However, certain symptoms warrant immediate medical attention. Severe or persistent abdominal pain, especially if radiating to the back and accompanied by nausea or vomiting, may indicate acute pancreatitis—a serious adverse effect requiring emergency evaluation. Similarly, symptoms of gallbladder disease (right upper quadrant pain, fever, jaundice) should prompt urgent assessment, as cholelithiasis risk increases with rapid weight loss.
Patients should contact their provider if they experience signs of hypoglycemia (confusion, sweating, tremor, rapid heartbeat), particularly if taking tirzepatide concurrently with insulin or sulfonylureas, as dose adjustments of these medications may be necessary. Symptoms suggesting thyroid abnormalities—including a neck mass, persistent hoarseness, dysphagia, or dyspnea—require evaluation, given the medication's boxed warning regarding thyroid C-cell tumors observed in rodent studies (though human relevance remains uncertain). Any signs of severe allergic reaction (difficulty breathing, facial swelling, severe rash) constitute a medical emergency.
Patients should seek medical attention for signs of dehydration (extreme thirst, dizziness, dark urine, reduced urination) or worsening of existing gastrointestinal conditions. Additionally, patients should discuss with their provider if gastrointestinal side effects persist beyond the first few weeks at a stable dose or significantly impair quality of life, as dose modification may be appropriate. Inadequate weight loss response (less than 5% body weight reduction after 12–16 weeks at therapeutic doses) should trigger reassessment of the treatment plan.
Women of childbearing potential should notify their provider immediately if pregnancy is suspected, as tirzepatide should be discontinued when pregnancy is recognized. Women planning pregnancy should discuss discontinuation timing with their healthcare provider, typically at least one month before planned conception based on the medication's half-life. Women using oral contraceptives should use a non-oral method or add a backup method for 4 weeks after starting tirzepatide and for 4 weeks after each dose increase. Regular monitoring of weight, blood pressure, and metabolic parameters helps optimize treatment outcomes and identify any concerns requiring intervention.
No, FDA guidelines do not specify a particular time of day for tirzepatide injection, and clinical trials showed effectiveness regardless of timing. The medication's five-day half-life maintains steady levels throughout the week, making consistency with your chosen day more important than the specific hour.
While no research definitively proves timing affects side effects, some clinicians suggest evening administration for patients experiencing nausea, allowing them to sleep through the period when gastrointestinal effects may be most noticeable. Individual preference and consistency matter most.
If fewer than four days have passed since your missed dose, inject as soon as possible and resume your regular schedule. If more than four days have passed, skip the missed dose and take your next injection on the regularly scheduled day—never double doses.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.