LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

When is the best time to start tirzepatide? This question is increasingly relevant as tirzepatide (Mounjaro, Zepbound) gains prominence in managing type 2 diabetes and obesity. As the first FDA-approved dual GIP/GLP-1 receptor agonist, tirzepatide offers substantial glycemic control and weight reduction. Optimal timing depends on FDA-approved indications, clinical criteria including baseline HbA1c and comorbidities, patient readiness for lifestyle modification, and practical considerations such as managing gastrointestinal side effects. This article examines evidence-based guidance on when to initiate tirzepatide therapy for maximum benefit and safety.
Quick Answer: The best time to start tirzepatide is when patients meet FDA criteria (type 2 diabetes requiring glycemic control or obesity/overweight with comorbidities), have inadequate response to lifestyle modification or current therapy, and can commit to weekly injections with appropriate monitoring.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide represents the first dual incretin receptor agonist available in clinical practice.
The medication works through a unique dual mechanism of action. As a GIP receptor agonist, tirzepatide enhances insulin secretion and may improve insulin sensitivity. Simultaneously, its GLP-1 receptor agonist activity stimulates glucose-dependent insulin release, suppresses glucose-dependent glucagon secretion, slows gastric emptying, and promotes satiety through central appetite regulation. In clinical trials, this dual action has demonstrated greater glycemic control and weight reduction compared to specific selective GLP-1 receptor agonists such as semaglutide 1 mg in the SURPASS-2 trial.
Tirzepatide is administered as a once-weekly subcutaneous injection, available in escalating doses from 2.5 mg to 15 mg. The medication undergoes proteolytic degradation with minimal renal clearance, with a half-life of approximately five days, allowing for convenient weekly dosing. The glucose-dependent mechanism of insulin secretion reduces the risk of hypoglycemia when used as monotherapy or with medications that do not independently cause low blood sugar.
Importantly, tirzepatide should not be coadministered with other GLP-1 receptor agonists. Understanding tirzepatide's pharmacology is essential for clinicians considering when to initiate therapy, as its mechanism informs patient selection, timing decisions, and expectations for therapeutic outcomes in both diabetes management and weight reduction.
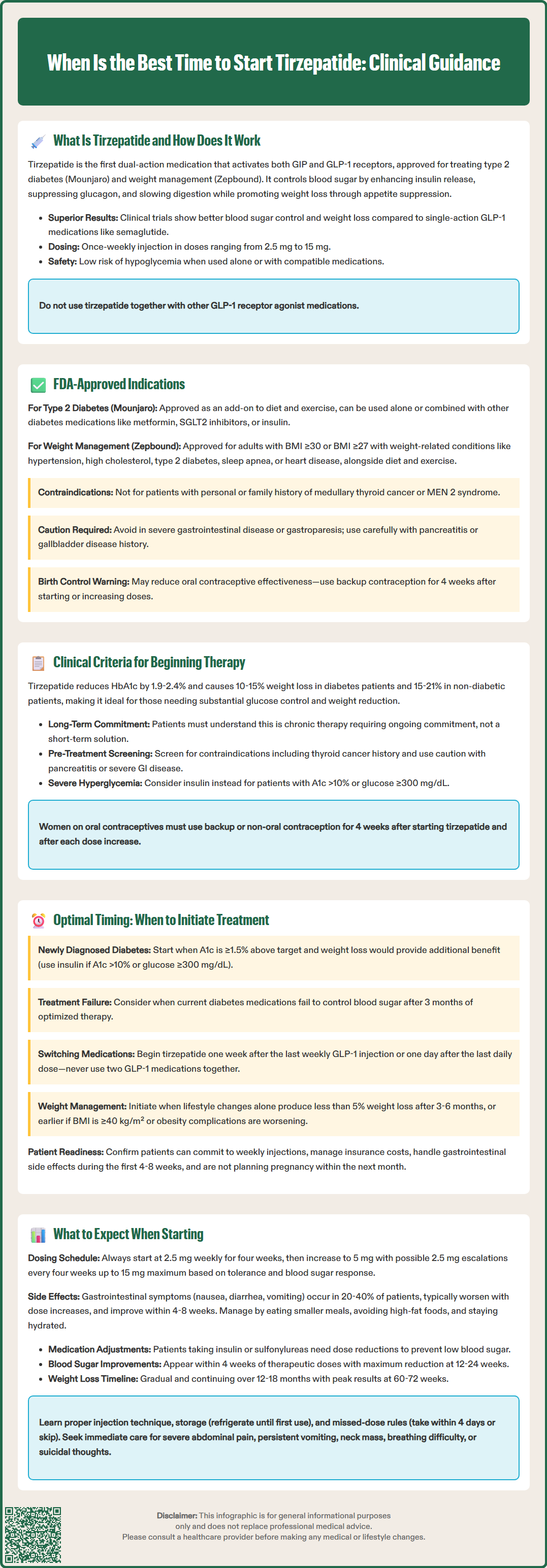
The FDA has approved tirzepatide for two distinct indications, each with specific criteria that guide the appropriate timing for treatment initiation. For type 2 diabetes mellitus, tirzepatide (Mounjaro) received FDA approval in May 2022 as an adjunct to diet and exercise to improve glycemic control in adults. The approval does not restrict tirzepatide to any particular line of therapy, meaning it can be used as monotherapy or in combination with other antidiabetic medications, including metformin, sulfonylureas, sodium-glucose cotransporter-2 (SGLT2) inhibitors, and insulin.
For chronic weight management, tirzepatide (Zepbound) gained FDA approval in November 2023 for adults with obesity (body mass index [BMI] ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbid condition. Qualifying comorbidities include hypertension, dyslipidemia, type 2 diabetes, obstructive sleep apnea, and cardiovascular disease. This indication requires that tirzepatide be used alongside a reduced-calorie diet and increased physical activity.
Importantly, tirzepatide is not approved for type 1 diabetes, diabetic ketoacidosis, or for use in patients under 18 years of age. The FDA label includes a boxed warning regarding thyroid C-cell tumors observed in rodent studies, contraindicating its use in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Routine calcitonin or thyroid ultrasound screening is not recommended by the FDA label.
Additional label warnings that may impact initiation decisions include caution in patients with severe gastrointestinal disease or gastroparesis (not recommended), history of pancreatitis, and gallbladder disease. Women using oral contraceptives should be advised about potential reduced efficacy after tirzepatide initiation or dose escalation.
These FDA-approved indications establish the regulatory framework for when tirzepatide therapy can be appropriately initiated, though clinical judgment and individual patient factors ultimately determine optimal timing within these parameters.
Beyond FDA indications, several clinical criteria should be evaluated when considering tirzepatide initiation. For patients with type 2 diabetes, the American Diabetes Association (ADA) Standards of Care emphasize individualized glycemic targets and treatment selection based on patient-specific factors including baseline hemoglobin A1c (HbA1c), presence of atherosclerotic cardiovascular disease (ASCVD), heart failure, or chronic kidney disease, hypoglycemia risk, weight considerations, and patient preferences.
Tirzepatide is particularly appropriate for patients requiring substantial HbA1c reduction, as clinical trials demonstrated reductions of 1.9% to 2.4% from baseline. For patients with established ASCVD or multiple cardiovascular risk factors, the ADA currently prioritizes GLP-1 receptor agonists with proven cardiovascular benefit and/or SGLT2 inhibitors. While tirzepatide's cardiovascular outcomes trial is ongoing, it may be considered based on individual patient factors. Additionally, patients with type 2 diabetes who would benefit from weight loss represent ideal candidates, as tirzepatide produces weight reductions of approximately 10-15% of body weight in patients with diabetes (SURMOUNT-2) and 15-21% in patients without diabetes (SURMOUNT-1).
For weight management candidates, comprehensive evaluation should include assessment of previous weight loss attempts, evaluation for secondary causes of obesity (hypothyroidism, Cushing's syndrome, medication-induced weight gain), screening for eating disorders, and discussion of realistic expectations and long-term commitment to therapy. Patients should understand that tirzepatide is intended as chronic therapy, not a short-term intervention.
Clinicians must screen for contraindications before initiating therapy, which include personal or family history of medullary thyroid carcinoma or MEN 2, and hypersensitivity to tirzepatide. Caution is warranted in patients with history of pancreatitis, severe gastrointestinal disease, or gastroparesis. No dose adjustment is required for renal impairment, including end-stage renal disease, though monitoring is recommended if significant gastrointestinal adverse events occur. Baseline laboratory evaluation should include HbA1c (for diabetes patients), comprehensive metabolic panel, lipid panel, and thyroid function tests if clinically indicated.
Patients should be counseled not to combine tirzepatide with other GLP-1 receptor agonists. Women using oral contraceptives should use non-oral or backup contraception for 4 weeks after initiation and each dose escalation due to potential reduced efficacy. For patients with severe hyperglycemia (A1c >10% or glucose ≥300 mg/dL) or catabolic symptoms, insulin initiation may be more appropriate per ADA guidelines.
Determining the optimal timing for tirzepatide initiation requires integration of clinical guidelines, patient readiness, and practical considerations. For newly diagnosed type 2 diabetes patients, current ADA guidelines support initial combination therapy when A1c is ≥1.5% above target. Tirzepatide may be considered in this context, particularly when weight loss would provide additional benefit. However, for patients with catabolic symptoms, A1c >10%, or glucose ≥300 mg/dL, insulin initiation is typically recommended per ADA guidelines.
For patients already on other diabetes medications with inadequate glycemic control (HbA1c above individualized target despite 3 months of optimized therapy), tirzepatide represents an appropriate intensification option. The medication can be added to existing regimens or substituted for other injectable therapies. When patients are on multiple oral agents with suboptimal control and significant treatment burden, transitioning to tirzepatide monotherapy or simplified combination therapy may improve both efficacy and adherence.
When switching from another GLP-1 receptor agonist, tirzepatide should be initiated approximately one week after the last dose of a weekly GLP-1 RA, or the day after the last dose of a daily GLP-1 RA. Coadministration with other GLP-1 RAs should be avoided.
In weight management, the best time to start tirzepatide is when patients have demonstrated commitment to lifestyle modification but have not achieved adequate weight loss (generally defined as <5% body weight reduction after 3-6 months of intensive lifestyle intervention), or when obesity-related comorbidities require more aggressive intervention. Earlier initiation may be warranted in patients with severe obesity (BMI ≥40 kg/m²) or those with rapidly progressive obesity-related complications.
Practical timing considerations include ensuring patients can commit to weekly injections and follow-up appointments, verifying insurance coverage or discussing out-of-pocket costs before initiation, scheduling initiation when patients can manage potential gastrointestinal side effects (avoiding major life events, travel, or work commitments in the first 4-8 weeks), and confirming patients are not planning pregnancy in the near term. Women should discontinue tirzepatide when pregnancy is recognized and consider stopping at least one month before planned conception. Seasonal considerations may also be relevant, as some patients prefer avoiding initiation during holidays when dietary patterns are disrupted.
Patients beginning tirzepatide should receive comprehensive counseling about the initiation process, expected timeline for benefits, and potential adverse effects. Treatment always begins with the 2.5 mg dose administered once weekly for four weeks, serving as a tolerability-building dose rather than a therapeutic dose. After this initial period, the dose is increased to 5 mg weekly, with subsequent escalations by 2.5 mg increments every four weeks as tolerated, up to a maximum of 15 mg weekly based on glycemic response and tolerability. Dose escalation can be delayed beyond 4 weeks if gastrointestinal effects persist.
Gastrointestinal side effects represent the most common adverse events, occurring in 20% to 40% of patients. These include nausea, diarrhea, decreased appetite, vomiting, constipation, dyspepsia, and abdominal pain. Symptoms typically emerge or worsen with dose escalation and generally improve over 4 to 8 weeks as tolerance develops. Patients should be advised to eat smaller, more frequent meals, avoid high-fat foods, stay well-hydrated, and report severe or persistent symptoms. Antiemetic medications may be prescribed if needed, though symptoms often resolve without intervention.
When initiating or escalating tirzepatide in patients taking insulin or sulfonylureas, dose reductions of these medications should be considered to mitigate hypoglycemia risk. Patients with pre-existing diabetic retinopathy should be monitored for worsening retinopathy with rapid glycemic improvement.
Glycemic improvements typically become apparent within 4 weeks of reaching therapeutic doses (5 mg or higher), with maximal HbA1c reduction observed at 12 to 24 weeks. Weight loss begins within the first month but continues progressively over 12 to 18 months, with most patients achieving maximum weight reduction between 60 and 72 weeks of therapy. Patients should be counseled that weight loss is gradual and sustained adherence is essential.
Patients should receive clear instructions on injection technique, proper storage (refrigeration until first use, with specific room-temperature allowances per label), and missed-dose management (take within 4 days of scheduled dose; otherwise skip and resume at next scheduled dose). They should be educated on recognition of hypoglycemia symptoms and when to seek medical attention, including severe abdominal pain, persistent vomiting, signs of pancreatitis, symptoms of thyroid tumors (neck mass, dysphagia, dyspnea), or suicidal thoughts or behavior (particularly for patients using tirzepatide for weight management).
Clinicians should establish a monitoring schedule including follow-up at 4 to 8 weeks after initiation to assess tolerability and side effects, HbA1c measurement every 3 months until stable, then every 6 months, regular weight and blood pressure monitoring, periodic renal function and lipid panel assessment, and evaluation for signs of pancreatitis, gallbladder disease, or other serious adverse events.
Yes, tirzepatide is FDA-approved without restriction to any particular line of therapy and can be used as monotherapy or in combination with other diabetes medications. The ADA supports initial combination therapy when HbA1c is ≥1.5% above target, making tirzepatide appropriate for newly diagnosed patients, particularly when weight loss would provide additional benefit.
Glycemic improvements typically become apparent within 4 weeks of reaching therapeutic doses (5 mg or higher), with maximal HbA1c reduction at 12-24 weeks. Weight loss begins within the first month but continues progressively over 12-18 months, with most patients achieving maximum weight reduction between 60-72 weeks of therapy.
Tirzepatide should not be combined with other GLP-1 receptor agonists, but it can be used with most other diabetes medications. When initiating tirzepatide in patients taking insulin or sulfonylureas, dose reductions of these medications should be considered to reduce hypoglycemia risk, though this decision should be made in consultation with your healthcare provider.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.