LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Blood in stool while taking tirzepatide (Mounjaro, Zepbound) is not a recognized side effect in FDA prescribing information, but warrants immediate medical evaluation. Tirzepatide, a dual GIP and GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management, commonly causes gastrointestinal effects including nausea, diarrhea, and constipation. While the medication does not directly cause gastrointestinal bleeding, its effects on bowel function may indirectly contribute to conditions like hemorrhoids or anal fissures that produce rectal bleeding. Any patient experiencing blood in stool should seek prompt clinical assessment to determine the underlying cause and ensure appropriate management.
Quick Answer: Blood in stool is not a recognized side effect of tirzepatide, but the medication's gastrointestinal effects may indirectly contribute to conditions causing rectal bleeding that require medical evaluation.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). While gastrointestinal side effects are common with this medication class, blood in the stool is not listed as a typical adverse effect in the FDA prescribing information for either Mounjaro or Zepbound.
Patients may notice blood in their stool as bright red streaks, dark tarry stools (melena), or blood mixed with diarrhea. The presence of blood always warrants clinical evaluation, as it can indicate various conditions ranging from benign hemorrhoids to more serious gastrointestinal pathology. It's worth noting that some substances like iron supplements or bismuth subsalicylate (Pepto-Bismol) can darken stool without causing bleeding.
While current evidence does not establish a direct causal relationship between tirzepatide and gastrointestinal bleeding, tirzepatide's known gastrointestinal effects—including nausea, diarrhea, vomiting, and constipation—may indirectly contribute to conditions that cause rectal bleeding. For example, severe diarrhea can lead to anal fissures, while constipation may cause hemorrhoidal bleeding from straining. The medication's effect on gastric emptying and bowel motility creates a physiological environment where pre-existing gastrointestinal conditions might become symptomatic.
It is essential to distinguish between medication-related gastrointestinal symptoms and bleeding that represents underlying pathology requiring investigation. Any patient experiencing blood in their stool while taking tirzepatide should seek prompt medical evaluation to determine the cause and ensure appropriate management. Clinicians may recommend temporarily holding tirzepatide during acute significant gastrointestinal bleeding or severe symptoms pending evaluation.
Tirzepatide's mechanism of action directly influences gastrointestinal physiology through its dual agonism of GIP and GLP-1 receptors. GLP-1 receptor activation significantly delays gastric emptying, may modestly reduce gastric acid secretion, and decreases gastrointestinal motility. These effects contribute to the medication's glucose-lowering and weight-reduction benefits by promoting satiety and reducing caloric intake, but they also account for the high incidence of gastrointestinal adverse effects.
In the SURPASS clinical trial program, gastrointestinal side effects were the most commonly reported adverse events. According to the FDA prescribing information, nausea occurred in 12-24% of patients, diarrhea in 11-17%, vomiting in 5-10%, and constipation in 5-7%, with rates varying by dose. These effects are typically most pronounced during dose initiation and escalation, generally improving over time as physiological adaptation occurs. The delayed gastric emptying can lead to feelings of fullness, bloating, and altered bowel patterns.
The medication's impact on bowel function may potentially affect pre-existing gastrointestinal conditions, though evidence is limited. Patients with inflammatory bowel disease, diverticular disease, or hemorrhoids should be monitored closely for symptom changes. Severe or persistent diarrhea can cause dehydration, electrolyte imbalances, and mechanical trauma to the anal canal and rectal mucosa. Conversely, constipation may lead to hard stools, straining, and hemorrhoidal engorgement.
While tirzepatide has not been shown to directly cause gastrointestinal ulceration in clinical trials, its effects on motility and bowel habits may create conditions where bleeding from benign sources becomes more likely. The FDA prescribing information cautions against use in patients with severe gastrointestinal disease, including severe gastroparesis. Understanding this relationship helps clinicians counsel patients appropriately and distinguish between expected medication effects and symptoms requiring further investigation.
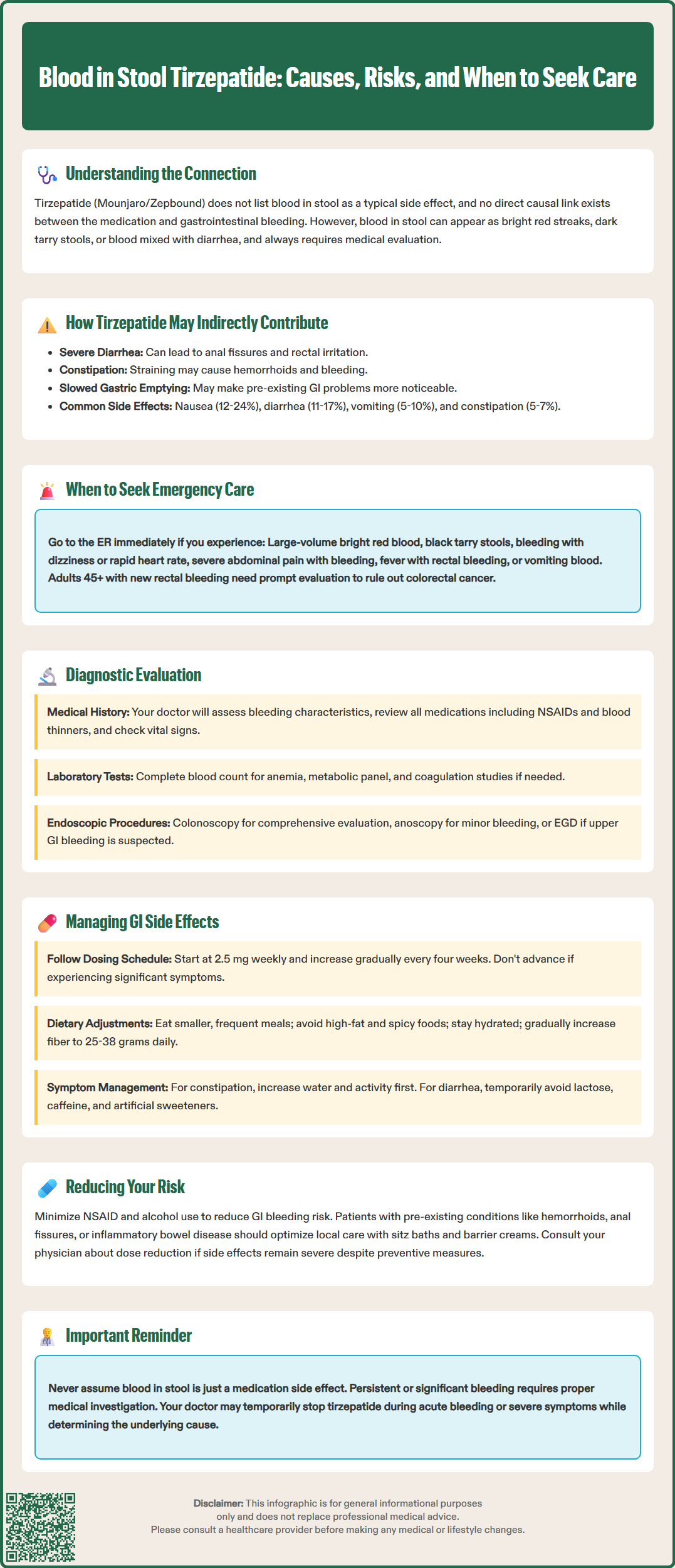
Certain presentations of gastrointestinal bleeding constitute medical emergencies requiring immediate evaluation in an emergency department. Patients taking tirzepatide should call 911 or seek emergency care immediately if they experience large-volume bright red blood per rectum, passage of maroon or black tarry stools (melena), or blood in stool accompanied by hemodynamic instability. Warning signs of significant blood loss include dizziness, lightheadedness, syncope, rapid heart rate, confusion, pale or clammy skin, and shortness of breath.
Additional red flag symptoms that warrant emergency assessment include severe abdominal pain, particularly if localized and persistent, fever accompanying rectal bleeding, and vomiting blood (hematemesis) or coffee-ground material. Patients with known liver disease, history of gastrointestinal bleeding, or those taking anticoagulant or antiplatelet medications face higher risk for significant bleeding complications and should have a lower threshold for seeking emergency care. Importantly, patients should not discontinue anticoagulants or antiplatelets without medical guidance, even with bleeding.
Even without hemodynamic compromise, certain patterns of bleeding require prompt same-day evaluation. Persistent bleeding over multiple bowel movements, bleeding that increases in volume rather than resolving, or new-onset bleeding in patients aged 45 or older should trigger urgent medical assessment. Current US guidelines, including those from the US Preventive Services Task Force and American College of Gastroenterology, emphasize that new rectal bleeding in adults 45 and older requires investigation to exclude colorectal malignancy, regardless of presumed benign causes.
Patients should not assume that blood in stool is simply a side effect of tirzepatide. While the medication may contribute to conditions causing minor bleeding, it does not explain significant or persistent hemorrhage. Healthcare providers should maintain a high index of suspicion and pursue appropriate diagnostic evaluation rather than attributing bleeding solely to medication effects. Clear patient education about warning signs and when to seek care is essential for safety.
The diagnostic approach to gastrointestinal bleeding in patients taking tirzepatide begins with a thorough clinical history and physical examination. Clinicians should characterize the bleeding pattern: color (bright red versus dark), volume, frequency, relationship to bowel movements, and associated symptoms. A complete medication review is essential, including over-the-counter NSAIDs, anticoagulants, and antiplatelet agents that increase bleeding risk. Past medical history should address previous gastrointestinal conditions, bleeding episodes, liver disease, and colorectal cancer screening status.
Physical examination includes vital signs assessment for hemodynamic stability, abdominal examination for tenderness or masses, and digital rectal examination to identify anorectal pathology and characterize stool appearance. Laboratory evaluation typically includes complete blood count to assess for anemia and determine acuity of blood loss, comprehensive metabolic panel to evaluate renal function and electrolytes (particularly relevant given tirzepatide's gastrointestinal effects), and coagulation studies if bleeding disorder is suspected. Note that fecal occult blood testing is unnecessary when bleeding is visible.
For patients with minor, self-limited bright red blood suggesting anorectal source, anoscopy or flexible sigmoidoscopy may suffice to identify hemorrhoids, fissures, or distal inflammation. However, colonoscopy remains the gold standard for comprehensive evaluation, particularly in patients 45 and older or those with alarm features. The American Society for Gastrointestinal Endoscopy and American College of Gastroenterology provide evidence-based algorithms for the endoscopic evaluation of lower gastrointestinal bleeding.
Upper gastrointestinal bleeding, suggested by melena or hematemesis, requires esophagogastroduodenoscopy (EGD). In cases of obscure bleeding where upper and lower endoscopy are unrevealing, additional modalities including capsule endoscopy, CT enterography, or tagged red blood cell scan may be indicated per ACG small-bowel bleeding guidelines. The diagnostic approach should be individualized based on bleeding severity, patient age, risk factors, and clinical presentation. Decisions about temporarily holding tirzepatide during acute significant gastrointestinal illness should be made based on clinical judgment and the severity of symptoms.
Proactive management of tirzepatide's gastrointestinal effects can reduce the risk of complications that might lead to rectal bleeding. The FDA-approved dosing schedule includes gradual titration specifically to improve gastrointestinal tolerability. For type 2 diabetes, tirzepatide starts at 2.5 mg subcutaneously once weekly for four weeks, then increases by 2.5 mg increments every four weeks as tolerated, per the Mounjaro prescribing information. Patients should not advance doses if experiencing significant gastrointestinal symptoms.
Dietary modifications can substantially improve tolerability. Patients should eat smaller, more frequent meals rather than large portions, avoid high-fat and spicy foods that delay gastric emptying further, and maintain adequate hydration, particularly during diarrheal episodes. Increasing dietary fiber gradually can help regulate bowel movements, though excessive fiber may worsen bloating. The Dietary Guidelines for Americans and Academy of Nutrition and Dietetics recommend approximately 25 grams of fiber daily for women and 38 grams daily for men, with adequate fluid intake.
For patients experiencing constipation, a stepwise approach includes increased water intake, physical activity, and dietary fiber. If insufficient, osmotic laxatives such as polyethylene glycol are generally safe and effective as first-line agents per AGA-ACG guidelines. Stimulant laxatives may be used judiciously under medical supervision when needed. Patients with diarrhea may benefit from temporary dietary restriction of lactose, caffeine, and artificial sweeteners, with consideration of loperamide for symptomatic relief if infectious causes are excluded.
Patients with pre-existing hemorrhoids or anal fissures should optimize local care including warm sitz baths, topical barrier creams, and avoidance of straining. Those with inflammatory bowel disease or other chronic gastrointestinal conditions require close monitoring and may need specialist gastroenterology input before initiating or continuing tirzepatide. Minimizing NSAID use and alcohol consumption can reduce gastrointestinal bleeding risk. If gastrointestinal side effects are severe or persistent despite conservative measures, dose reduction or medication discontinuation should be considered in consultation with the prescribing physician. Regular follow-up allows early identification of complications and adjustment of management strategies to optimize both therapeutic benefit and patient safety.
No, blood in stool is not listed as a typical adverse effect in FDA prescribing information for tirzepatide. However, the medication's gastrointestinal effects like diarrhea and constipation may indirectly contribute to conditions such as hemorrhoids or anal fissures that cause rectal bleeding.
Seek emergency care immediately for large-volume bright red blood, black tarry stools, bleeding with dizziness or rapid heart rate, severe abdominal pain, fever, or vomiting blood. Patients taking anticoagulants or with liver disease should have a lower threshold for emergency evaluation.
Follow the FDA-approved gradual dose titration schedule, eat smaller frequent meals, avoid high-fat and spicy foods, maintain adequate hydration, and increase dietary fiber gradually. If symptoms persist despite these measures, consult your physician about dose adjustment or medication discontinuation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.