LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro, Zepbound) is an FDA-approved dual GIP and GLP-1 receptor agonist used for type 2 diabetes and chronic weight management. While highly effective, many patients wonder: does tirzepatide cause loose stools? The answer is yes—diarrhea and loose stools are among the most common side effects, affecting 13-24% of patients in clinical trials. These gastrointestinal symptoms result from tirzepatide's mechanism of slowing gastric emptying and affecting intestinal motility. Understanding why these effects occur, how to manage them, and when to seek medical attention helps patients navigate treatment successfully while maximizing therapeutic benefits.
Quick Answer: Tirzepatide commonly causes loose stools and diarrhea in 13-24% of patients, typically mild to moderate and resolving within weeks of treatment initiation or dose escalation.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. This medication works by mimicking naturally occurring incretin hormones that regulate blood sugar levels, slow gastric emptying, and reduce appetite. While these mechanisms contribute to its therapeutic benefits, they also explain why gastrointestinal side effects are among the most commonly reported adverse reactions.
The pharmacological action of tirzepatide directly affects the digestive system. By activating GLP-1 receptors in the gastrointestinal tract, the medication slows the movement of food from the stomach into the small intestine. This delayed gastric emptying can alter normal bowel patterns and digestive processes. Additionally, GLP-1 receptor activation influences intestinal motility and fluid secretion, which may contribute to changes in stool consistency and frequency, including diarrhea (defined as three or more loose or watery stools per day).
Clinical trials have consistently demonstrated that gastrointestinal adverse effects are the most frequent side effects associated with tirzepatide therapy. These effects typically occur early in treatment or following dose escalation and often diminish over time as the body adapts to the medication. According to the FDA prescribing information, tirzepatide is not recommended for patients with severe gastrointestinal disease, such as severe gastroparesis. Additionally, dehydration from gastrointestinal side effects may increase the risk of acute kidney injury, and gallbladder disease has been reported with incretin-based therapies.
Understanding the relationship between tirzepatide's mechanism of action and digestive symptoms helps patients and healthcare providers anticipate, recognize, and appropriately manage these common side effects. The gastrointestinal tolerability profile is an important consideration when initiating therapy and counseling patients about what to expect during treatment.
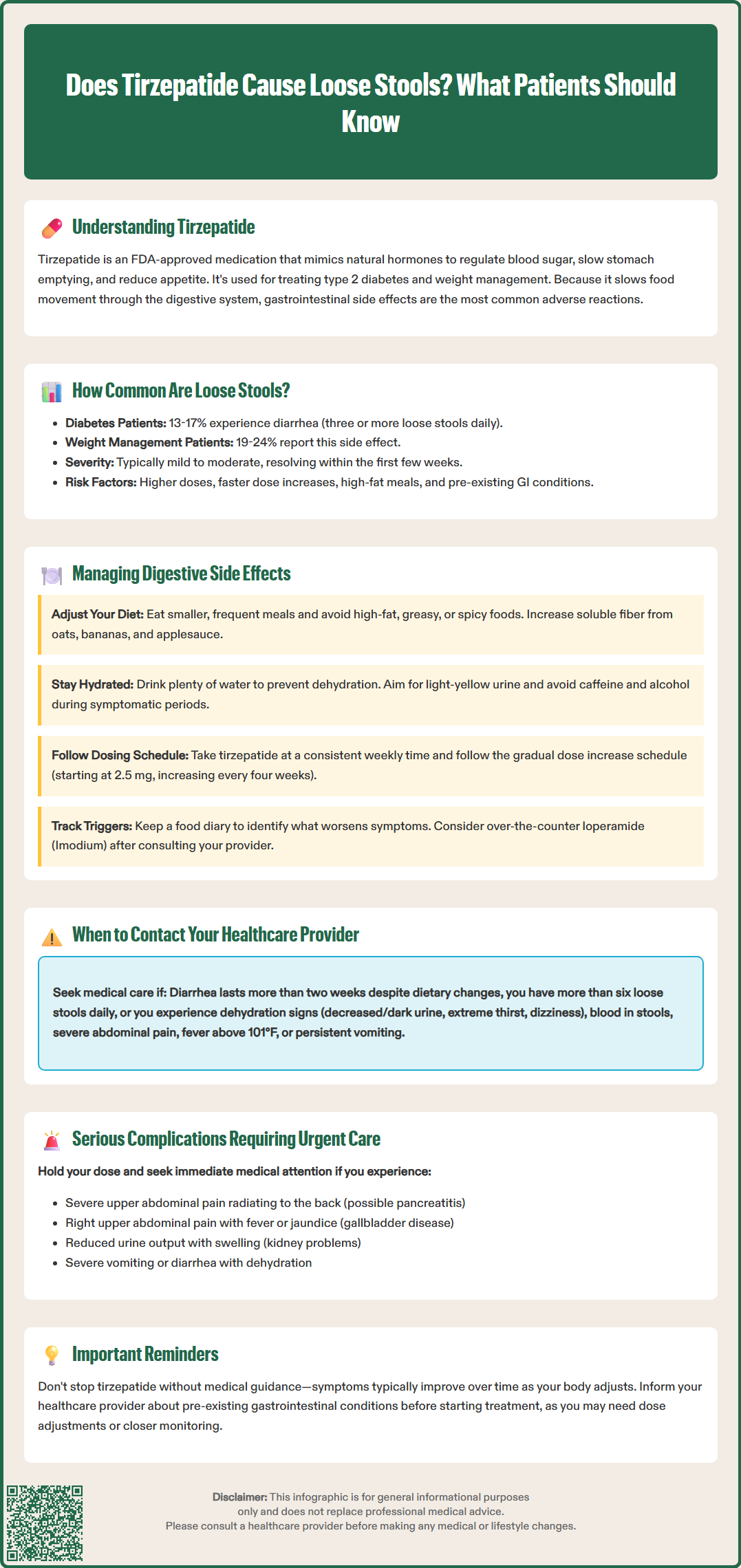
Yes, tirzepatide can cause loose stools and diarrhea, and these are recognized adverse effects in the FDA-approved prescribing information. In the pivotal SURPASS clinical trial program for type 2 diabetes, diarrhea was reported in 13-17% of patients receiving tirzepatide, with rates varying by dose. The incidence increased with higher doses, ranging from 5 mg (13%) to 15 mg (17%) weekly. In the SURMOUNT trials evaluating tirzepatide for weight management, diarrhea occurred in 19-24% of participants across doses, making it one of the most common gastrointestinal complaints alongside nausea and vomiting.
The severity of loose stools associated with tirzepatide is typically mild to moderate, and most cases resolve spontaneously within the first few weeks of treatment. The highest risk period occurs during treatment initiation and when doses are increased. The FDA-approved dosing schedule includes a gradual titration strategy specifically designed to minimize gastrointestinal side effects, starting at 2.5 mg weekly and increasing every four weeks as tolerated.
Several factors may influence an individual's likelihood of experiencing loose stools on tirzepatide. These include the starting dose, rate of dose escalation, dietary habits (particularly high-fat meals), concurrent medications, and individual gastrointestinal sensitivity. Patients with pre-existing gastrointestinal conditions may be more susceptible to digestive side effects. It is important to note that while diarrhea is common, severe or persistent diarrhea is less frequent and warrants medical evaluation. The American Diabetes Association Standards of Care emphasize the importance of patient education regarding expected side effects to improve medication adherence and treatment outcomes.
Effective management of loose stools and diarrhea while taking tirzepatide involves both preventive strategies and symptomatic treatment approaches. Dietary modifications represent the first-line approach to minimizing gastrointestinal disturbances. Patients should consider eating smaller, more frequent meals rather than large portions, which can overwhelm the already-slowed digestive system. Reducing intake of high-fat, greasy, or spicy foods may decrease the likelihood of loose stools, as these foods can exacerbate gastrointestinal symptoms. Increasing soluble fiber intake through foods like oats, bananas, and applesauce can help firm stools naturally.
Hydration is critically important when experiencing diarrhea to prevent dehydration and electrolyte imbalances. Patients should maintain adequate fluid intake to produce light-yellow urine, though specific fluid needs vary by individual. Those with heart failure or kidney disease should follow their healthcare provider's guidance on fluid intake. Oral rehydration solutions containing electrolytes may be beneficial for those with persistent symptoms. Avoiding caffeine and alcohol, which can worsen diarrhea and dehydration, is advisable during symptomatic periods.
Practical management strategies include:
Taking tirzepatide at a consistent time each week, preferably when you can rest if side effects occur
Following the prescribed dose escalation schedule without rushing increases
Keeping a food and symptom diary to identify potential dietary triggers
Using over-the-counter antidiarrheal medications like loperamide (Imodium) for occasional relief, after consulting your healthcare provider (avoid if you have fever or bloody stools, and do not exceed recommended dosing)
Considering probiotics, though evidence for their effectiveness specifically with GLP-1 receptor agonist-related diarrhea remains limited
Patients should not discontinue tirzepatide without medical guidance, as gastrointestinal symptoms often improve with continued use. If symptoms are severe or significantly impact quality of life, healthcare providers may recommend temporarily maintaining the current dose longer before escalating, reducing to the previous tolerated dose, or occasionally holding a dose. Communication with your healthcare team about symptom severity and impact on daily functioning is essential for optimizing your treatment plan.
While mild to moderate loose stools are expected side effects of tirzepatide that often resolve with time, certain symptoms warrant prompt medical evaluation. Patients should contact their healthcare provider if diarrhea persists beyond two weeks despite dietary modifications and supportive care, as prolonged symptoms may indicate a need for dose adjustment or additional evaluation. Severe diarrhea, defined as more than six loose stools per day or diarrhea that significantly interferes with daily activities, requires medical assessment.
Contact your healthcare provider immediately if you experience:
Signs of dehydration, including decreased urination, dark urine, extreme thirst, dizziness, or lightheadedness
Blood in stools or black, tarry stools
Severe abdominal pain or cramping that doesn't resolve
Fever above 101°F (38.3°C) accompanying diarrhea
Unintentional weight loss beyond expected therapeutic effects
Persistent nausea and vomiting preventing adequate fluid intake
Symptoms of pancreatitis, including severe upper abdominal pain radiating to the back
Signs of gallbladder disease, such as right upper quadrant pain, fever, or yellowing of skin/eyes
Symptoms of kidney problems, including reduced urine output, swelling, or confusion
These warning signs may indicate complications requiring urgent evaluation. In cases of severe or persistent vomiting or diarrhea with signs of dehydration, or suspected pancreatitis, patients should hold their tirzepatide dose and seek urgent medical care. The FDA prescribing information for tirzepatide includes warnings about acute pancreatitis, gallbladder disease, and acute kidney injury risk with dehydration.
Patients with pre-existing gastrointestinal disorders, including inflammatory bowel disease, gastroparesis, or chronic diarrhea conditions, should discuss these conditions with their healthcare provider before starting tirzepatide. Dose adjustments, alternative medications, or additional monitoring may be appropriate. Regular follow-up appointments allow healthcare providers to assess treatment tolerance, adjust therapy as needed, and ensure that gastrointestinal symptoms are not masking other medical conditions. Open communication about side effects supports safe, effective use of tirzepatide while maximizing its therapeutic benefits for diabetes management or weight loss.
Diarrhea occurs in 13-17% of patients taking tirzepatide for type 2 diabetes and 19-24% of those using it for weight management, with higher rates at increased doses. Most cases are mild to moderate and resolve within the first few weeks of treatment.
Yes, most cases of loose stools associated with tirzepatide resolve spontaneously as the body adapts to the medication, typically within the first few weeks of treatment or after dose increases. Symptoms often diminish with continued use and dietary modifications.
Contact your healthcare provider if diarrhea persists beyond two weeks, occurs more than six times daily, or is accompanied by signs of dehydration, bloody stools, severe abdominal pain, fever above 101°F, or inability to maintain adequate fluid intake.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.