LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro, Zepbound) is a dual GIP and GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management. While increased thirst is not listed as a direct side effect in FDA prescribing information, some patients report experiencing this symptom during treatment. Thirst may occur indirectly through gastrointestinal side effects like nausea, vomiting, or diarrhea that lead to dehydration. Understanding whether tirzepatide makes you thirsty requires examining the medication's mechanism, common adverse effects, and when thirst signals a medical concern requiring evaluation. Most cases are manageable with proper hydration strategies and monitoring.
Quick Answer: Tirzepatide does not directly cause thirst as a listed side effect, but patients may experience increased thirst indirectly through gastrointestinal side effects like nausea, vomiting, or diarrhea that lead to dehydration.
Tirzepatide (Mounjaro, Zepbound) is not officially listed as causing increased thirst as a direct side effect in the FDA prescribing information. However, some patients anecdotally report experiencing thirst while taking this medication, and there are several plausible explanations for this symptom. Understanding the relationship between tirzepatide and thirst requires examining both the medication's mechanism of action and its common side effects.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). While thirst itself is not documented as a primary adverse effect in clinical trials, the medication can indirectly lead to increased thirst through several mechanisms, particularly gastrointestinal side effects that may cause dehydration.
It is important to distinguish between mild thirst related to medication side effects and excessive thirst (polydipsia) that may signal a medical concern such as hyperglycemia. Polydipsia is a classic symptom of elevated blood glucose and should prompt blood glucose monitoring. Most patients who experience thirst on tirzepatide find it manageable and temporary, particularly during the initial weeks of treatment or after dose escalation. However, persistent or severe thirst warrants medical evaluation to rule out underlying conditions such as inadequately controlled diabetes or dehydration from gastrointestinal side effects.
Patients should maintain open communication with their healthcare providers about any new or worsening symptoms, including thirst, to ensure safe and effective treatment with tirzepatide.
Several mechanisms may explain why patients experience increased thirst while taking tirzepatide. The most common reason relates to the medication's gastrointestinal side effects, particularly nausea, vomiting, and diarrhea. According to the FDA prescribing information, nausea occurs in approximately 15-30% of patients, vomiting in 6-12%, and diarrhea in 13-24% (rates vary by dose and indication). When these symptoms are present, they can lead to fluid loss and subsequent dehydration, triggering the body's natural thirst response.
Another potential contributor is the medication's effect on blood glucose levels. Tirzepatide works by enhancing insulin secretion in a glucose-dependent manner and suppressing glucagon release, which lowers blood sugar. However, if blood glucose remains elevated despite treatment, thirst can occur due to osmotic diuresis—a process where excess glucose in the bloodstream pulls water into the urine, leading to increased urination and subsequent thirst. This is particularly relevant during the initial adjustment period or if diabetes is not yet optimally controlled.
Dehydration from gastrointestinal side effects may be compounded by reduced fluid intake, especially if patients experience nausea or reduced appetite, another common effect of tirzepatide. Some patients also anecdotally report dry mouth while taking tirzepatide, though this is not prominently featured in clinical trial data. If present, dry mouth could contribute to the sensation of thirst.
It's worth noting that while tirzepatide slows gastric emptying, which contributes to its weight loss effects by promoting satiety, there is insufficient evidence to conclude that this directly affects fluid balance or causes thirst through altered fluid absorption patterns.
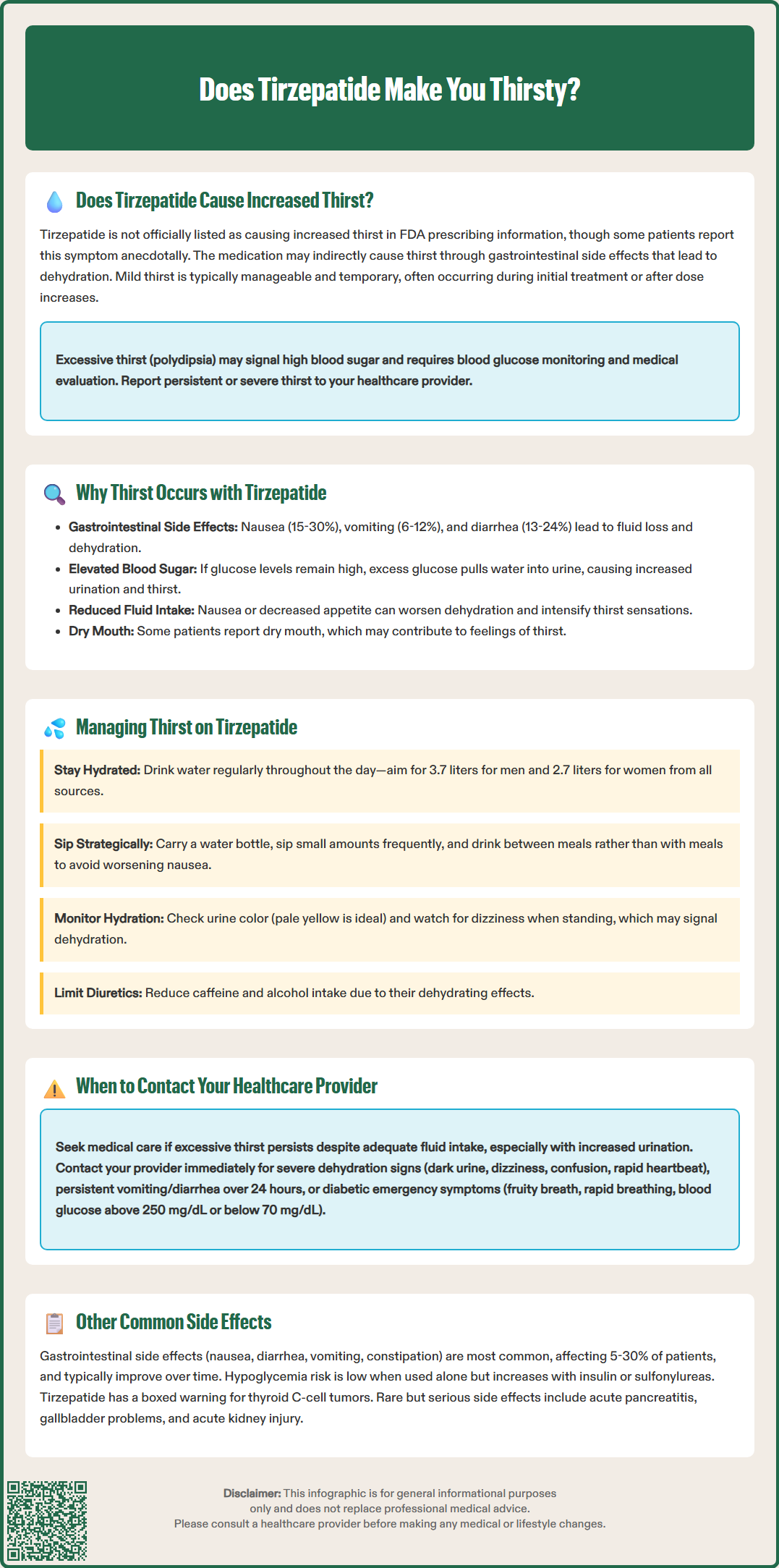
While mild thirst is generally manageable, certain warning signs indicate the need for prompt medical evaluation. Patients should contact their healthcare provider if they experience excessive thirst (polydipsia) that persists despite adequate fluid intake, as this may signal uncontrolled diabetes or other metabolic disturbances. According to the American Diabetes Association (ADA) guidelines, persistent polydipsia accompanied by increased urination (polyuria) warrants assessment of blood glucose levels and kidney function.
Contact your healthcare provider immediately if thirst is accompanied by:
Signs of severe dehydration (dark urine, dizziness, confusion, rapid heartbeat, decreased skin turgor)
Persistent vomiting or diarrhea lasting more than 24 hours
Inability to keep fluids down
Symptoms of diabetic ketoacidosis (fruity breath odor, rapid breathing, abdominal pain)
Blood glucose readings consistently above 250 mg/dL (check ketones if available)
Blood glucose readings below 70 mg/dL with symptoms of hypoglycemia
Decreased urine output despite drinking fluids
Rapid weight loss over 24-48 hours (suggesting dehydration)
While tirzepatide does not require dose adjustment based on renal function, patients experiencing severe gastrointestinal adverse reactions should be monitored for acute kidney injury, particularly if dehydration occurs. The FDA prescribing information notes limited data in patients on dialysis.
It is also important to seek medical advice if thirst develops suddenly after a dose increase or if it significantly impacts quality of life. Your healthcare provider may need to adjust your dose, evaluate for complications, or recommend additional testing such as comprehensive metabolic panel, hemoglobin A1c, or kidney function tests to ensure safe continuation of therapy.
Effective management of thirst while taking tirzepatide involves both preventive strategies and responsive measures. The cornerstone of management is maintaining adequate hydration throughout the day. Patients should aim to drink water regularly rather than waiting until they feel thirsty, as thirst is often a late indicator of dehydration. Individual hydration needs vary based on body weight, activity level, climate, and medical conditions. The National Academies of Sciences, Engineering, and Medicine suggests general adequate intake of about 3.7 liters (125 ounces) daily for men and 2.7 liters (91 ounces) for women from all beverages and foods combined, though patients with heart failure or kidney disease may have fluid restrictions.
Practical strategies to manage thirst include:
Carrying a water bottle throughout the day as a visual reminder to drink regularly
Setting hydration goals and tracking fluid intake using smartphone apps or journals
Drinking small amounts frequently rather than large volumes at once, which may worsen nausea
Consuming hydrating foods such as watermelon, cucumbers, and broths
Limiting caffeine and alcohol, which can have diuretic effects
Using appropriate oral rehydration solutions if experiencing significant gastrointestinal fluid losses (consult your healthcare provider for specific recommendations, especially with kidney disease or heart failure)
Timing fluid intake strategically can help minimize discomfort. Some patients find it helpful to drink water between meals rather than with meals, as tirzepatide slows gastric emptying and drinking large amounts with food may increase feelings of fullness or nausea. If dry mouth contributes to thirst, sugar-free gum or lozenges can stimulate saliva production.
Monitoring for signs of adequate hydration is important. Pale yellow urine generally indicates good hydration status, while dark yellow or amber urine suggests the need for increased fluid intake. Check for orthostatic symptoms (dizziness when standing) as these may indicate dehydration. Patients should also monitor their weight regularly, as sudden weight loss may indicate dehydration requiring medical attention. If gastrointestinal side effects are contributing to thirst, anti-nausea medications prescribed by your healthcare provider may help reduce fluid losses and improve overall comfort.
Beyond thirst-related concerns, tirzepatide is associated with several other side effects that patients should recognize. The most common adverse effects are gastrointestinal in nature, reflecting the medication's mechanism of action on GLP-1 and GIP receptors in the digestive system. According to FDA prescribing information, these effects are typically most pronounced during initial treatment and after dose escalations, often improving over time as the body adjusts.
Gastrointestinal side effects include:
Nausea (15-30% of patients depending on dose): Usually mild to moderate and decreasing over time
Diarrhea (13-24%): May contribute to dehydration if persistent
Vomiting (6-12%): More common at higher doses
Constipation (5-17%): Can alternate with diarrhea in some patients
Abdominal pain (6-10%): Typically mild and self-limiting
Decreased appetite: An intended effect contributing to weight loss
Hypoglycemia risk varies depending on concurrent medications. When tirzepatide is used as monotherapy or with medications that do not cause hypoglycemia (such as metformin), the risk is low. However, when combined with insulin or sulfonylureas, hypoglycemia rates increase significantly. Dose reduction of these concomitant medications may be necessary.
More serious but rare adverse effects require awareness. Tirzepatide carries a boxed warning regarding thyroid C-cell tumors based on rodent studies, though human relevance remains uncertain. The medication is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Acute pancreatitis has been reported in clinical trials, presenting with severe abdominal pain radiating to the back. Patients should discontinue tirzepatide and seek immediate medical attention if pancreatitis is suspected.
Other notable adverse effects include injection site reactions (typically mild), gallbladder problems including cholelithiasis, acute kidney injury (particularly with severe dehydration from gastrointestinal side effects), and hypersensitivity reactions including anaphylaxis and angioedema. Patients experiencing persistent or severe side effects should consult their healthcare provider, who may adjust the dose, slow the titration schedule, or consider alternative treatments based on individual tolerance and therapeutic goals.
Increased thirst is not officially listed as a direct side effect in FDA prescribing information, but some patients report it anecdotally. Thirst typically occurs indirectly through gastrointestinal side effects like nausea, vomiting, or diarrhea that cause dehydration.
Contact your healthcare provider immediately if thirst is accompanied by signs of severe dehydration, persistent vomiting or diarrhea lasting more than 24 hours, inability to keep fluids down, blood glucose consistently above 250 mg/dL, or symptoms of diabetic ketoacidosis.
Maintain adequate hydration by drinking water regularly throughout the day, carrying a water bottle as a reminder, consuming hydrating foods, and limiting caffeine and alcohol. If gastrointestinal side effects contribute to thirst, anti-nausea medications prescribed by your healthcare provider may help.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.