LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Can you take weight loss injections forever? This question reflects growing interest in GLP-1 receptor agonists like semaglutide (Wegovy) and tirzepatide (Zepbound) for chronic weight management. These FDA-approved medications are designed for long-term use as part of comprehensive obesity treatment. Obesity is now recognized as a chronic, relapsing disease requiring ongoing management—similar to diabetes or hypertension. While these injections can be continued indefinitely when benefits outweigh risks, treatment duration should be individualized based on response, tolerability, and patient goals. Understanding the implications of long-term therapy, including safety considerations and what happens if treatment stops, is essential for informed decision-making with your healthcare provider.
Quick Answer: Weight loss injections like semaglutide and tirzepatide are intended for chronic use and can be taken long-term when benefits outweigh risks, though treatment duration should be individualized with your physician.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections primarily refer to incretin-based agents, including glucagon-like peptide-1 (GLP-1) receptor agonists (e.g., semaglutide) and the dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 receptor agonist tirzepatide. These medications were originally developed for type 2 diabetes management but are now FDA-approved as an adjunct to reduced-calorie diet and increased physical activity for chronic weight management. The most commonly prescribed agents include semaglutide (marketed as Wegovy for weight management and Ozempic for diabetes) and tirzepatide (Zepbound for weight management, Mounjaro for diabetes).
These medications work by mimicking naturally occurring incretin hormones that regulate appetite and glucose metabolism. They bind to receptors in multiple tissues throughout the body, including the brain, pancreas, and gastrointestinal tract. In the hypothalamus, they reduce appetite and increase feelings of fullness (satiety). In the stomach, they slow gastric emptying, which prolongs the sensation of fullness after meals. Additionally, these medications enhance insulin secretion in response to food intake and suppress glucagon release, contributing to improved glycemic control.
These injections are administered subcutaneously, typically once weekly for most formulations, though some (like liraglutide) require daily dosing. The FDA has approved these medications for chronic weight management in adults with obesity (body mass index ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity such as hypertension, type 2 diabetes, or dyslipidemia. Semaglutide (Wegovy) is also approved for adolescents aged 12 and older with obesity. Clinical trials have demonstrated average weight loss of approximately 15% with semaglutide 2.4 mg and up to 22% with tirzepatide 15 mg, though individual results vary considerably. These medications should not be used in combination with other GLP-1 receptor agonist-containing products.
The current medical consensus, supported by FDA labeling and clinical guidelines from organizations such as the Endocrine Society, American Gastroenterological Association (AGA), and American Association of Clinical Endocrinology (AACE), indicates that weight loss injections are intended for chronic use while benefits outweigh risks and the medication remains effective and tolerated. Obesity is increasingly recognized as a chronic, relapsing disease rather than a temporary condition or lifestyle choice. This paradigm shift has important implications for treatment duration—just as patients with hypertension or diabetes require ongoing medication management, individuals with obesity may need continuous pharmacological support to maintain weight loss and associated health benefits.
Clinical trial data supporting long-term use extends to approximately 2 years for semaglutide and 72 weeks for tirzepatide, with ongoing studies examining safety and efficacy beyond these timeframes. The STEP (Semaglutide Treatment Effect in People with obesity) trials and SURMOUNT (tirzepatide) trials have provided robust evidence for sustained weight loss maintenance with continued treatment. The SELECT cardiovascular outcomes trial followed patients on semaglutide 2.4 mg for approximately 3 years.
Guidelines recommend discontinuing therapy if a patient does not achieve at least 5% weight loss after 3 months on the maintenance dose, as benefits are unlikely to outweigh risks in such cases. The decision to continue treatment long-term must be individualized and reassessed periodically. Factors influencing long-term continuation include the degree of weight loss achieved, improvement in obesity-related comorbidities, side effect profile, cost considerations, and patient preference. Some individuals may achieve sufficient lifestyle modification to maintain weight loss without medication, while others may experience weight regain upon discontinuation, necessitating resumed or lifelong therapy.
It is important to note that while these medications can be taken long-term, there is no official requirement to take them "forever." Treatment duration should be determined collaboratively between patient and physician based on individual circumstances, treatment response, and evolving health needs.
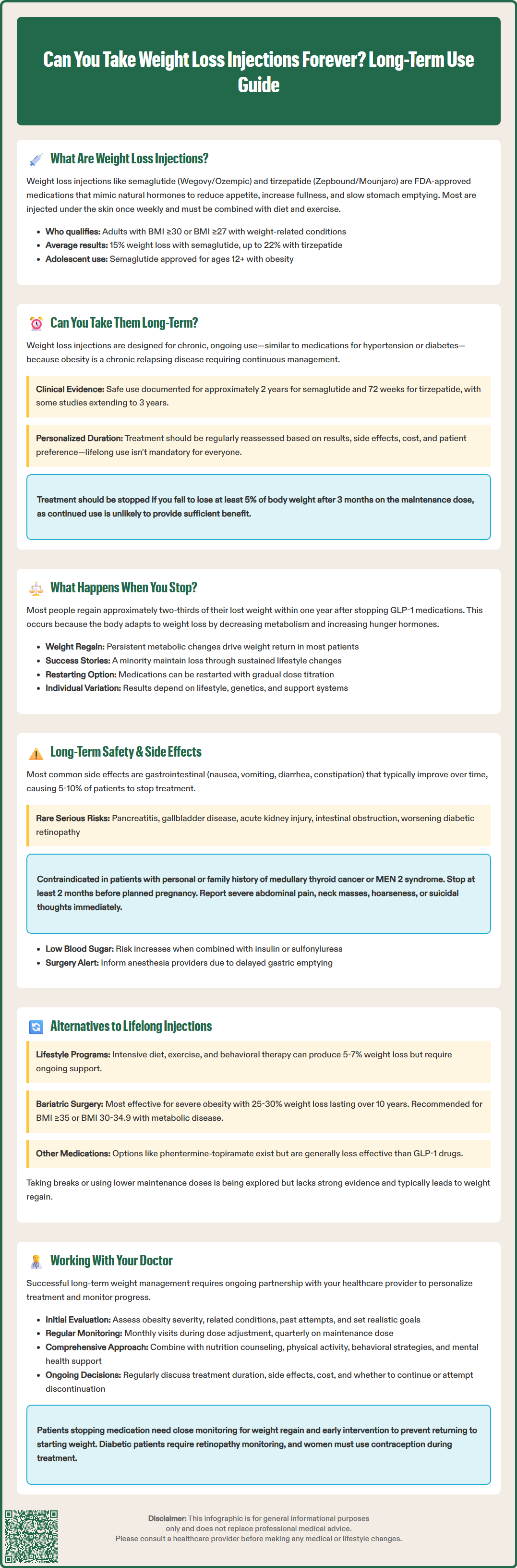
Discontinuation of weight loss injections typically results in weight regain for most individuals, though the extent and timeline vary considerably. Clinical trial data consistently demonstrates that when GLP-1 receptor agonists are stopped, patients regain a substantial portion of their lost weight within one year. The STEP 1 extension study showed that participants who discontinued semaglutide regained approximately two-thirds of their lost weight within one year of stopping treatment. Similarly, the SURMOUNT-4 randomized withdrawal trial demonstrated significant weight regain when tirzepatide was discontinued after initial weight loss. This phenomenon reflects the underlying biology of obesity, including metabolic adaptations that favor weight regain.
The physiological mechanisms driving weight regain after discontinuation are multifactorial. When weight loss occurs, the body undergoes metabolic adaptations including decreased energy expenditure, increased hunger hormones (such as ghrelin), and reduced satiety signals. These adaptations persist even after weight loss stabilizes, creating a biological drive to return to the previous weight set point. When the appetite-suppressing effects of incretin-based medications are removed, these compensatory mechanisms become unopposed, leading to increased hunger, reduced fullness, and gradual weight regain.
Not all individuals experience the same degree of weight regain. Factors that may influence outcomes after discontinuation include the extent of lifestyle modifications implemented during treatment, baseline metabolic health, genetic factors, and psychosocial support systems. Some patients who have successfully adopted sustainable dietary changes, regular physical activity, and behavioral strategies may maintain a portion of their weight loss. However, current evidence suggests this represents a minority of patients.
For individuals who discontinue treatment and experience significant weight regain, restarting the medication may be considered, though evidence specifically studying this approach is limited. If restarting, dose re-titration is typically recommended to minimize gastrointestinal side effects, and patients should be monitored closely. This approach should be discussed with a healthcare provider to ensure appropriate management and expectations.
The safety profile of GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists has been extensively studied in both diabetes and obesity populations, with generally favorable long-term safety data. The most common adverse effects are gastrointestinal, including nausea, vomiting, diarrhea, constipation, and abdominal discomfort. These symptoms typically occur during dose escalation and often diminish over time as tolerance develops. Most gastrointestinal side effects are mild to moderate in severity, though they lead to treatment discontinuation in approximately 5-10% of patients.
More serious but less common adverse effects require clinical vigilance. Pancreatitis has been reported with these medications, though a definitive causal relationship remains uncertain. Patients should be counseled to seek immediate medical attention for severe, persistent abdominal pain. Gallbladder disease, including cholelithiasis and cholecystitis, occurs more frequently with rapid weight loss and has been observed in clinical trials. Hypoglycemia risk is low when these medications are used alone but increases when combined with insulin or sulfonylureas.
Additional FDA label warnings include acute kidney injury (often secondary to dehydration from gastrointestinal side effects), ileus/intestinal obstruction, and risk of diabetic retinopathy complications in patients with type 2 diabetes, particularly with semaglutide. These medications are contraindicated during pregnancy and should be discontinued when pregnancy is recognized. Due to their long half-lives, women of childbearing potential should consider stopping treatment at least 2 months before a planned pregnancy.
The FDA has issued warnings regarding potential thyroid risks. In rodent studies, GLP-1 receptor agonists caused thyroid C-cell tumors, including medullary thyroid carcinoma. While there is no established link in humans, these medications are contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Patients should report any neck mass, hoarseness, or difficulty swallowing.
Emerging concerns include potential effects on muscle mass loss during rapid weight loss and reports of suicidal ideation. The Wegovy label includes a warning to monitor for depression or suicidal thoughts. Cardiovascular outcomes trials have demonstrated benefits, with semaglutide 2.4 mg now FDA-approved to reduce the risk of major adverse cardiovascular events in adults with established cardiovascular disease and either overweight or obesity, based on the SELECT trial.
Patients on chronic therapy should maintain regular follow-up with their healthcare provider, including monitoring for adverse effects, assessment of treatment efficacy, and evaluation of ongoing appropriateness of therapy. Patients should also inform anesthesia teams about their use of these medications prior to procedures due to their effects on gastric emptying.
For individuals seeking alternatives to indefinite medication use, several evidence-based approaches exist, though their effectiveness varies considerably. Intensive lifestyle intervention remains the foundation of obesity management and involves structured programs combining dietary modification, increased physical activity, and behavioral therapy. The Diabetes Prevention Program demonstrated that intensive lifestyle intervention can produce 5-7% weight loss and reduce diabetes risk, though maintaining this weight loss long-term proves challenging for many individuals without ongoing support.
Bariatric surgery represents the most effective intervention for severe obesity, producing average weight loss of 25-30% of total body weight with durable results extending beyond 10 years. Procedures such as Roux-en-Y gastric bypass and sleeve gastrectomy alter gastrointestinal anatomy and physiology, leading to sustained changes in appetite hormones and metabolism. According to 2022 ASMBS/IFSO guidelines, surgery is recommended for individuals with BMI ≥35 kg/m² regardless of comorbidities and may be considered for those with BMI 30-34.9 kg/m² with metabolic disease, though insurance coverage criteria may still follow older thresholds. While highly effective, surgery carries procedural risks and requires lifelong nutritional monitoring and supplementation.
Other pharmacological options include older weight loss medications such as phentermine-topiramate and naltrexone-bupropion, which have different mechanisms of action and may be appropriate for some patients. However, these agents generally produce less weight loss than GLP-1 receptor agonists and also require chronic administration for weight maintenance. Orlistat, a lipase inhibitor, is available over-the-counter but has limited efficacy and significant gastrointestinal side effects.
Intermittent or cyclical medication use is being explored as a potential strategy, though robust clinical trial evidence supporting this approach is lacking. Some clinicians and patients experiment with periodic breaks from medication or dose reduction after achieving weight loss goals, but current data suggests this frequently results in weight regain. Emerging research is investigating whether lower maintenance doses might sustain weight loss while reducing cost and side effect burden, but this approach is not yet supported by randomized controlled trials and should only be undertaken with physician guidance.
Successful long-term weight management requires a collaborative, individualized approach between patient and healthcare provider. Initial evaluation should include comprehensive assessment of obesity severity, related comorbidities, previous weight loss attempts, psychosocial factors, and patient goals and preferences. This assessment helps determine whether weight loss injections are appropriate and establishes realistic expectations for treatment outcomes and duration.
Ongoing monitoring is essential for patients receiving weight loss injections. Regular follow-up visits should be individualized based on response, tolerance, and comorbidities. Many patients benefit from monthly visits during dose titration and at least quarterly once a maintenance dose is established. These visits should assess weight trajectory, side effects, adherence, and improvement in obesity-related comorbidities such as blood pressure, lipids, and glycemic control. Laboratory monitoring may include baseline and periodic assessment of lipid panel, hemoglobin A1c (if diabetic or prediabetic), liver function tests, and renal function, particularly in patients with pre-existing conditions.
Patients should be counseled on warning signs requiring immediate medical attention, including severe abdominal pain (potential pancreatitis), signs of gallbladder disease, symptoms of thyroid masses, persistent vomiting leading to dehydration or acute kidney injury, intestinal obstruction, and changes in mood or suicidal thoughts. Patients with type 2 diabetes should be monitored for diabetic retinopathy complications. Women of childbearing potential should use effective contraception during treatment and inform their provider immediately if pregnancy occurs. Patients should also inform anesthesia providers about their use of these medications prior to procedures due to delayed gastric emptying concerns.
The conversation about treatment duration should be ongoing and revisited regularly. Factors to discuss include the patient's satisfaction with weight loss achieved, tolerance of side effects, financial considerations including insurance coverage, and personal preferences regarding long-term medication use. Some patients may wish to attempt discontinuation after achieving significant weight loss and implementing lifestyle changes, while others may prefer continued treatment to maintain their results. Neither approach is inherently correct—the decision should reflect individual circumstances and values.
Comprehensive weight management extends beyond medication alone. Physicians should emphasize the importance of concurrent lifestyle modifications, including nutrition counseling, physical activity recommendations, behavioral strategies, and psychosocial support. Referral to registered dietitians, exercise physiologists, or behavioral health specialists can enhance outcomes. For patients who discontinue medication, close monitoring for weight regain and early intervention if regain occurs can prevent return to baseline weight. If therapy is interrupted, dose re-titration is typically recommended when restarting. Ultimately, obesity management is a chronic endeavor requiring sustained engagement, flexibility, and partnership between patient and healthcare team.
Weight loss injections are approved for chronic use and can be taken long-term when medically appropriate. Clinical trial data supports safety for at least 2 years with semaglutide and 72 weeks with tirzepatide, with ongoing studies examining longer durations. Treatment duration should be individualized based on efficacy, tolerability, and regular reassessment with your healthcare provider.
Most patients regain a substantial portion of lost weight after discontinuing GLP-1 medications, with studies showing approximately two-thirds of weight regained within one year. This occurs due to metabolic adaptations including increased hunger hormones and decreased energy expenditure that persist after weight loss.
Common side effects include gastrointestinal symptoms like nausea and diarrhea. Serious but less common risks include pancreatitis, gallbladder disease, acute kidney injury, and potential thyroid concerns. These medications are contraindicated in patients with personal or family history of medullary thyroid carcinoma or MEN 2 syndrome, and require regular monitoring by a healthcare provider.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.