LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Do you put weight back on after weight loss injections? This is a critical question for anyone considering or currently using GLP-1 medications like Wegovy or Zepbound. Clinical evidence shows that weight regain is common after stopping these injections, with studies indicating patients may regain approximately two-thirds of lost weight within one year of discontinuation. Understanding why this happens and how to prepare for life after treatment is essential for long-term success. This article examines the science behind weight regain, evidence-based maintenance strategies, and medical guidance for transitioning off weight loss medications.
Quick Answer: Most patients regain significant weight after stopping weight loss injections, with clinical trials showing approximately two-thirds of lost weight returns within one year of discontinuation.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections primarily include glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), as well as tirzepatide (Zepbound), a dual GIP/GLP-1 receptor agonist. These medications mimic naturally occurring incretin hormones that regulate appetite and glucose metabolism.
The primary mechanism involves binding to receptors in the brain, particularly in areas controlling appetite and satiety. This action slows gastric emptying, meaning food remains in the stomach longer, creating prolonged feelings of fullness after meals. Patients typically report reduced hunger and decreased food cravings, making it easier to adhere to calorie-restricted diets. Additionally, these medications enhance insulin secretion in a glucose-dependent manner while suppressing glucagon release, improving overall glycemic control.
Clinical trials demonstrate specific efficacy for each medication. Semaglutide 2.4 mg (Wegovy) produces average weight loss of approximately 15% of initial body weight over 68 weeks when combined with lifestyle modifications. Tirzepatide (Zepbound) has shown even greater efficacy, with weight reductions of 15-22.5% in clinical trials. It's important to note that Ozempic (semaglutide) and Mounjaro (tirzepatide) are FDA-approved for type 2 diabetes management, not weight loss, though they contain the same active ingredients as their weight management counterparts.
These medications provide pharmacological support for weight management by modifying appetite signals and metabolic processes while the medication remains active in your system, which is why understanding what happens after discontinuation is clinically significant for long-term weight management planning.
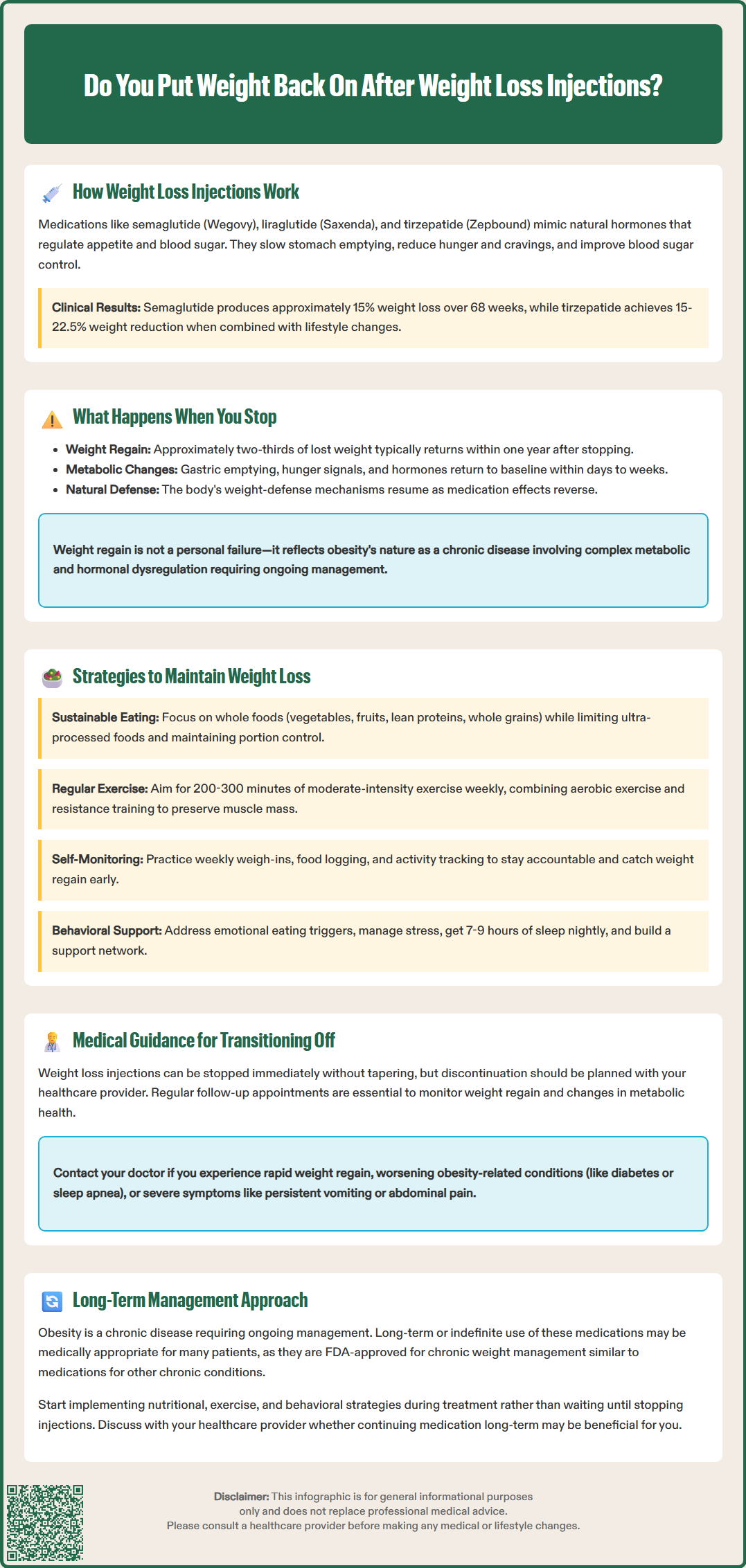
Weight regain after discontinuing incretin-based medications is a well-documented phenomenon in clinical research, though the extent varies considerably among individuals. The STEP 1 extension trial found that participants who stopped semaglutide regained approximately two-thirds of their lost weight within one year of discontinuation. Similarly, the SURMOUNT-4 trial showed significant weight regain when tirzepatide was discontinued compared to those who continued treatment.
The physiological explanation centers on the reversal of the medication's effects. Once you stop injections, gastric emptying returns to baseline rates, appetite-suppressing signals diminish, and the hormonal modifications that facilitated weight loss are no longer present. Many patients report a return of hunger sensations and food cravings within days to weeks of their last dose. The body's compensatory mechanisms—which evolved to defend against weight loss—become unopposed without pharmacological intervention.
Several factors influence the degree of weight regain. Patients who established sustainable dietary and exercise habits during treatment tend to maintain more of their weight loss compared to those who relied primarily on medication effects without lifestyle modification. While longer treatment periods may provide more opportunity for behavioral changes, this doesn't guarantee maintained weight loss after discontinuation.
It's crucial to recognize that weight regain doesn't represent treatment failure or lack of willpower. Rather, it reflects the chronic nature of obesity as a disease characterized by complex metabolic, hormonal, and neurological dysregulation. The American Diabetes Association and American Medical Association recognize obesity as requiring long-term management, similar to other chronic conditions like hypertension or diabetes. For many patients, long-term treatment may be medically appropriate as these medications are FDA-approved for chronic weight management.
Successful long-term weight maintenance after weight loss injections requires a comprehensive, multifaceted approach that addresses behavioral, nutritional, and physical activity components. Evidence suggests that patients who implement these strategies during treatment—rather than waiting until discontinuation—achieve better outcomes.
Nutritional strategies form the foundation of weight maintenance. Focus on establishing a sustainable eating pattern rather than restrictive dieting. Emphasize whole foods including vegetables, fruits, lean proteins, and whole grains while limiting ultra-processed foods high in added sugars and unhealthy fats. Portion control remains important; many patients benefit from continued use of measuring tools or mindful eating practices developed during treatment. Regular meal timing and adequate protein intake may help preserve lean muscle mass and promote satiety, though specific protein needs should be discussed with your healthcare provider or registered dietitian nutritionist (RDN), especially if you have kidney disease.
Physical activity plays a critical role in weight maintenance, with evidence supporting at least 200-300 minutes of moderate-intensity exercise weekly for those maintaining significant weight loss, according to the US Physical Activity Guidelines. This exceeds general health recommendations but reflects the increased energy expenditure needed to counteract metabolic adaptation. Incorporate both aerobic exercise and resistance training; the latter is particularly important for maintaining muscle mass, which supports metabolic rate.
Behavioral strategies include regular self-monitoring through weekly weigh-ins, food logging, and activity tracking. Identify and address emotional eating triggers, develop stress management techniques, and build a support network. Consider ongoing participation in structured weight management programs or support groups. Sleep optimization (7-9 hours nightly) and stress reduction also contribute to weight maintenance by regulating hormones that influence appetite and metabolism.
Some patients may benefit from continuing FDA-approved doses of weight management medications rather than discontinuation. Discuss these options with your healthcare provider as part of an individualized long-term management plan.
Discontinuing weight loss injections should be a planned, medically supervised process. The FDA-approved prescribing information doesn't require a tapering protocol, and medications can be stopped without dose reduction.
Before discontinuation, schedule a comprehensive evaluation with your healthcare provider. This assessment should include current weight, body composition if available, metabolic parameters (fasting glucose, A1C, lipid panel), blood pressure, and review of comorbid conditions. Discuss your reasons for considering discontinuation—whether due to cost, side effects, achievement of weight goals, or other factors. Your provider can help determine if stopping is appropriate or if alternative strategies might better serve your health needs.
Monitoring after discontinuation is essential for early intervention if significant weight regain occurs. Consider regular follow-up appointments with your healthcare provider to track your weight and health parameters. Work with your provider to establish an individualized monitoring plan and determine when additional interventions might be needed. Continue monitoring metabolic parameters, as weight regain may affect diabetes control, blood pressure, and lipid levels.
When to seek medical attention: Contact your healthcare provider if you experience rapid weight regain, return of obesity-related complications (worsening diabetes control, sleep apnea symptoms, joint pain), or psychological distress related to weight changes. Also seek immediate medical care for severe abdominal pain, persistent vomiting, or signs of gallbladder problems. If you're planning pregnancy, discuss medication discontinuation timing with your provider, as these medications are not recommended during pregnancy.
Consider referral to specialists such as American Board of Obesity Medicine (ABOM) certified physicians or comprehensive weight management programs that offer multidisciplinary support including registered dietitians, exercise physiologists, and behavioral health specialists. For some patients with BMI ≥35 with comorbidities or BMI ≥40, bariatric surgery may be appropriate according to current guidelines. Remember that obesity is a chronic disease; ongoing medical management—whether through continued medication, intensive lifestyle intervention, or other approaches—is often necessary for sustained health benefits.
Weight regain typically begins within weeks of discontinuation, with clinical trials showing patients regain approximately two-thirds of their lost weight within one year after stopping medications like semaglutide or tirzepatide. The rate varies based on individual factors and lifestyle habits established during treatment.
While complete prevention is challenging, patients who establish sustainable dietary patterns, engage in 200-300 minutes of weekly exercise, and implement behavioral strategies during treatment tend to maintain more weight loss after discontinuation. Some patients may benefit from continuing medication as part of long-term chronic disease management.
No, weight regain reflects the chronic nature of obesity as a disease with complex metabolic and hormonal dysregulation. The American Diabetes Association and American Medical Association recognize obesity as requiring long-term management similar to other chronic conditions like hypertension or diabetes.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.