LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Do you gain weight back after stopping weight loss injections? This question concerns many patients considering or currently using medications like Wegovy or Zepbound. Clinical evidence shows that weight regain is common after discontinuing these medications, with studies demonstrating patients typically regain approximately two-thirds of lost weight within one year of stopping treatment. This occurs because the pharmacological effects supporting weight loss—appetite suppression and delayed gastric emptying—cease when medication is discontinued. Understanding this pattern and implementing evidence-based maintenance strategies is essential for long-term success.
Quick Answer: Yes, weight regain is common after stopping weight loss injections, with clinical studies showing patients typically regain approximately two-thirds of lost weight within one year of discontinuation.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections approved for chronic weight management in the US include semaglutide (Wegovy) and tirzepatide (Zepbound). These medications work through different but related mechanisms—semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist, while tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist.
These medications primarily work by binding to receptors in the brain that control appetite and satiety. This action slows gastric emptying, meaning food remains in the stomach longer, creating prolonged feelings of fullness after meals. Patients typically report reduced hunger and decreased food cravings, making it easier to adhere to calorie-restricted diets. Additionally, these medications enhance insulin secretion in response to meals while suppressing glucagon release, improving overall glycemic control.
Clinical trials demonstrate significant weight loss with these medications when combined with lifestyle modifications. In the STEP 1 trial, semaglutide produced average weight loss of approximately 15% over 68 weeks, while the SURMOUNT-1 trial showed tirzepatide achieved 15-21% weight loss over 72 weeks. The FDA-approved dosing involves weekly subcutaneous injections, with gradual dose escalation to minimize gastrointestinal side effects. Common adverse effects include nausea, vomiting, diarrhea, and constipation, which generally improve over time.
Important safety considerations include a boxed warning for thyroid C-cell tumors (these medications are contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2) and should not be used during pregnancy.
These medications provide pharmacological support for weight loss by modifying appetite signals and digestive processes. When treatment stops, these effects cease, which helps explain why weight regain commonly occurs after discontinuation.
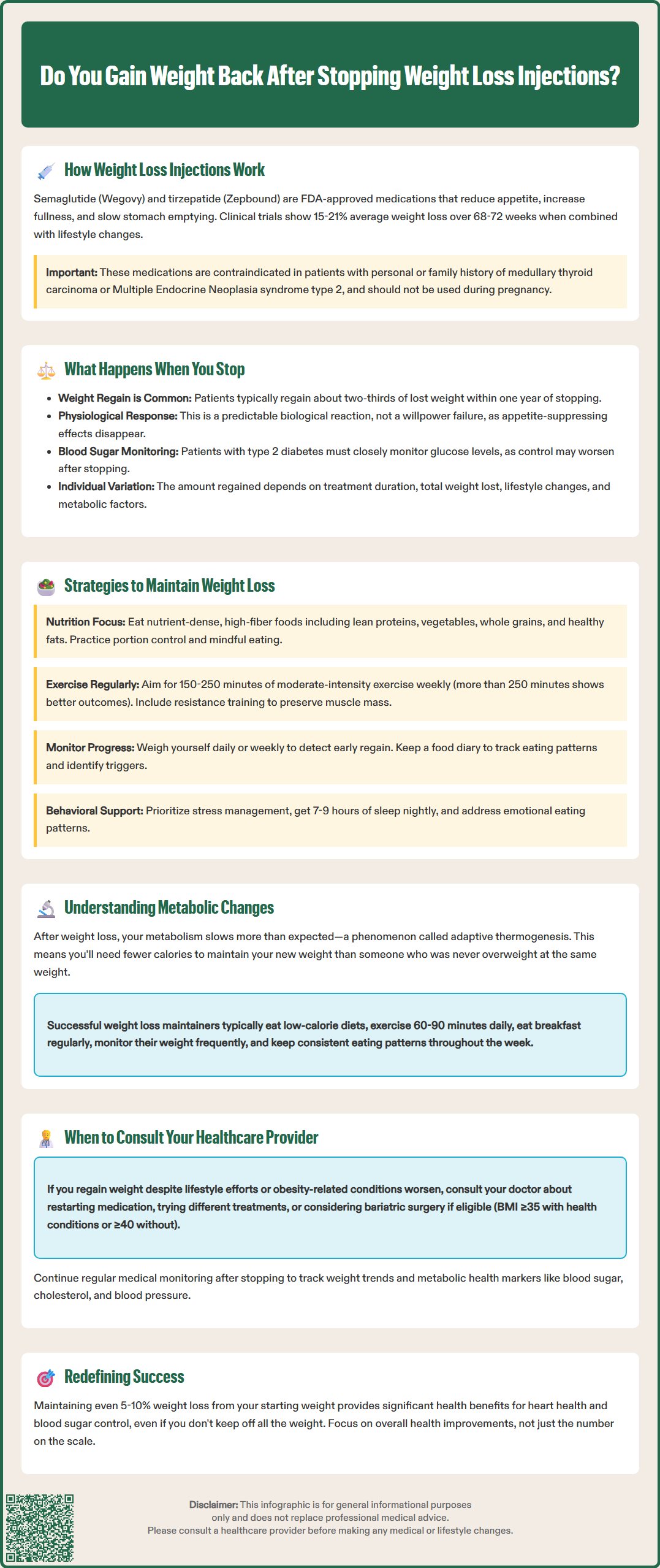
When patients discontinue weight loss injections, weight regain is common and well-documented in clinical studies. In the STEP 1 extension study of semaglutide, participants who discontinued the medication regained approximately two-thirds of their lost weight within one year of stopping treatment. This phenomenon occurs because the pharmacological effects that supported weight loss—appetite suppression, delayed gastric emptying, and enhanced satiety—are no longer present.
The body's homeostatic mechanisms, which regulate energy balance and body weight, reassert themselves after medication cessation. Many patients report increased hunger, reduced feelings of fullness after meals, and return of food cravings that were previously controlled by the medication. Gastric emptying returns to normal speed, eliminating the prolonged satiety that helped reduce caloric intake.
Clinical evidence from randomized withdrawal trials provides clear insights into this pattern. The STEP 4 trial showed that participants who continued semaglutide maintained their weight loss, while those who switched to placebo experienced significant regain. Similar findings were observed with tirzepatide in the SURMOUNT-4 trial. This weight regain is not a failure of willpower but rather a predictable physiological response to medication withdrawal.
For patients with type 2 diabetes who are taking these medications (Ozempic or Mounjaro, which contain the same active ingredients but are FDA-approved for diabetes, not weight management), stopping treatment requires special consideration. Blood glucose levels may worsen after discontinuation, potentially requiring adjustment of other diabetes medications. Close monitoring of glucose levels and coordination with your healthcare provider is essential.
The rate and extent of weight regain vary among individuals and depend on several factors, including the duration of treatment, amount of weight lost, lifestyle modifications implemented during treatment, and individual metabolic factors. Understanding this likelihood is essential for setting realistic expectations and planning long-term weight management strategies before discontinuing medication.
Maintaining weight loss after discontinuing weight loss injections requires a comprehensive, evidence-based approach that addresses both dietary and behavioral factors. The most successful strategies involve implementing sustainable lifestyle changes during treatment, rather than relying solely on medication effects.
Dietary modifications should focus on nutrient-dense, high-fiber foods that promote natural satiety. Emphasize lean proteins (which increase satiety and preserve muscle mass), vegetables, whole grains, and healthy fats. Portion control remains critical—using smaller plates, measuring servings, and practicing mindful eating can help compensate for the loss of medication-induced appetite suppression. The American Diabetes Association and other US guidelines recommend individualized meal planning that creates a modest caloric deficit (500-750 calories daily) for gradual, sustainable weight maintenance.
Physical activity plays an essential role in preventing weight regain. The American College of Sports Medicine recommends at least 150-250 minutes of moderate-intensity exercise weekly for weight maintenance, with higher amounts (>250 minutes weekly) associated with better long-term outcomes. Resistance training is particularly important for preserving lean muscle mass, which supports metabolic rate. Incorporating both structured exercise and increased daily movement (taking stairs, walking meetings) helps maintain energy expenditure.
Behavioral strategies include regular self-monitoring through daily weighing or weekly measurements, which allows early detection of weight regain and prompt intervention. Keeping a food diary, whether paper-based or using smartphone applications, increases awareness of eating patterns and helps identify triggers for overeating. Stress management techniques, adequate sleep (7-9 hours nightly), and addressing emotional eating patterns are equally important.
Consider working with a registered dietitian or behavioral psychologist who specializes in weight management. Professional support provides accountability, personalized strategies, and evidence-based interventions. Some patients benefit from structured programs that provide ongoing support during the transition off medication. If you notice consistent weight regain, consult your healthcare provider to discuss whether resuming medication or exploring alternative treatments is appropriate.
Successful long-term weight management without medication requires understanding that obesity is a chronic condition influenced by genetic, metabolic, environmental, and behavioral factors. Evidence suggests that sustained weight loss maintenance is achievable but requires ongoing effort and often multifaceted approaches.
The National Weight Control Registry, which tracks individuals who have maintained significant weight loss (≥30 pounds for ≥1 year), identifies common characteristics among successful maintainers. These include eating a low-calorie, low-fat diet, engaging in high levels of physical activity (approximately 60-90 minutes daily), eating breakfast regularly, self-monitoring weight frequently, and maintaining consistent eating patterns across weekdays and weekends. These behaviors become habitual rather than temporary measures.
Metabolic considerations are important to acknowledge. After significant weight loss, metabolic adaptation occurs—the body's energy expenditure decreases beyond what would be predicted by the loss of body mass alone. This adaptive thermogenesis means that maintaining weight loss requires fewer calories than would be expected for someone of the same weight who was never overweight. This physiological reality makes long-term maintenance challenging and explains why many individuals struggle despite adherence to healthy behaviors.
Medical monitoring should continue even after stopping weight loss injections. Regular follow-up with your primary care provider allows assessment of weight trends, metabolic parameters (lipids, glucose, blood pressure), and obesity-related comorbidities. If weight regain occurs despite intensive lifestyle efforts, discuss alternative evidence-based treatments, which may include resuming medication (with appropriate re-titration per FDA guidelines), trying different medications, or considering bariatric surgery for eligible patients. According to ASMBS/IFSO guidelines, bariatric surgery may be considered for individuals with BMI ≥35 kg/m² with obesity-related conditions or BMI ≥40 kg/m² regardless of comorbidities.
Realistic expectations are essential. Complete prevention of weight regain is uncommon, but maintaining even 5-10% weight loss below starting weight provides significant health benefits, including improved cardiovascular risk factors and glycemic control. Focus on health improvements and functional gains rather than solely on scale numbers. If you experience weight regain accompanied by worsening of obesity-related conditions (hypertension, diabetes, sleep apnea), prompt medical consultation is warranted to optimize your treatment plan.
Clinical studies show that patients who discontinue semaglutide typically regain approximately two-thirds of their lost weight within one year of stopping treatment. Similar patterns are observed with tirzepatide discontinuation.
Weight regain occurs because the pharmacological effects that supported weight loss—appetite suppression, delayed gastric emptying, and enhanced satiety—cease when medication is discontinued. The body's homeostatic mechanisms that regulate energy balance and body weight then reassert themselves.
While complete prevention is uncommon, implementing comprehensive lifestyle modifications during treatment can help minimize regain. Evidence-based strategies include maintaining a nutrient-dense diet, engaging in 150-250 minutes of weekly physical activity, regular self-monitoring, and working with healthcare professionals for ongoing support.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.