LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Weight loss injections such as semaglutide (Wegovy) and tirzepatide (Zepbound) can produce significant weight reduction without structured exercise programs, though the FDA has approved them as adjuncts to reduced-calorie diet and increased physical activity. These glucagon-like peptide-1 (GLP-1) receptor agonists work primarily by suppressing appetite and reducing food intake rather than increasing metabolic rate. Clinical trials demonstrate substantial weight loss even without mandated exercise regimens, though participants received lifestyle counseling. Understanding how these medications function, what results to expect, and when to incorporate physical activity helps patients and clinicians make informed treatment decisions for chronic weight management.
Quick Answer: Weight loss injections such as semaglutide and tirzepatide can produce significant weight reduction without structured exercise by suppressing appetite and reducing food intake, though the FDA approves them as adjuncts to diet and physical activity.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and tirzepatide (Zepbound), function through multiple physiological mechanisms that reduce body weight. It's important to note that while these medications can work without structured exercise programs, the FDA has approved them specifically as adjuncts to reduced-calorie diet and increased physical activity.
Wegovy (semaglutide 2.4 mg) and Zepbound (tirzepatide) are FDA-approved for chronic weight management in adults with a BMI ≥30 kg/m², or ≥27 kg/m² with at least one weight-related comorbidity. Ozempic (semaglutide) and Mounjaro (tirzepatide) are approved only for type 2 diabetes management, not for weight loss.
These medications mimic naturally occurring incretin hormones that regulate appetite and glucose metabolism. Their primary mechanism involves binding to GLP-1 receptors in the brain's hypothalamus, specifically in areas controlling satiety and food intake. This activation leads to reduced appetite, increased feelings of fullness after meals, and decreased food cravings. Patients typically report feeling satisfied with smaller portions and experiencing less frequent hunger between meals. Additionally, these agents slow gastric emptying, prolonging the sensation of fullness after eating.
GLP-1 receptor agonists also improve glycemic control by enhancing glucose-dependent insulin secretion from pancreatic beta cells and suppressing inappropriate glucagon release. Tirzepatide offers dual action by also activating glucose-dependent insulinotropic polypeptide (GIP) receptors, which may contribute to its enhanced weight loss efficacy compared to single-agonist formulations.
These medications do not directly increase metabolic rate or fat oxidation in the manner that exercise does. Instead, they create a sustained caloric deficit by reducing energy intake through appetite suppression. The weight loss achieved occurs primarily through decreased food consumption rather than increased energy expenditure, which helps explain why these injections can produce significant results even without formal exercise programs.
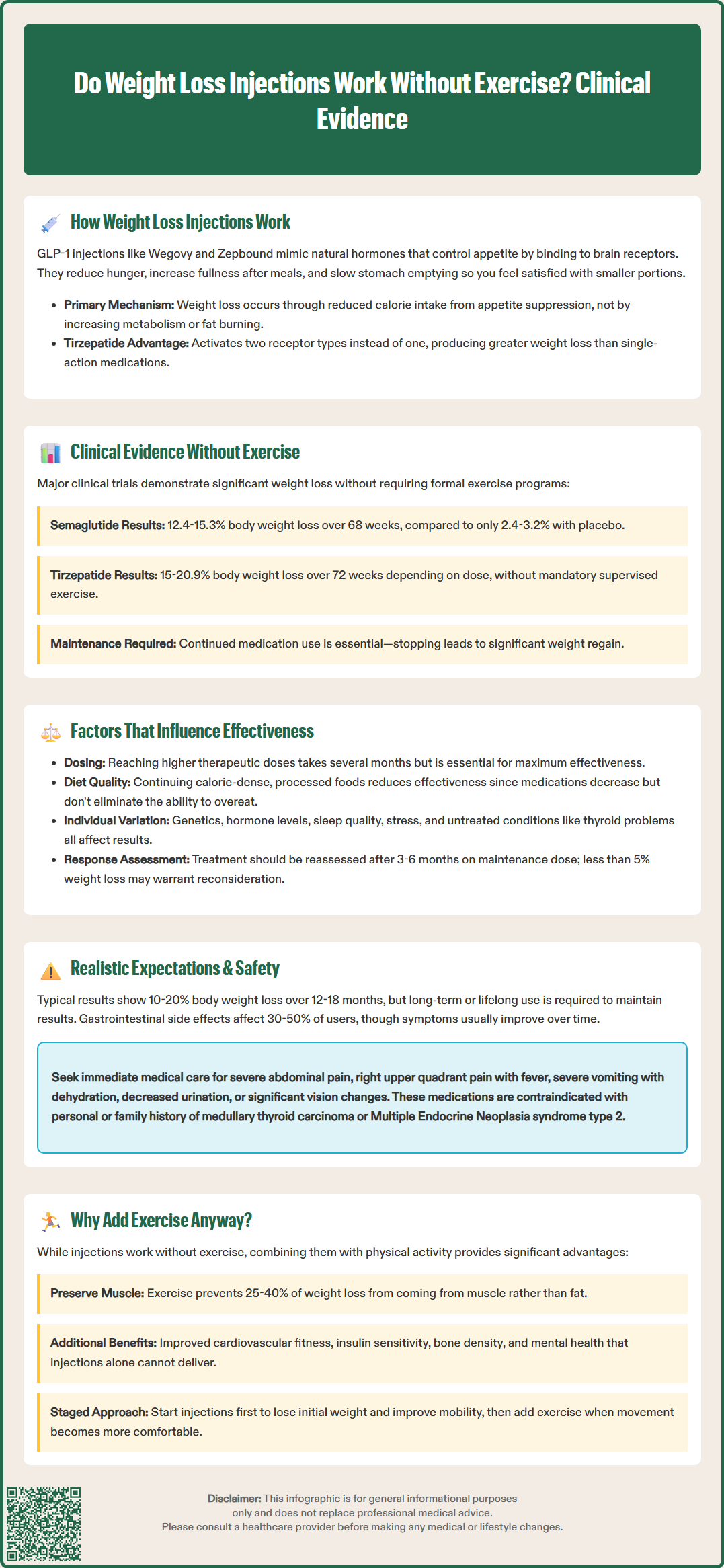
Robust clinical trial data demonstrates that weight loss injections produce significant results without mandated structured exercise programs, though it's important to note that all pivotal trials included lifestyle counseling on both diet and physical activity as part of the study protocols.
The STEP (Semaglutide Treatment Effect in People with obesity) trials, which included over 4,500 participants, showed that semaglutide 2.4 mg weekly resulted in mean weight loss of 12.4% to 15.3% of initial body weight over 68 weeks, compared to 2.4% to 3.2% with placebo. In the STEP 1 trial published in the New England Journal of Medicine, participants received counseling on caloric restriction and physical activity recommendations, though no formal exercise program was required.
The SURMOUNT-1 trial evaluating tirzepatide demonstrated substantial results, with participants achieving mean weight reductions of approximately 15% (5 mg), 19.5% (10 mg), and 20.9% (15 mg) over 72 weeks. Again, lifestyle counseling was provided, but no supervised exercise program was mandated. Weight loss occurred primarily through reduced caloric intake facilitated by the medication's appetite-suppressing effects.
The STEP 4 trial, published in JAMA, demonstrated the importance of continued medication use. When participants who had been taking semaglutide were randomized to either continue the medication or switch to placebo after 20 weeks, those who continued treatment maintained their weight loss, while those switched to placebo regained significant weight.
It is important to note that while formal exercise programs were not required in these trials, participants did receive dietary counseling promoting reduced caloric intake. The injections facilitated adherence to lower-calorie diets by reducing hunger and cravings. Therefore, while structured exercise is not necessary for weight loss with these medications, some degree of dietary awareness and portion control optimization typically accompanies successful outcomes. The medications make caloric restriction more tolerable and sustainable rather than creating weight loss entirely independent of behavioral factors.
Multiple variables affect individual responses to weight loss injections, creating substantial heterogeneity in outcomes even without exercise. Baseline body mass index (BMI) significantly influences absolute weight loss, with individuals having higher starting weights typically losing more total pounds, though percentage weight loss remains relatively consistent across BMI categories. Clinical trials suggest that a proportion of patients may be "non-responders," achieving less than 5% weight loss despite adequate medication adherence and time on a maintenance dose.
Genetic factors may play a role in treatment response, though it's important to note that pharmacogenomic testing is not currently recommended for clinical decision-making regarding these medications. Individual differences in gastric emptying rates, baseline incretin hormone levels, and satiety signaling may contribute to response variability.
Dosing and medication adherence are critical determinants of success. Weight loss typically follows a dose-response relationship, with higher doses producing greater weight reduction. The gradual dose escalation protocols used with these medications—designed to minimize gastrointestinal adverse effects—mean that maximum efficacy may not be apparent until patients reach therapeutic doses after several months. Premature discontinuation due to side effects or cost barriers significantly limits effectiveness.
Clinicians should reassess treatment efficacy after approximately 3-6 months on a maintenance dose, as recommended by clinical guidelines. If a patient has not achieved at least 5% weight loss by this point, the benefit-risk profile should be reevaluated.
Dietary composition and eating patterns, while not requiring formal exercise, still matter considerably. Patients who continue consuming calorie-dense, highly processed foods may experience attenuated weight loss compared to those who optimize nutrition quality. The medications reduce appetite but do not eliminate the ability to override satiety signals. Psychological factors including stress, sleep quality, and emotional eating patterns also influence outcomes. Concurrent medications, particularly those associated with weight gain such as certain antidepressants or antipsychotics, may partially counteract weight loss effects. Underlying medical conditions affecting metabolism, including hypothyroidism or polycystic ovary syndrome, should be appropriately managed to optimize treatment response.
While weight loss injections work without structured exercise programs, setting appropriate expectations is essential for patient satisfaction and treatment persistence. Most patients can expect to lose 10% to 20% of their initial body weight over 12 to 18 months when using therapeutic doses of semaglutide or tirzepatide, with weight loss plateauing after this period. This represents clinically significant improvement associated with reduced cardiovascular risk, improved glycemic control in those with diabetes, and decreased joint stress.
However, these medications are not a cure for obesity. Weight loss occurs primarily during the active treatment phase, and substantial weight regain typically follows discontinuation. The STEP 1 extension study demonstrated that participants who stopped semaglutide after achieving weight loss regained a significant portion of their lost weight within one year. This underscores that these medications require long-term, potentially lifelong use to maintain benefits—a consideration with significant cost and adherence implications.
The rate of weight loss varies considerably among individuals and over time. Initial weight loss is often most rapid in the first three to six months, with gradual deceleration thereafter. Some patients experience frustrating plateaus despite continued medication use. While formal exercise programs are not required for weight loss with these medications, physical activity may provide additional benefits for weight maintenance and overall health.
Adverse effects may limit tolerability and effectiveness. Gastrointestinal symptoms including nausea, vomiting, diarrhea, and constipation affect 30% to 50% of users, though these typically improve over time. Patients should seek immediate medical attention for severe persistent abdominal pain (possible pancreatitis), right upper quadrant pain with fever (possible gallbladder disease), severe vomiting leading to dehydration, decreased urine output (possible acute kidney injury), or significant vision changes (possible diabetic retinopathy complications).
Other important safety considerations include hypoglycemia risk when combined with insulin or sulfonylureas, suicidal ideation (monitor for mood changes), and contraindication during pregnancy. Tirzepatide may reduce oral contraceptive effectiveness during dose escalation, so alternative or backup contraception methods should be considered. The FDA label includes a boxed warning regarding thyroid C-cell tumors, contraindicating use in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
Although weight loss injections can work without structured exercise programs, it's important to emphasize that the FDA has approved these medications specifically as adjuncts to reduced-calorie diet and increased physical activity. The American Diabetes Association Standards of Care and obesity treatment guidelines from organizations like the American Association of Clinical Endocrinology recommend comprehensive obesity management incorporating both pharmacological and behavioral interventions.
Exercise provides benefits beyond weight loss that medications cannot replicate. Regular physical activity helps preserve lean muscle mass during weight reduction, which is particularly important since approximately 25% to 40% of weight lost with GLP-1 agonists alone may come from lean tissue rather than fat, according to body composition studies. Resistance training helps maintain metabolic rate and functional capacity. Additionally, exercise improves cardiovascular fitness, insulin sensitivity, bone density, mental health, and overall quality of life—outcomes not directly addressed by appetite-suppressing medications.
Patients with specific comorbidities particularly benefit from combined approaches. Those with type 2 diabetes achieve better glycemic control when pairing injections with physical activity. Individuals with cardiovascular disease risk factors see greater improvements in blood pressure, lipid profiles, and inflammatory markers when exercise is included. Patients with mobility limitations or osteoarthritis may find that initial weight loss from injections improves their ability to subsequently engage in physical activity that was previously too uncomfortable.
Practical considerations should guide individualized recommendations. For severely deconditioned patients or those with significant obesity-related mobility impairment, initiating injections first and adding exercise once initial weight loss improves functional capacity represents a reasonable staged approach. Conversely, patients already engaged in regular physical activity should be encouraged to maintain these habits while starting medication.
Clinicians should emphasize that lifestyle changes, particularly dietary quality and eating patterns, remain important even when structured exercise is not feasible. Focusing on nutrient-dense foods, adequate protein intake to preserve muscle mass, and mindful eating practices optimizes outcomes. Referral to registered dietitian nutritionists (RDNs) for medical nutrition therapy enhances results. Behavioral support addressing emotional eating, stress management, and sleep hygiene complements pharmacological treatment. The goal is sustainable, health-promoting weight management rather than simply achieving a number on the scale through medication alone.
Yes, clinical trials demonstrate that GLP-1 medications like semaglutide and tirzepatide produce significant weight loss primarily through appetite suppression and reduced food intake, even without structured exercise programs. However, the FDA approves these medications as adjuncts to reduced-calorie diet and increased physical activity for optimal results.
Clinical trials show patients typically achieve clinically significant weight reduction with semaglutide or tirzepatide over 12-18 months without mandated exercise, though individual results vary based on medication adherence, dosing, dietary patterns, and baseline characteristics. Weight loss occurs primarily through reduced caloric intake facilitated by appetite suppression.
Substantial weight regain typically occurs after discontinuing weight loss injections, as demonstrated in clinical trials where patients who stopped semaglutide regained significant weight within one year. These medications require long-term, potentially lifelong use to maintain weight loss benefits.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.