LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
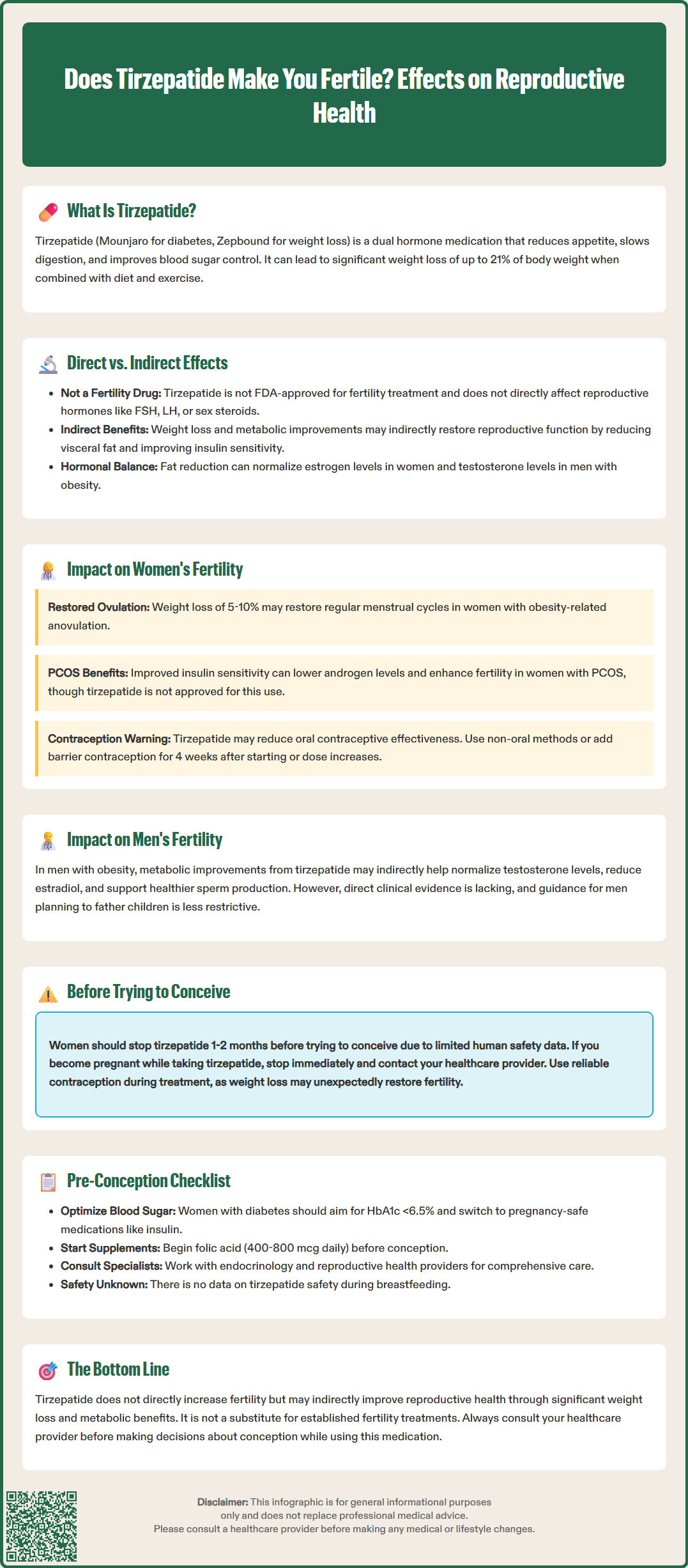
Does tirzepatide make you fertile? This question has emerged as more patients use tirzepatide (Mounjaro, Zepbound) for type 2 diabetes and weight management. Tirzepatide is a dual GIP and GLP-1 receptor agonist that produces substantial weight loss and metabolic improvements. While the medication is not approved for fertility treatment, its effects on weight reduction and insulin sensitivity may indirectly influence reproductive health. Understanding the relationship between tirzepatide and fertility requires examining both its direct pharmacological actions and the secondary metabolic benefits that can affect hormonal balance and ovulatory function in both women and men.
Quick Answer: Tirzepatide does not directly increase fertility, but its substantial weight loss and metabolic improvements may indirectly restore reproductive function in some patients with obesity-related infertility.
Tirzepatide is a novel dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for two primary indications: type 2 diabetes mellitus (marketed as Mounjaro) and chronic weight management (marketed as Zepbound). For weight management, it's specifically indicated as an adjunct to reduced-calorie diet and increased physical activity in adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity.
The mechanism of action involves mimicking two naturally occurring incretin hormones that regulate glucose metabolism and appetite. Tirzepatide enhances insulin secretion in a glucose-dependent manner, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. Clinical trials have demonstrated substantial weight loss—with mean reductions up to approximately 21% of body weight at 72 weeks in the SURMOUNT-1 trial—alongside meaningful improvements in hemoglobin A1c levels in patients with diabetes.
While tirzepatide's metabolic effects are well-established, questions have emerged regarding its potential impact on fertility. This interest stems primarily from the medication's profound effects on weight loss and metabolic health, both of which are connected to reproductive function. Understanding whether tirzepatide influences fertility requires examining both its pharmacological properties and the indirect metabolic improvements it produces. It is important to note that tirzepatide is not approved or indicated for fertility treatment, and any reproductive effects observed are secondary to its primary metabolic actions.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
Tirzepatide's hormonal effects extend beyond glucose regulation, though there is no established direct link between tirzepatide and fertility enhancement. The medication primarily targets metabolic pathways through GIP and GLP-1 receptors, which are widely expressed in pancreatic tissue, the gastrointestinal tract, adipose tissue, and certain brain regions involved in appetite regulation. Current evidence does not demonstrate that tirzepatide directly modulates reproductive hormones such as follicle-stimulating hormone (FSH), luteinizing hormone (LH), or sex steroids.
However, the medication's profound metabolic effects create an indirect hormonal cascade that may influence reproductive health. Significant weight loss—particularly reduction of visceral adipose tissue—can improve insulin sensitivity and reduce chronic low-grade inflammation, both of which affect the hypothalamic-pituitary-gonadal axis. Adipose tissue functions as an endocrine organ, producing hormones and inflammatory mediators that can disrupt normal reproductive function when present in excess.
In women with obesity, excess adipose tissue increases peripheral conversion of androgens to estrogens through aromatase activity, potentially disrupting normal menstrual cyclicity. Weight loss induced by tirzepatide may help restore more physiologic hormone levels. Additionally, improved insulin sensitivity can reduce hyperinsulinemia, which is known to stimulate ovarian androgen production and contribute to anovulation in certain conditions.
For men, obesity is associated with reduced testosterone levels, increased estradiol, and impaired spermatogenesis. While tirzepatide does not directly target these pathways, the metabolic improvements and weight reduction it facilitates may indirectly support healthier reproductive hormone profiles. Clinicians should recognize these potential indirect effects while emphasizing that tirzepatide is not a fertility medication.
There is currently no robust clinical evidence demonstrating that tirzepatide directly increases fertility in either women or men. The medication has not been studied in clinical trials specifically designed to assess fertility outcomes, and it is not indicated for infertility treatment. While there have been anecdotal clinical observations suggesting metabolic improvements with tirzepatide may influence reproductive capacity in certain patients, these observations require systematic study before drawing conclusions.
In women, particularly those with obesity-related anovulation, significant weight loss can restore ovulatory cycles and improve the likelihood of conception. Studies of bariatric surgery and intensive lifestyle interventions have consistently shown that weight reduction of 5-10% or more can improve menstrual regularity and fertility in women with obesity. Given that tirzepatide produces weight loss exceeding these thresholds in many patients, similar reproductive benefits may occur, though this requires further research.
For men with obesity, weight loss may improve testosterone levels, sperm quality, and sexual function. Obesity is associated with reduced sperm concentration, motility, and increased DNA fragmentation. While direct evidence for tirzepatide's effects on male fertility is lacking, the metabolic improvements it produces—including reduced inflammation, improved insulin sensitivity, and hormonal normalization—could theoretically benefit reproductive parameters.
Importantly, the FDA label for tirzepatide includes warnings about potential pregnancy risk and contraceptive interactions. The medication may reduce the effectiveness of oral contraceptives, particularly during the first 4 weeks after initiation and following dose escalation, due to delayed gastric emptying. Women of reproductive potential should use non-oral contraceptives or add a barrier method for 4 weeks after initiation and for 4 weeks after each dose escalation. Women should be counseled about the possibility of restored fertility with weight loss.
Infertility is defined in the US as the inability to conceive after 12 months of regular unprotected intercourse (or after 6 months in women age 35 and older). Women with irregular menstrual cycles should consider earlier evaluation.
Polycystic ovary syndrome (PCOS) represents a clinical scenario where tirzepatide's metabolic effects may have particular relevance to fertility, though this remains an area requiring further research. PCOS affects approximately 6-12% of women of reproductive age and is characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovarian morphology. Insulin resistance and obesity are present in 50-70% of women with PCOS and play central roles in the syndrome's pathophysiology.
Insulin resistance in PCOS contributes to hyperinsulinemia, which stimulates ovarian androgen production and disrupts normal follicular development. This creates a cycle of anovulation, irregular menses, and reduced fertility. Weight loss of just 5-10% has been shown to improve insulin sensitivity, reduce androgen levels, restore ovulatory cycles, and enhance fertility in women with PCOS. First-line management according to US guidelines, including those from the Endocrine Society and American Society for Reproductive Medicine, emphasizes lifestyle modification for weight reduction.
Tirzepatide's dual incretin agonism produces substantial weight loss and marked improvements in insulin sensitivity, making it theoretically relevant for metabolic aspects of PCOS management. Limited data from studies with other GLP-1 receptor agonists have reported improvements in menstrual regularity and metabolic parameters in women with PCOS, though data specific to tirzepatide remain limited. In head-to-head trials like SURMOUNT-5, tirzepatide has demonstrated greater weight loss compared to single GLP-1 receptor agonists like semaglutide.
However, it is crucial to emphasize that tirzepatide is not FDA-approved for PCOS treatment or fertility enhancement. Women with PCOS seeking fertility should be managed according to established guidelines, which typically include lifestyle modification, ovulation induction with medications such as letrozole (first-line in the US) or clomiphene citrate, and metformin in selected cases. Any consideration of tirzepatide as part of comprehensive weight management in women with PCOS and obesity should involve shared decision-making with endocrinology and reproductive specialists. Any woman with PCOS using tirzepatide who wishes to conceive should discontinue the medication appropriately before attempting pregnancy.
Women planning pregnancy should discontinue tirzepatide at least 1-2 months before attempting to conceive, based on the medication's approximately 5-day half-life. This washout period allows for adequate drug clearance and minimizes potential fetal exposure during early pregnancy. While the FDA label does not specify a precise preconception discontinuation timeline, it does advise discontinuation when pregnancy is recognized. Animal studies have shown adverse developmental outcomes, and while human data are limited, the precautionary principle supports medication discontinuation before conception.
Patients should be counseled that weight loss itself may restore fertility, potentially leading to unintended pregnancy. Women of childbearing potential using tirzepatide should employ reliable contraception, with awareness that oral contraceptive effectiveness may be reduced during the first 4 weeks after starting tirzepatide or increasing the dose. Non-oral contraceptives or additional barrier methods should be used during these periods. Any patient who suspects pregnancy while taking tirzepatide should discontinue the medication immediately and contact their healthcare provider.
Before attempting conception, comprehensive preconception counseling is essential. This should include optimization of glycemic control in patients with diabetes (target HbA1c <6.5% before conception when achievable without significant hypoglycemia), folic acid supplementation (400-800 mcg daily, or higher doses in certain cases), and screening for diabetes-related complications. Patients should be transitioned to pregnancy-safe medications for diabetes management, such as insulin, well before conception attempts. Other potentially teratogenic medications like ACE inhibitors, ARBs, and statins should also be discontinued when planning pregnancy.
Regarding lactation, there are no data on tirzepatide presence in human milk, effects on the breastfed infant, or effects on milk production. The potential benefits and risks should be considered when using tirzepatide in lactating women.
Men taking tirzepatide who are planning to father children face less restrictive guidance, as the medication's effects on male fertility are not well-characterized and paternal exposure has not been established as a significant risk. However, given limited data, men may consider discussing timing of conception attempts with their healthcare provider. Both partners should be encouraged to optimize overall health, maintain achieved weight loss through lifestyle measures, and work closely with their healthcare team—including reproductive specialists when indicated—to ensure the safest approach to family planning while managing chronic metabolic conditions.
Tirzepatide is not FDA-approved for PCOS or fertility treatment, but its weight loss and insulin sensitivity improvements may indirectly benefit ovulatory function in women with PCOS and obesity. Women with PCOS seeking fertility should follow established treatment guidelines including lifestyle modification and ovulation induction medications like letrozole.
Women planning pregnancy should discontinue tirzepatide at least 1-2 months before attempting conception to allow adequate drug clearance. Patients should also transition to pregnancy-safe diabetes medications and use reliable contraception until ready to conceive, as weight loss may restore fertility.
Yes, tirzepatide may reduce oral contraceptive effectiveness during the first 4 weeks after starting the medication and for 4 weeks after each dose increase due to delayed gastric emptying. Women should use non-oral contraceptives or add a barrier method during these periods.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.