LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Does tirzepatide cause restless legs? Currently, restless legs syndrome is not listed as a known side effect of tirzepatide in FDA prescribing information or clinical trial data. Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management. While the medication commonly causes gastrointestinal side effects like nausea and diarrhea, there is no established pharmacological mechanism linking tirzepatide to restless legs syndrome. Patients experiencing new leg symptoms should consult their healthcare provider to evaluate alternative causes, including iron deficiency, medication interactions, or underlying conditions.
Quick Answer: Restless legs syndrome is not listed as a known side effect of tirzepatide in FDA prescribing information or clinical trial data.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide represents a significant advancement in metabolic disease therapy.
The medication works through a dual mechanism of action by simultaneously activating both GIP and GLP-1 receptors. This dual agonism enhances insulin secretion in a glucose-dependent manner, meaning insulin is released only when blood glucose levels are elevated, thereby reducing the risk of hypoglycemia. Additionally, tirzepatide suppresses glucagon secretion, slows gastric emptying, and promotes satiety through central nervous system pathways that regulate appetite.
Clinical trials have demonstrated that tirzepatide produces substantial improvements in glycemic control, with HbA1c reductions of 1.9% to 2.4% at the highest doses in the SURPASS trials. The medication also induces significant weight loss, with patients losing an average of 15% to 21% of their body weight in the SURMOUNT obesity trials, with somewhat lower weight loss observed in patients with type 2 diabetes. Tirzepatide is administered once weekly via subcutaneous injection, with doses starting at 2.5 mg for a 4-week initiation period, then titrating every 4 weeks up to a maximum of 15 mg.
The pharmacokinetic profile of tirzepatide includes a half-life of approximately five days, allowing for convenient weekly dosing. The medication is metabolized through proteolytic cleavage. While dose adjustment is not generally required for mild to moderate renal or hepatic impairment, tirzepatide has not been studied in patients with severe gastrointestinal disease, including severe gastroparesis, and is not recommended in these populations. The medication is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). The delayed gastric emptying may affect absorption of oral medications, including oral contraceptives, potentially requiring additional contraceptive measures.
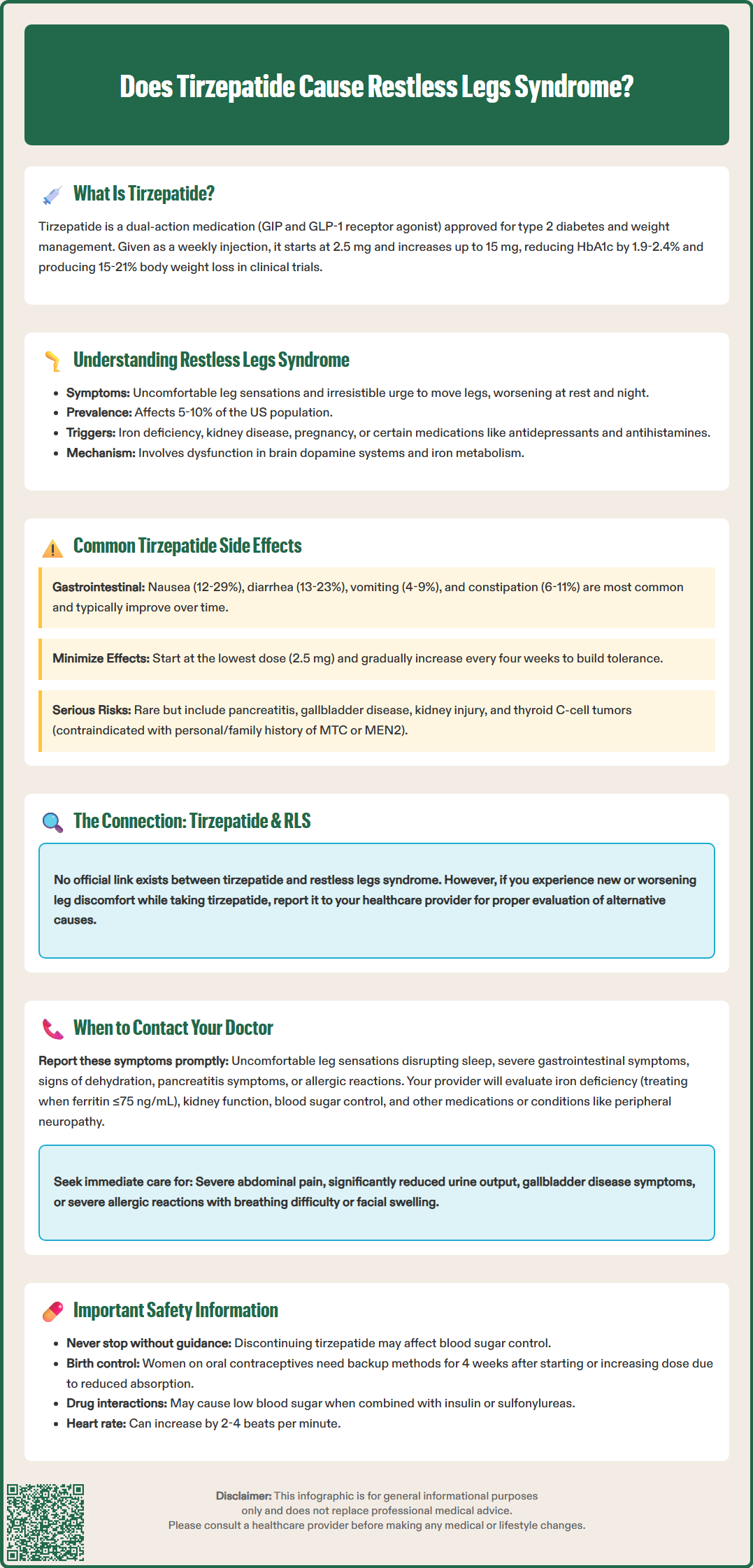
Restless legs syndrome (RLS), also known as Willis-Ekbom disease, is a neurological sensorimotor disorder characterized by an overwhelming urge to move the legs, typically accompanied by uncomfortable sensations. The condition affects approximately 5% to 10% of the US population, though clinically significant cases requiring treatment are less common.
The hallmark symptoms of RLS include:
Uncomfortable leg sensations described as crawling, creeping, pulling, throbbing, aching, or electric-like feelings deep within the legs
Irresistible urge to move the legs to relieve the uncomfortable sensations
Symptom onset or worsening during rest or inactivity, particularly in the evening or at night
Temporary relief with movement such as walking, stretching, or rubbing the legs
Circadian pattern with symptoms typically worsening in the evening and night hours
RLS can be classified as primary (idiopathic) or secondary to underlying conditions. Secondary causes include iron deficiency, end-stage renal disease, pregnancy, peripheral neuropathy, and certain medications. Common medication triggers include antidepressants (particularly SSRIs and SNRIs), antihistamines, dopamine antagonists, and some antipsychotics. The pathophysiology involves dopaminergic dysfunction in the central nervous system and iron metabolism abnormalities in the brain.
Diagnosis is primarily clinical, based on the International Restless Legs Syndrome Study Group criteria. Patients should be evaluated for iron deficiency with serum ferritin levels and transferrin saturation, as iron supplementation can improve symptoms when ferritin is below 75 ng/mL and/or transferrin saturation is below 20%. Other investigations may include assessment of renal function, blood glucose, and vitamin B12 levels. Differential diagnosis includes leg cramps, akathisia, and peripheral neuropathy. The condition can range from mild, occasional symptoms to severe, daily manifestations that profoundly disrupt sleep and daily functioning.
The most frequently reported adverse effects of tirzepatide are gastrointestinal in nature, consistent with the mechanism of action shared by GLP-1 receptor agonists. According to FDA prescribing information and clinical trial data, these side effects are generally dose-dependent and tend to diminish over time as patients develop tolerance to the medication.
Gastrointestinal side effects are the most common and include:
Nausea (reported in 12% to 29% of patients, depending on dose)
Diarrhea (occurring in 13% to 23% of patients)
Vomiting (affecting 4% to 9% of patients)
Constipation (reported in 6% to 11% of patients)
Abdominal pain and dyspepsia (affecting 6% to 9% of patients)
Decreased appetite (common and often contributes to weight loss)
These gastrointestinal symptoms typically occur during dose escalation and often improve with continued use. Patients are advised to start with the lowest dose (2.5 mg) and gradually titrate upward every four weeks to minimize these effects.
Other notable adverse effects include:
Injection site reactions such as erythema, pruritus, or swelling
Fatigue reported in approximately 5% to 6% of patients
Hypoglycemia when used in combination with insulin or sulfonylureas
Increased heart rate with modest elevations of 2 to 4 beats per minute (a class effect of incretin therapies with uncertain clinical significance)
Serious but rare adverse effects include acute pancreatitis, gallbladder disease (cholelithiasis, cholecystitis), acute kidney injury (typically secondary to dehydration from gastrointestinal symptoms), and hypersensitivity reactions. There is a boxed warning regarding thyroid C-cell tumors based on rodent studies, with a contraindication in patients with personal or family history of MTC or MEN2.
Tirzepatide's delayed gastric emptying may affect the absorption of oral medications, including oral contraceptives. Patients using oral contraceptives should use additional contraceptive methods for 4 weeks after initiation and with each dose increase.
Notably, restless legs syndrome is not listed among the common, uncommon, or rare adverse effects in the FDA prescribing information for tirzepatide. There is currently no established pharmacological mechanism by which tirzepatide would be expected to cause or exacerbate RLS symptoms.
While there is no official link between tirzepatide and restless legs syndrome in current medical literature or FDA safety data, patients experiencing new or worsening leg symptoms while taking tirzepatide should discuss these concerns with their healthcare provider. Prompt medical evaluation is important to determine the underlying cause and ensure appropriate management.
Contact your healthcare provider if you experience:
New onset of uncomfortable leg sensations or an irresistible urge to move your legs, particularly if symptoms interfere with sleep or daily activities
Worsening of pre-existing RLS symptoms after starting tirzepatide
Severe or persistent gastrointestinal symptoms including nausea, vomiting, or diarrhea that may lead to dehydration
Signs of dehydration such as decreased urination, dizziness, dry mouth, or fatigue
Symptoms of pancreatitis including severe abdominal pain radiating to the back, nausea, and vomiting
Allergic reactions such as rash, itching, swelling, or difficulty breathing
Seek immediate medical attention for:
Severe abdominal pain that does not resolve
Signs of kidney problems including markedly reduced urine output, sudden weight gain with edema, confusion, or severe dehydration
Symptoms of gallbladder disease such as right upper abdominal pain, fever, or jaundice
Severe allergic reactions with difficulty breathing or swelling of the face, lips, or throat
If you develop leg symptoms while taking tirzepatide, your healthcare provider will likely evaluate for alternative causes of RLS, including iron deficiency (checking serum ferritin and transferrin saturation, with iron therapy often considered when ferritin is ≤75 ng/mL or transferrin saturation <20%), kidney function, blood glucose control, and other medications that may contribute to symptoms. They may also assess whether the symptoms represent a different condition such as peripheral neuropathy, particularly relevant in patients with diabetes. Severe or refractory RLS symptoms may warrant referral to a sleep medicine specialist or neurologist.
Patients should never discontinue tirzepatide without consulting their healthcare provider, as abrupt cessation may affect glycemic control. Women using oral contraceptives should be advised about potential reduced effectiveness and the need for additional contraceptive methods. Unexpected or concerning side effects should be reported to your healthcare provider and may be reported to the FDA MedWatch program. A thorough evaluation can help determine whether symptoms are related to the medication, an underlying condition, or another cause entirely, allowing for appropriate management while maintaining effective diabetes or weight management therapy.
No, restless legs syndrome is not listed among the common, uncommon, or rare adverse effects in FDA prescribing information for tirzepatide. There is currently no established pharmacological mechanism by which tirzepatide would be expected to cause or exacerbate RLS symptoms.
The most common side effects of tirzepatide are gastrointestinal, including nausea (12-29%), diarrhea (13-23%), vomiting (4-9%), constipation (6-11%), and abdominal pain. These symptoms are typically dose-dependent and tend to diminish over time as patients develop tolerance to the medication.
Contact your healthcare provider for evaluation of alternative causes including iron deficiency (checking ferritin and transferrin saturation), kidney function, other medications, or conditions like peripheral neuropathy. Do not discontinue tirzepatide without consulting your provider, as this may affect glycemic control.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.