LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, marketed as Ozempic and Wegovy, is an FDA-approved medication primarily used for type 2 diabetes management and chronic weight management. While not specifically designed as a cholesterol medication, semaglutide does produce modest improvements in lipid profiles as a secondary benefit. Clinical trials consistently demonstrate reductions in total cholesterol, LDL cholesterol, and triglycerides, largely mediated through weight loss. However, these effects are considerably smaller than those achieved with statins, and semaglutide should not replace established lipid-lowering therapies. Understanding how semaglutide affects cholesterol helps patients and providers make informed decisions about cardiovascular risk management.
Quick Answer: Semaglutide produces modest reductions in total cholesterol, LDL cholesterol, and triglycerides as a secondary benefit, primarily through weight loss rather than direct lipid-lowering action.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist primarily approved by the FDA for type 2 diabetes management, chronic weight management, and cardiovascular risk reduction in adults with established cardiovascular disease and overweight or obesity. While not specifically indicated as a cholesterol-lowering medication, semaglutide does produce modest improvements in lipid profiles as a secondary benefit.
The medication works by mimicking the naturally occurring GLP-1 hormone, which enhances glucose-dependent insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite. These effects lead to improved glycemic control and significant weight loss in many patients. The lipid benefits observed with semaglutide appear to be largely mediated through weight reduction, though some direct effects on lipoprotein metabolism may also contribute.
Clinical trials have consistently demonstrated that semaglutide treatment is associated with reductions in total cholesterol, low-density lipoprotein cholesterol (LDL-C), and triglycerides, along with small and sometimes variable changes in high-density lipoprotein cholesterol (HDL-C). The magnitude of these changes is generally proportional to the amount of weight lost during treatment. Patients achieving greater weight reduction typically experience more pronounced improvements in their lipid parameters.
It is important to understand that semaglutide should not be considered a replacement for established lipid-lowering therapies such as statins. Rather, it may provide complementary cardiovascular benefits in appropriate patient populations, particularly those with obesity or type 2 diabetes who have not achieved adequate lipid control with lifestyle modifications and standard pharmacotherapy alone.
The SUSTAIN clinical trial program, which evaluated semaglutide for type 2 diabetes, provides robust evidence regarding its effects on cholesterol and other lipid parameters. Across multiple SUSTAIN trials, patients treated with semaglutide 0.5 mg or 1.0 mg weekly demonstrated statistically significant reductions in total cholesterol and LDL-C compared to placebo and several active comparators.
In the SUSTAIN 6 cardiovascular outcomes trial (published in NEJM 2016), semaglutide reduced the risk of major adverse cardiovascular events (MACE) by 26% compared to placebo in patients with type 2 diabetes and established cardiovascular disease or multiple cardiovascular risk factors. The cardiovascular benefits observed were associated with improved glycemic control and weight loss, though the precise mechanisms contributing to MACE reduction remain under investigation.
The STEP (Semaglutide Treatment Effect in People with obesity) trials evaluated higher doses of semaglutide (2.4 mg weekly) specifically for weight management in individuals without diabetes. STEP 1 (published in NEJM 2021) demonstrated that participants receiving semaglutide 2.4 mg experienced mean reductions in total cholesterol of approximately 5-7%, LDL-C reductions of 5-8%, and triglyceride reductions of 12-15% from baseline. These changes were significantly greater than those observed in the placebo group.
The SELECT trial (published in NEJM 2023) established semaglutide's cardiovascular benefits in patients with established cardiovascular disease and overweight or obesity but without diabetes. This landmark study showed a 20% reduction in MACE with semaglutide 2.4 mg weekly. Subgroup analyses suggested benefits across various baseline characteristics. Based on these results, the FDA approved Wegovy (semaglutide 2.4 mg) in 2024 to reduce the risk of cardiovascular death, heart attack, and stroke in adults with cardiovascular disease and either overweight or obesity.
Meta-analyses of GLP-1 receptor agonist trials consistently show that the lipid-modifying effects of semaglutide are comparable to or slightly better than other medications in this class, likely due to its greater weight loss efficacy.
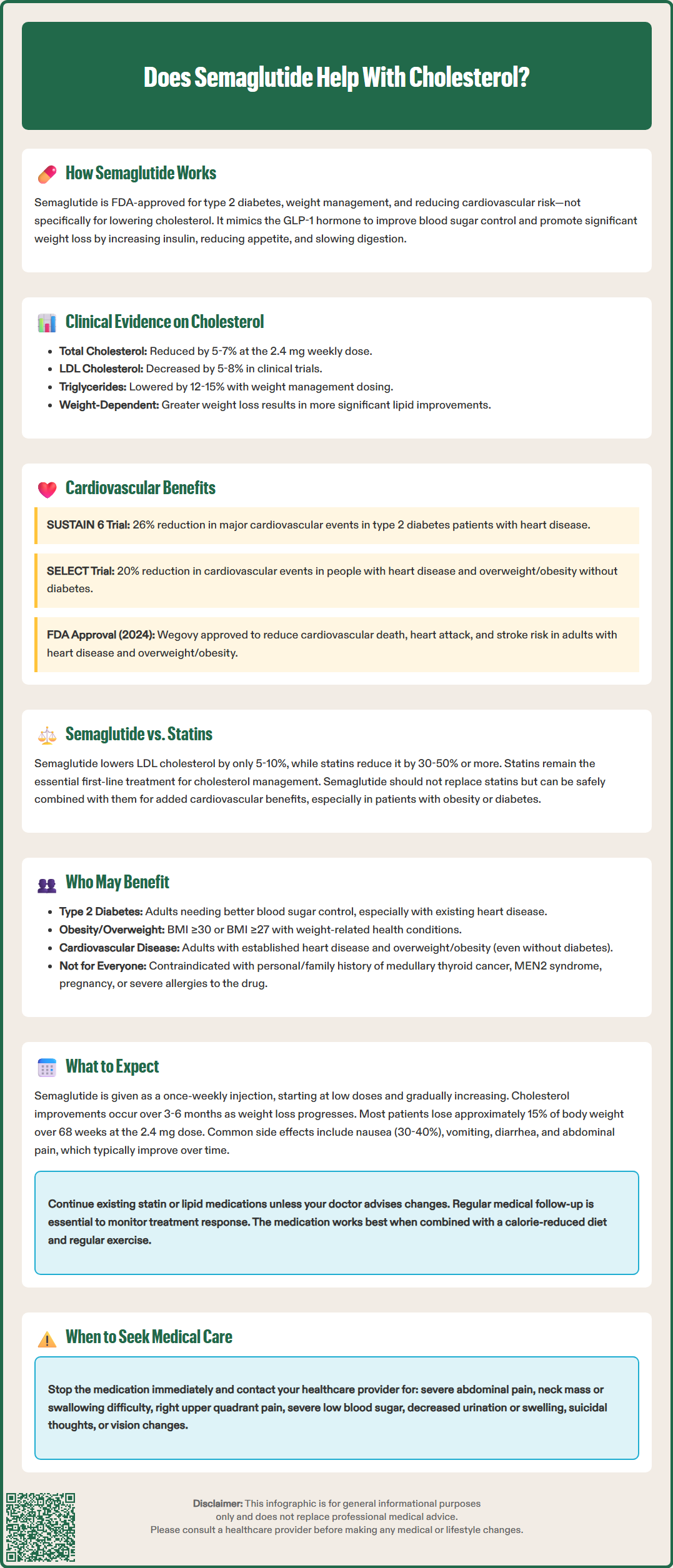
Semaglutide and traditional cholesterol medications such as statins, ezetimibe, and PCSK9 inhibitors work through fundamentally different mechanisms and should not be viewed as interchangeable therapies. Statins remain the cornerstone of lipid management, with extensive evidence demonstrating robust LDL-C reductions and significant cardiovascular event reduction across diverse patient populations.
The lipid-lowering effects of semaglutide are considerably more modest than those achieved with statins. While semaglutide may reduce LDL-C by 5-10%, moderate-intensity statins typically achieve reductions of 30-50%, and high-intensity statins can lower LDL-C by ≥50%. For patients requiring substantial LDL-C lowering to reach guideline-recommended targets, statins or combination lipid therapy remain essential first-line treatments. The American College of Cardiology and American Heart Association guidelines do not currently recommend GLP-1 receptor agonists as primary lipid-lowering agents.
However, semaglutide offers distinct advantages in specific clinical contexts. Unlike statins, which primarily target LDL-C, semaglutide provides multifaceted metabolic benefits including weight loss, improved glycemic control, and blood pressure reduction. These pleiotropic benefits may be particularly valuable for patients with obesity, metabolic syndrome, or type 2 diabetes who have residual cardiovascular risk despite adequate statin therapy.
Combination therapy with semaglutide and statins is common in clinical practice and appears safe and effective. The SELECT trial demonstrated that semaglutide provided cardiovascular benefits even when added to background statin therapy, suggesting complementary rather than redundant mechanisms of action. Patients should not discontinue established lipid-lowering medications when initiating semaglutide unless specifically directed by their healthcare provider.
Cost considerations are also relevant. Semaglutide is significantly more expensive than generic statins, with costs varying considerably depending on insurance coverage, dose, and formulation. This economic factor, combined with its modest direct lipid effects, reinforces that semaglutide should be prescribed primarily for its approved indications rather than as a cholesterol medication.
Semaglutide may provide cardiovascular and lipid benefits for specific patient populations, though it should be prescribed according to its FDA-approved indications. The medication is most appropriate for adults with type 2 diabetes who require improved glycemic control, or for individuals with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity.
Patients with type 2 diabetes and established atherosclerotic cardiovascular disease represent a particularly appropriate population for semaglutide therapy. The SUSTAIN 6 trial specifically demonstrated cardiovascular benefits in this high-risk group. For these patients, semaglutide addresses multiple cardiovascular risk factors simultaneously—hyperglycemia, excess weight, and modestly elevated lipids—while reducing the risk of major cardiovascular events.
Individuals with obesity or overweight who have metabolic syndrome may also benefit from semaglutide's effects on lipid profiles and cardiovascular risk factors. Metabolic syndrome, characterized by abdominal obesity, elevated triglycerides, low HDL-C, hypertension, and insulin resistance, confers increased cardiovascular risk. Semaglutide's ability to promote weight loss and improve multiple metabolic parameters makes it a valuable therapeutic option for this population.
Adults with established cardiovascular disease and overweight or obesity without diabetes now have an FDA-approved indication for Wegovy (semaglutide 2.4 mg) to reduce the risk of cardiovascular death, heart attack, and stroke, based on the SELECT trial results. Insurance coverage for this indication may vary, and patients should discuss coverage with their healthcare provider and insurance plan.
Patients who may not be appropriate candidates include:
Individuals with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2
Those with a history of severe hypersensitivity reactions to semaglutide
Patients with a history of pancreatitis (relative contraindication requiring careful risk-benefit assessment)
Pregnant women or those planning pregnancy (contraindicated for weight management; discontinue at least 2 months before planned conception)
Individuals seeking cholesterol management as the sole therapeutic goal without diabetes or obesity
Patients already taking another GLP-1 receptor agonist
Healthcare providers should conduct comprehensive cardiovascular risk assessment and ensure patients meet appropriate criteria before prescribing semaglutide. Patients with diabetes should be monitored for diabetic retinopathy complications, particularly if they have pre-existing retinopathy.
Patients initiating semaglutide should understand both the potential benefits and common adverse effects associated with treatment. The medication is administered as a once-weekly subcutaneous injection, typically started at a low dose (0.25 mg weekly for diabetes; 0.25 mg weekly for weight management) and gradually titrated upward over several weeks to months to minimize gastrointestinal side effects.
Common adverse effects include:
Nausea (reported by 30-40% of patients at the 2.4 mg dose)
Vomiting
Diarrhea
Constipation
Abdominal pain
Decreased appetite
These gastrointestinal symptoms are typically most pronounced during dose escalation and often improve with continued treatment. Eating smaller, more frequent meals and avoiding high-fat foods may help minimize these effects. Patients should be counseled that these symptoms, while uncomfortable, are generally not dangerous and tend to resolve over time.
Regarding lipid changes, patients should not expect dramatic or immediate improvements in cholesterol levels. Lipid benefits typically emerge gradually over 3-6 months as weight loss progresses. Healthcare providers should monitor lipid panels at baseline, 4-12 weeks after therapy changes, and then every 3-12 months according to ACC/AHA guidance. Patients already taking statins or other lipid-lowering medications should continue these treatments unless their provider recommends adjustments based on follow-up laboratory results.
Weight loss with semaglutide is typically progressive, with most patients losing approximately 15% of body weight over 68 weeks at the 2.4 mg dose in clinical trials. This weight reduction is the primary driver of lipid improvements, so patients who do not achieve significant weight loss may see minimal changes in their cholesterol levels.
Patients should seek immediate medical attention for and discontinue semaglutide if they experience:
Severe, persistent abdominal pain (possible pancreatitis)
Signs of thyroid tumors (neck mass, difficulty swallowing, persistent hoarseness)
Symptoms of gallbladder disease (right upper quadrant pain, especially after meals)
Severe hypoglycemia (when combined with insulin or sulfonylureas)
Signs of kidney problems (decreased urination, swelling, fatigue)
Suicidal thoughts or behaviors (particularly with Wegovy)
Vision changes (especially in patients with diabetes and pre-existing retinopathy)
Regular follow-up with healthcare providers is essential to monitor treatment response, adjust dosing, manage side effects, and assess cardiovascular risk factors including blood pressure, glucose control, and lipid profiles. Semaglutide is most effective when combined with lifestyle modifications including a balanced, calorie-reduced diet and regular physical activity.
No, semaglutide should not replace statins for cholesterol management. While semaglutide reduces LDL cholesterol by 5-10%, statins achieve much greater reductions of 30-50% and remain the cornerstone of lipid therapy according to ACC/AHA guidelines.
Lipid benefits from semaglutide typically emerge gradually over 3-6 months as weight loss progresses. Healthcare providers should monitor lipid panels at baseline, 4-12 weeks after starting therapy, and then every 3-12 months.
Patients with type 2 diabetes and cardiovascular disease, or individuals with obesity and metabolic syndrome, are most likely to benefit from semaglutide's lipid effects. The medication addresses multiple cardiovascular risk factors simultaneously, including weight, blood sugar, and modestly elevated lipids.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.