LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide, marketed as Mounjaro for type 2 diabetes and Zepbound for weight management, has generated questions about potential effects beyond its FDA-approved indications. While this dual GIP/GLP-1 receptor agonist produces substantial metabolic improvements and weight reduction, does tirzepatide help with acne? Currently, no direct pharmacological connection exists between tirzepatide and acne treatment. However, the medication's metabolic effects—particularly improvements in insulin sensitivity and hormonal balance—may indirectly influence acne in certain patients with obesity-related hormonal imbalances. Understanding tirzepatide's mechanisms and realistic expectations is essential for patients considering this therapy.
Quick Answer: Tirzepatide has no direct effect on acne, but may indirectly improve acne in some patients through metabolic improvements that normalize insulin and androgen levels associated with obesity.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide represents a significant advancement in metabolic disease therapy due to its dual incretin receptor activity.
The medication works through multiple complementary mechanisms. As a GLP-1 receptor agonist, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon release, and slows gastric emptying. The additional GIP receptor agonism appears to augment insulin secretion further and may contribute to improved lipid metabolism and enhanced satiety signaling. These combined actions result in improved glycemic control in patients with type 2 diabetes and substantial weight reduction in both diabetic and non-diabetic individuals with obesity.
Tirzepatide is administered as a once-weekly subcutaneous injection, with dosing typically initiated at 2.5 mg (an initiation dose not intended for glycemic control) and gradually titrated upward based on therapeutic response and tolerability. Maximum approved doses are 15 mg weekly for diabetes management and up to 15 mg weekly for chronic weight management. For weight management, tirzepatide (Zepbound) is indicated for adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity, and should be used in conjunction with a reduced-calorie diet and increased physical activity.
Clinical trials have demonstrated that tirzepatide produces average weight loss of 15-22% of body weight over 72 weeks in non-diabetic adults with obesity (SURMOUNT-1 trial), with somewhat smaller weight reductions typically observed in people with type 2 diabetes (SURPASS trials). Alongside significant improvements in hemoglobin A1c levels in diabetic patients, these metabolic improvements have generated interest in potential secondary benefits beyond glucose control and weight reduction, though additional research is needed to establish effects on cardiovascular outcomes, liver health, and other systems.
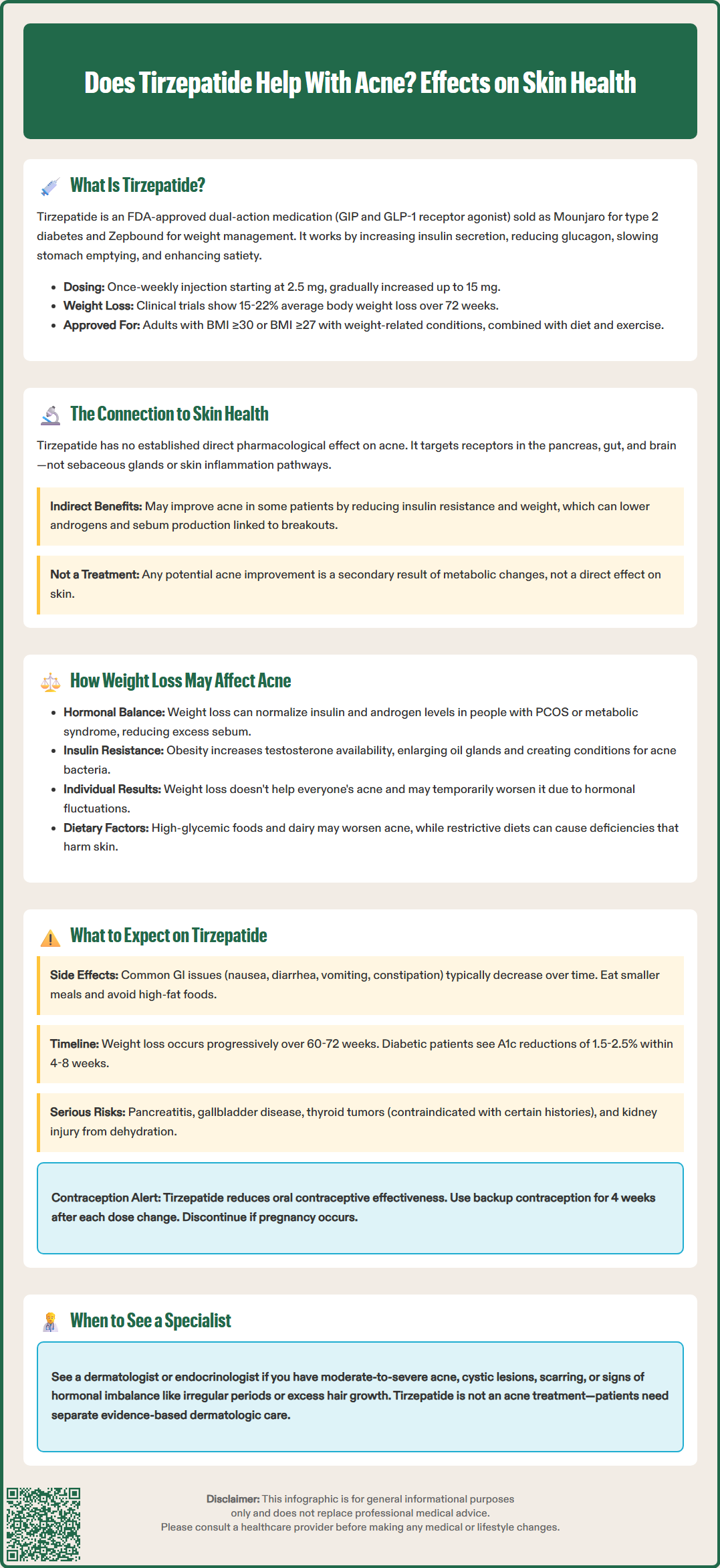
Currently, there is no established direct pharmacological connection between tirzepatide and acne improvement based on the medication's mechanism of action or FDA-approved prescribing information. Tirzepatide's primary targets—the GIP and GLP-1 receptors—are predominantly expressed in pancreatic islet cells, the gastrointestinal tract, and central nervous system regions involved in appetite regulation. While GLP-1 receptors have been identified in various tissues throughout the body, there is limited evidence that tirzepatide directly influences sebaceous gland function, androgen metabolism in the skin, or the inflammatory pathways central to acne pathogenesis.
The FDA prescribing information for tirzepatide does not list acne as either an adverse effect or a therapeutic benefit. Dermatologic adverse events reported in clinical trials were primarily injection site reactions, which typically resolved without intervention. Other potential dermatologic adverse reactions include hypersensitivity reactions such as rash and, rarely, anaphylaxis or angioedema.
However, the indirect metabolic effects of tirzepatide may theoretically influence factors associated with acne development in certain patient populations. Obesity and insulin resistance are linked to hormonal imbalances—particularly hyperinsulinemia and elevated androgens—that can exacerbate acne through increased sebum production and altered keratinization. By improving insulin sensitivity and facilitating weight loss, tirzepatide might indirectly modify these hormonal contributors to acne in susceptible individuals.
It is important to emphasize that any potential skin-related benefits would be secondary consequences of metabolic improvement rather than direct dermatologic effects. Tirzepatide has no FDA-approved dermatologic indications. Patients considering tirzepatide should not expect it to function as an acne treatment, and those experiencing acne should pursue evidence-based dermatologic therapies under appropriate specialist guidance.
The relationship between weight loss and acne is complex and varies considerably among individuals based on underlying hormonal status, acne etiology, and the specific mechanisms through which weight reduction occurs. In patients with obesity-related hormonal imbalances—particularly those with polycystic ovary syndrome (PCOS) or metabolic syndrome—significant weight loss can lead to improvements in acne severity through normalization of insulin and androgen levels.
Insulin resistance, common in obesity, stimulates ovarian and adrenal androgen production while reducing sex hormone-binding globulin (SHBG) levels, resulting in increased bioavailable testosterone. Elevated androgens promote sebaceous gland hypertrophy and increased sebum production, creating an environment conducive to Cutibacterium acnes proliferation and inflammatory acne lesions. Weight loss interventions that improve insulin sensitivity—whether through lifestyle modification, bariatric surgery, or pharmacotherapy—can reduce hyperinsulinemia and subsequently decrease androgen excess, potentially improving acne in hormonally-driven cases.
However, weight loss does not universally improve acne and may occasionally worsen skin conditions during the initial phases of treatment. Some individuals may experience temporary hormonal fluctuations during active weight loss. Additionally, dietary changes accompanying weight loss efforts may independently influence acne. According to American Academy of Dermatology guidelines, high-glycemic foods and possibly dairy consumption may exacerbate acne in some individuals. Nutritional deficiencies resulting from restrictive diets or malabsorption can also compromise skin health.
For medications like tirzepatide that produce substantial weight loss, the dermatologic effects will likely mirror those seen with other effective weight loss interventions. Patients with metabolic syndrome or PCOS may experience gradual acne improvement as insulin sensitivity normalizes over several months. Conversely, individuals whose acne is primarily driven by genetic factors, bacterial colonization, or non-hormonal inflammation may see little change in their skin condition despite significant weight reduction.
Patients with moderate-to-severe acne, cystic or nodular lesions, scarring, or acne accompanied by signs of hormonal imbalance (irregular menstrual cycles, hirsutism) should be referred to dermatology or endocrinology specialists for comprehensive evaluation and treatment.
Patients initiating tirzepatide for FDA-approved indications—type 2 diabetes or chronic weight management—should have realistic expectations regarding both intended therapeutic effects and potential adverse events. The medication requires gradual dose titration over several months to minimize gastrointestinal side effects, which are the most common tolerability concerns. Nausea, diarrhea, decreased appetite, vomiting, and constipation occur in a dose-dependent manner, with higher rates at maximum doses, and typically diminish in severity as treatment continues.
Weight loss with tirzepatide occurs progressively, with most patients experiencing steady reduction over 60-72 weeks. In non-diabetic adults with obesity (SURMOUNT-1 trial), average weight loss ranges from 15-22% of baseline body weight at maximum doses, while somewhat smaller reductions are typically seen in people with type 2 diabetes. Glycemic improvements in diabetic patients typically manifest within 4-8 weeks, with hemoglobin A1c reductions of 1.5-2.5% commonly observed. Patients should maintain regular follow-up appointments for monitoring of glycemic control, weight trends, and potential adverse effects.
Important safety considerations include:
Gastrointestinal symptoms: Eating smaller, more frequent meals and avoiding high-fat foods may reduce nausea and vomiting
Hypoglycemia risk: Particularly when combined with insulin or sulfonylureas; dose adjustments of concomitant medications may be necessary
Gallbladder disease: Rapid weight loss increases cholelithiasis risk; patients should report right upper quadrant pain promptly
Pancreatitis: Severe, persistent abdominal pain warrants immediate medical evaluation; tirzepatide should be discontinued if pancreatitis is suspected and not restarted if confirmed
Thyroid concerns: Tirzepatide carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies; it is contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2
Acute kidney injury: Risk increases with severe gastrointestinal adverse reactions that cause dehydration; patients should maintain adequate fluid intake
Contraception: Tirzepatide may reduce the effectiveness of oral hormonal contraceptives during initiation and dose escalation; non-oral or backup contraception is recommended for 4 weeks after each dose increase
Pregnancy/lactation: Weight loss therapy is not recommended during pregnancy; tirzepatide should be discontinued if pregnancy occurs
Severe gastrointestinal disease: Tirzepatide is not recommended for patients with severe gastrointestinal disease, including gastroparesis
Regarding skin-related expectations, patients should not anticipate tirzepatide to function as an acne treatment. While some individuals with obesity-related hormonal imbalances may experience gradual skin improvements as metabolic parameters normalize, this is neither predictable nor universal. Patients with significant acne concerns should pursue concurrent evidence-based dermatologic care, which may include topical retinoids, benzoyl peroxide, topical or oral antibiotics, hormonal therapies, or isotretinoin depending on acne severity and type. Any skin changes—whether improvement or worsening—should be discussed with healthcare providers to determine appropriate management strategies and ensure changes are not indicative of adverse reactions requiring intervention.
No, tirzepatide has no FDA-approved dermatologic indications and should not be prescribed for acne treatment. Patients with acne should pursue evidence-based dermatologic therapies under appropriate specialist guidance.
Patients with obesity-related hormonal imbalances, particularly those with PCOS or metabolic syndrome, may experience gradual acne improvement as tirzepatide-induced weight loss normalizes insulin sensitivity and reduces androgen excess. This is an indirect metabolic effect rather than a direct dermatologic action.
Tirzepatide is FDA-approved for treating type 2 diabetes mellitus (as Mounjaro) and chronic weight management in adults with obesity or overweight with weight-related comorbidities (as Zepbound), used alongside reduced-calorie diet and increased physical activity.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.