LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management. As patients and clinicians consider this medication, understanding its effects on digestion becomes essential for setting expectations and managing potential side effects. Yes, tirzepatide does slow gastric emptying as part of its mechanism of action, which contributes to both its therapeutic benefits and gastrointestinal adverse effects. This delayed gastric emptying helps regulate blood glucose levels and promotes satiety, but it also requires careful patient education and monitoring to ensure safe, effective treatment outcomes.
Quick Answer: Yes, tirzepatide slows gastric emptying as part of its pharmacological mechanism, delaying food movement from the stomach to the small intestine.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). This novel medication activates both GIP and GLP-1 receptors, which are incretin hormones naturally produced in the gastrointestinal tract in response to food intake.
The mechanism of action involves multiple pathways that contribute to glycemic control and weight reduction. Tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and reduces hepatic glucose production. These effects work synergistically to improve blood glucose levels in patients with type 2 diabetes.
Yes, tirzepatide does slow gastric emptying as part of its pharmacological action. This delayed gastric emptying contributes to the medication's therapeutic benefits but can also cause gastrointestinal adverse effects and affect the absorption of some oral medications. By slowing the rate at which food moves from the stomach into the small intestine, tirzepatide helps regulate postprandial glucose excursions and promotes satiety.
The medication also acts centrally on appetite regulation centers in the hypothalamus, reducing food intake and promoting weight loss. The combination of delayed gastric emptying, enhanced satiety, and improved glucose-dependent insulin secretion makes tirzepatide effective for patients requiring both glycemic control and weight management.
Important safety considerations include a boxed warning for thyroid C-cell tumors (contraindicated in patients with Multiple Endocrine Neoplasia syndrome type 2), and risks of pancreatitis, gallbladder disease, acute kidney injury from dehydration, and hypoglycemia when used with insulin or sulfonylureas. Tirzepatide is not recommended for patients with severe gastroparesis.
Clinical trial data from the SURPASS program and SURMOUNT studies provide robust evidence regarding tirzepatide's effects on gastric emptying and digestive function. In pharmacodynamic studies, tirzepatide demonstrated dose-dependent slowing of gastric emptying, with the effect being most pronounced during the early treatment period and showing some attenuation over time with continued use.
The SURPASS-1 through SURPASS-5 trials, which enrolled over 6,000 patients with type 2 diabetes, consistently reported gastrointestinal adverse events as the most common side effects. According to the FDA prescribing information, nausea occurred in 12-24% of patients, vomiting in 2-11%, and diarrhea in 7-17%, with rates varying by dose (5 mg, 10 mg, or 15 mg weekly). These symptoms were generally mild to moderate in severity and typically occurred during dose escalation phases.
Importantly, gastric emptying studies have shown that while tirzepatide significantly delays gastric emptying initially, this effect may diminish somewhat with chronic administration. This phenomenon, known as tachyphylaxis, has been observed with other GLP-1 receptor agonists as well. Despite this partial attenuation, the medication maintains its glucose-lowering and weight-reducing effects throughout long-term treatment.
The SURMOUNT trials, which evaluated tirzepatide specifically for weight management in patients without diabetes, reported similar gastrointestinal tolerability profiles. Approximately 80-90% of gastrointestinal adverse events occurred during the dose-escalation period, and most resolved within 4-8 weeks. Discontinuation rates due to gastrointestinal side effects ranged from 4-7% across clinical trials, indicating that most patients can tolerate the medication with appropriate management strategies. Rare but serious gastrointestinal events, including ileus, have been reported in clinical trials. These findings support the use of gradual dose titration to minimize digestive symptoms while achieving therapeutic benefits.
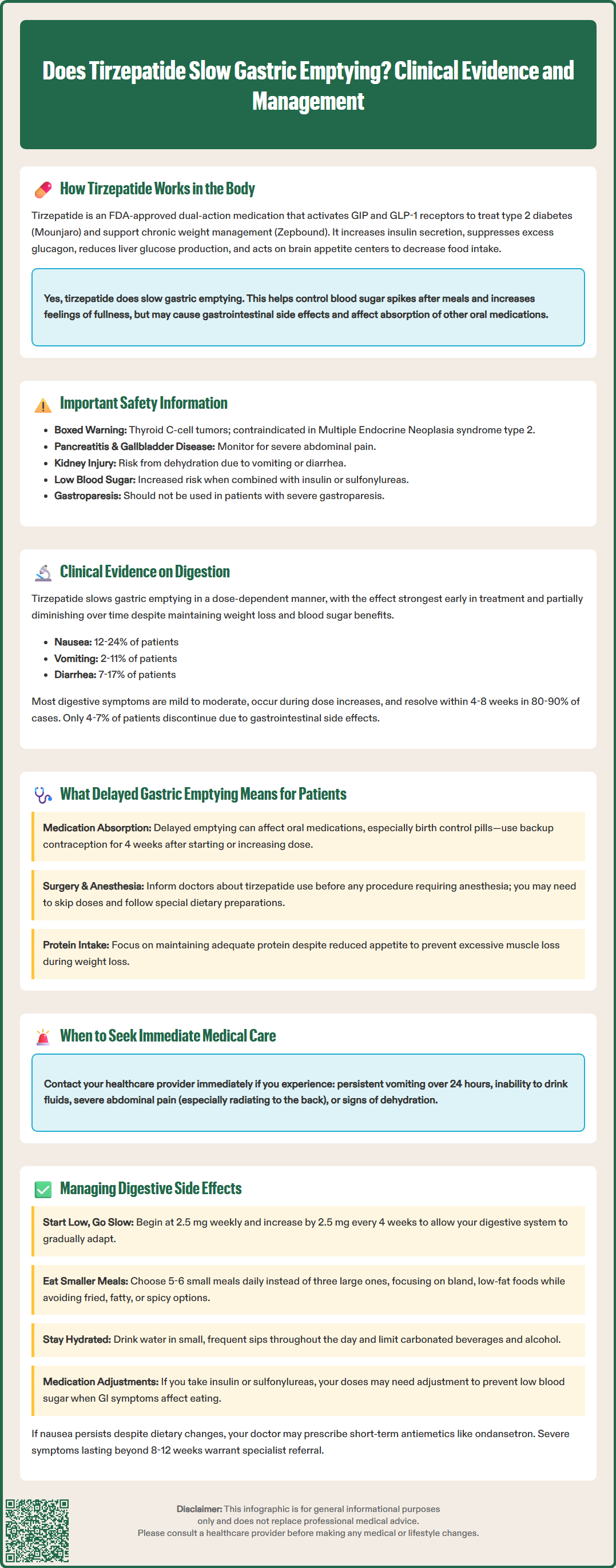
Delayed gastric emptying, or gastroparesis-like symptoms, can significantly impact patients' daily lives and nutritional status. When tirzepatide slows the movement of food from the stomach to the small intestine, patients may experience a range of digestive symptoms including early satiety, postprandial fullness, bloating, nausea, and occasionally vomiting. Understanding these effects helps patients set realistic expectations and recognize normal versus concerning symptoms.
For many patients, the delayed gastric emptying contributes positively to weight loss goals by promoting prolonged satiety and reducing overall caloric intake. Patients often report feeling fuller for longer periods after meals, which can facilitate adherence to reduced-calorie eating patterns. However, this same mechanism can make it challenging to consume adequate nutrition, particularly protein and fiber, which are essential for maintaining lean body mass during weight loss.
Patients should be aware of several practical implications of slowed gastric emptying:
Meal timing and medication absorption: Delayed gastric emptying may affect the absorption of oral medications, particularly those requiring rapid absorption or those taken with food. Notably, tirzepatide can reduce the exposure of oral contraceptives during initiation and dose escalation; backup non-oral/barrier contraception is recommended for 4 weeks after initiation and each dose increase.
Nutritional adequacy: Reduced appetite and early satiety may lead to inadequate protein intake, vitamin deficiencies, or excessive muscle loss if not properly managed.
Procedural considerations: Patients scheduled for endoscopy or surgery requiring anesthesia should inform their healthcare team about tirzepatide use. Current guidelines recommend risk stratification and potentially holding doses before procedures, following a liquid diet, and considering point-of-care gastric ultrasound in high-risk patients.
Certain symptoms warrant immediate medical evaluation. Patients should seek prompt care if they experience: persistent vomiting lasting more than 24 hours; inability to tolerate liquids; severe abdominal pain (especially if radiating to the back, which may indicate pancreatitis); right upper quadrant pain, fever or jaundice (possible gallbladder disease); signs of dehydration; or blood in vomit. Tirzepatide should be discontinued pending assessment of these serious symptoms.
Effective management of gastrointestinal side effects is essential for treatment adherence and patient comfort. The FDA-approved prescribing information recommends initiating tirzepatide at 2.5 mg subcutaneously once weekly, with dose increases of 2.5 mg increments every 4 weeks as tolerated. For Mounjaro (diabetes), the target dose is typically 5-15 mg weekly, while Zepbound (weight management) may be titrated up to 15 mg with intermediate steps. This gradual titration schedule allows the digestive system to adapt to the medication's effects on gastric emptying.
Dietary modifications can substantially reduce digestive discomfort:
Consume smaller, more frequent meals (5-6 times daily) rather than three large meals
Choose bland, low-fat foods during the initial treatment period and after dose increases
Avoid high-fat, fried, or heavily spiced foods that delay gastric emptying further
Stay well-hydrated with small, frequent sips of water throughout the day
Limit carbonated beverages and alcohol, which may exacerbate nausea and bloating
Eat slowly and chew food thoroughly to reduce the volume of food in the stomach
Avoid or limit medications that further slow gastric emptying (opioids, anticholinergics)
Pharmacological interventions may be appropriate for patients with persistent symptoms despite dietary modifications. However, routine prophylactic use of antiemetics is not recommended. If nausea becomes problematic, healthcare providers may consider short-term use of ondansetron or, in select cases, metoclopramide (5-10 mg). Metoclopramide carries an FDA boxed warning for tardive dyskinesia and should be used for the shortest duration possible, typically less than 12 weeks.
Patients taking insulin or sulfonylureas may need dose reductions of these medications to prevent hypoglycemia when GI symptoms affect food intake, per American Diabetes Association guidance.
Patients experiencing severe or persistent gastrointestinal symptoms may benefit from temporarily holding the next dose or reducing to a previously tolerated dose. For persistent symptoms, clinicians may consider laboratory evaluation (electrolytes, kidney function, lipase), right upper quadrant ultrasound for biliary symptoms, or gastric emptying scintigraphy. Referral to a gastroenterologist is appropriate for symptoms that persist beyond 8-12 weeks despite management strategies.
With appropriate management strategies, most patients can successfully continue tirzepatide therapy while minimizing digestive side effects.
Most gastrointestinal side effects occur during dose escalation and typically resolve within 4-8 weeks. Approximately 80-90% of these symptoms occur during the dose-escalation period, with discontinuation rates due to GI effects ranging from 4-7% across clinical trials.
Yes, delayed gastric emptying from tirzepatide may affect absorption of oral medications, particularly those requiring rapid absorption. Notably, tirzepatide can reduce oral contraceptive exposure, and backup non-oral or barrier contraception is recommended for 4 weeks after initiation and each dose increase.
Patients should inform their healthcare team about tirzepatide use before procedures requiring anesthesia. Current guidelines recommend risk stratification and potentially holding doses before procedures, following a liquid diet, and considering point-of-care gastric ultrasound in high-risk patients.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.