LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Why does tirzepatide work for me? Tirzepatide's effectiveness stems from its unique dual-action mechanism targeting both GIP and GLP-1 receptors, addressing multiple aspects of metabolic dysfunction simultaneously. This FDA-approved medication works differently in each person based on genetic factors, baseline metabolic health, lifestyle habits, and individual physiology. Understanding how tirzepatide interacts with your body's systems—from insulin secretion and appetite regulation to gastric emptying—helps explain why you may experience significant improvements in blood sugar control and weight management. Your individual response depends on factors including pancreatic function, medication adherence, dietary choices, and concurrent health conditions.
Quick Answer: Tirzepatide works for you by activating both GIP and GLP-1 receptors to improve insulin secretion, reduce appetite, slow gastric emptying, and decrease glucose production.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). This medication works through multiple complementary mechanisms that address the underlying metabolic dysfunction in these conditions.
When you take tirzepatide, it activates both GIP and GLP-1 receptors throughout your body. The GLP-1 component stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released primarily when blood sugar levels are elevated. Simultaneously, tirzepatide suppresses glucagon secretion from pancreatic alpha cells, which decreases hepatic glucose production. The GIP receptor activation may contribute to improved metabolic effects, though the precise contribution of each pathway continues to be studied.
Beyond glycemic control, tirzepatide significantly affects appetite regulation and gastric emptying. It acts on receptors in the hypothalamus and brainstem to reduce hunger signals and increase satiety. The medication also slows gastric emptying, which prolongs the feeling of fullness after meals and reduces postprandial glucose excursions. These combined effects explain why tirzepatide produces substantial weight loss—up to approximately 21% of body weight in adults without diabetes at the 15 mg dose in clinical trials, with somewhat lower averages in people with type 2 diabetes—alongside improvements in hemoglobin A1c levels.
The dual agonist mechanism distinguishes tirzepatide from single GLP-1 receptor agonists like semaglutide. This multifaceted approach addresses several aspects of metabolic disease simultaneously, which may explain its effectiveness for many patients. Important safety considerations include: tirzepatide is not indicated for type 1 diabetes or treatment of diabetic ketoacidosis, and it is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). The risk of hypoglycemia increases when tirzepatide is used with insulin or sulfonylureas.
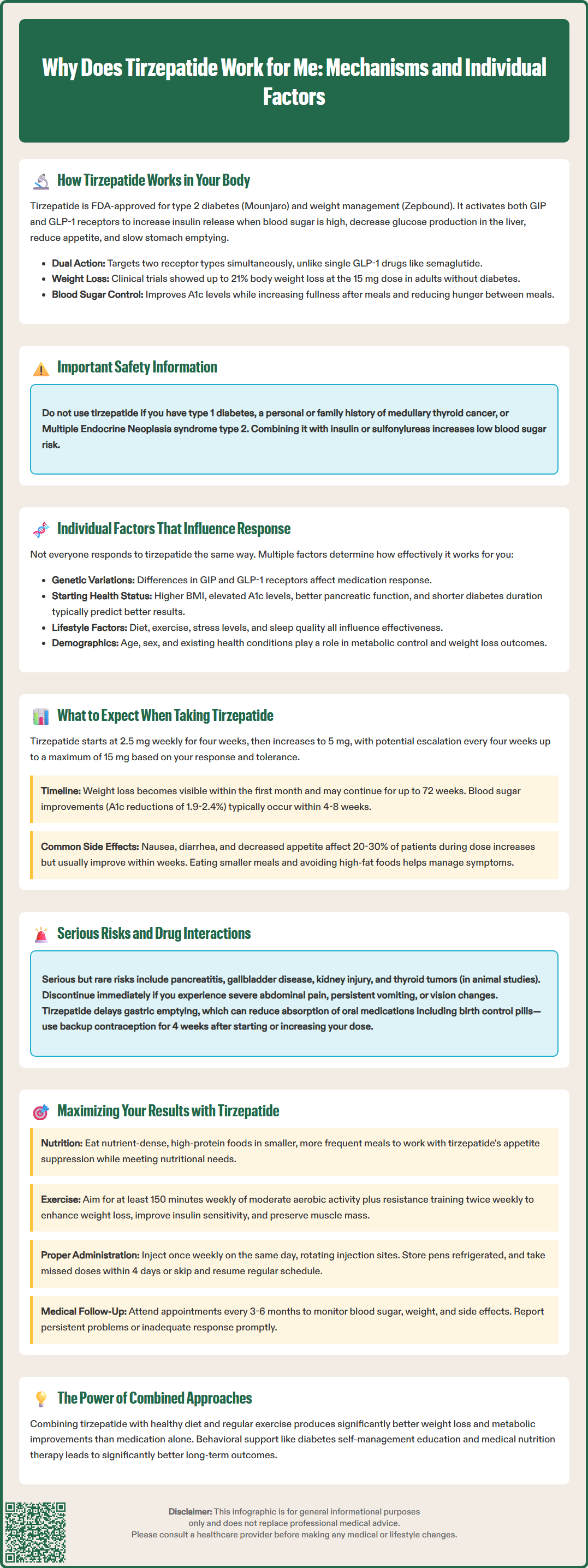
Your response to tirzepatide depends on numerous individual factors, and understanding these variables helps explain why outcomes vary among patients. Genetic differences in receptor expression and function can influence how effectively tirzepatide binds to GIP and GLP-1 receptors in your tissues. Some individuals naturally have variations in these receptors that may enhance or diminish the medication's effects, though genetic testing for tirzepatide response is not currently part of routine clinical practice.
Baseline metabolic characteristics significantly impact treatment outcomes. Patients with higher initial body mass index (BMI) and hemoglobin A1c levels often experience more dramatic absolute improvements, though percentage changes may be similar across groups. Your pancreatic beta cell function also matters—individuals with substantial residual insulin secretion capacity typically respond better than those with advanced beta cell dysfunction. Duration of diabetes affects response as well; earlier intervention generally yields better glycemic outcomes than treatment initiated after years of poorly controlled disease.
Lifestyle factors interact substantially with tirzepatide's pharmacological effects. Adherence to dietary modifications and physical activity recommendations enhances weight loss and metabolic improvements. Patients who combine tirzepatide with structured lifestyle interventions consistently achieve superior results compared to medication alone. Certain medications may interfere with tirzepatide's effectiveness—particularly drugs that affect gastric motility or glucose metabolism.
Physiological variables including age, sex, and concurrent medical conditions influence treatment response. Gastrointestinal disorders may affect tolerability, though absorption is not affected since tirzepatide is administered subcutaneously. No dose adjustment is recommended for any stage of renal or hepatic impairment, though monitoring renal function is advised if significant gastrointestinal adverse effects occur. Psychological factors, including stress levels and sleep quality, affect metabolic regulation and may modulate treatment outcomes. Importantly, tirzepatide can reduce the effectiveness of oral medications, including oral contraceptives, due to delayed gastric emptying—using alternative or back-up contraception for 4 weeks after starting or increasing your dose is recommended.
Tirzepatide treatment follows a structured dose escalation schedule designed to minimize gastrointestinal side effects while achieving therapeutic efficacy. The FDA-approved regimen begins with 2.5 mg subcutaneously once weekly for four weeks, serving as an initiation dose rather than a therapeutic dose. Your healthcare provider will then increase the dose to 5 mg weekly, with potential further increases every four weeks (to 7.5 mg, 10 mg, 12.5 mg, or maximum 15 mg) based on your glycemic response, weight loss progress, and tolerability. This titration schedule is similar for both Mounjaro (diabetes indication) and Zepbound (weight management indication).
Gastrointestinal side effects are the most common adverse reactions, particularly during dose escalation. Nausea affects approximately 20-30% of patients and typically diminishes over several weeks as your body adapts. Other frequent effects include diarrhea, decreased appetite, vomiting, constipation, and abdominal discomfort. These symptoms are generally mild to moderate and transient. Eating smaller, more frequent meals and avoiding high-fat foods can help manage these effects. If symptoms become severe or persistent, contact your healthcare provider—dose reduction or temporary treatment interruption may be necessary.
Weight loss typically becomes noticeable within the first month, with progressive reductions that may continue for up to 72 weeks based on clinical trials. Glycemic improvements often occur more rapidly, with measurable hemoglobin A1c reductions within 4-8 weeks. Clinical trials demonstrate average A1c reductions of 1.9-2.4% from baseline, with many patients achieving target levels below 7%. Individual response varies considerably; some patients experience dramatic improvements while others show more modest benefits.
Serious adverse effects are uncommon but require awareness. Tirzepatide carries warnings for thyroid C-cell tumors (based on rodent studies), acute pancreatitis, gallbladder disease, acute kidney injury, severe gastrointestinal disease, and diabetic retinopathy complications. Tirzepatide should be discontinued if pancreatitis is suspected or confirmed. The risk of hypoglycemia increases when used with insulin or sulfonylureas; dose reductions of these medications may be necessary. Tirzepatide is not recommended during pregnancy, and women of reproductive potential should discuss contraception with their healthcare provider. Seek immediate medical attention for severe abdominal pain, persistent vomiting, signs of pancreatitis, or visual changes.
Optimizing tirzepatide outcomes requires a comprehensive approach that extends beyond medication administration. Dietary modifications work synergistically with tirzepatide's appetite-suppressing effects. Focus on nutrient-dense, high-protein foods that promote satiety while meeting nutritional needs despite reduced caloric intake. The American Diabetes Association recommends individualized medical nutrition therapy, emphasizing whole grains, vegetables, lean proteins, and healthy fats while limiting processed foods and added sugars. Given tirzepatide's effect on gastric emptying, smaller, more frequent meals often improve tolerability and help maintain consistent energy levels throughout the day.
Physical activity enhances both weight loss and glycemic control when combined with tirzepatide. The American Diabetes Association and U.S. Department of Health and Human Services recommend at least 150 minutes of moderate-intensity aerobic activity weekly, plus resistance training twice weekly. Exercise improves insulin sensitivity, preserves lean muscle mass during weight loss, and provides cardiovascular benefits independent of weight reduction. Start gradually if you're currently sedentary, and consult your healthcare provider before beginning vigorous exercise programs, particularly if you have cardiovascular disease or diabetic complications.
Medication adherence is critical for sustained benefits. Tirzepatide requires once-weekly subcutaneous injection, ideally on the same day each week. Proper injection technique and site rotation (abdomen, thigh, or upper arm) minimize injection site reactions. Store unused pens in the refrigerator (36-46°F or 2-8°C), do not freeze, and protect from light. Pens may be kept at room temperature (up to 86°F/30°C) for a limited time per product labeling. If you miss a dose, administer it within four days; if more than four days have passed, skip that dose and resume your regular schedule. Never take two doses within 72 hours.
Regular monitoring and communication with your healthcare team optimize long-term outcomes. Schedule follow-up appointments as recommended—typically every 3-6 months—for assessment of glycemic control, weight trends, side effects, and complications screening. Blood glucose monitoring frequency depends on your diabetes regimen; patients on insulin or with hypoglycemia risk require more frequent testing. Report persistent side effects, inadequate response, or new symptoms promptly. If you're planning surgery or procedures, discuss tirzepatide with your healthcare team due to its effects on gastric emptying. Behavioral support, including diabetes self-management education and medical nutrition therapy, significantly enhances outcomes. Remember that tirzepatide is approved only for adults; it is not indicated for pediatric patients.
Glycemic improvements typically occur within 4-8 weeks, with measurable hemoglobin A1c reductions, while weight loss becomes noticeable within the first month and may continue progressively for up to 72 weeks based on clinical trials.
Individual response varies due to genetic differences in receptor expression, baseline metabolic characteristics, pancreatic beta cell function, duration of diabetes, lifestyle factors, and adherence to dietary and physical activity recommendations.
Combine tirzepatide with nutrient-dense, high-protein meals, at least 150 minutes of weekly moderate-intensity exercise, consistent once-weekly injections on the same day, and regular follow-up appointments with your healthcare provider for monitoring and dose adjustments.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.