LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
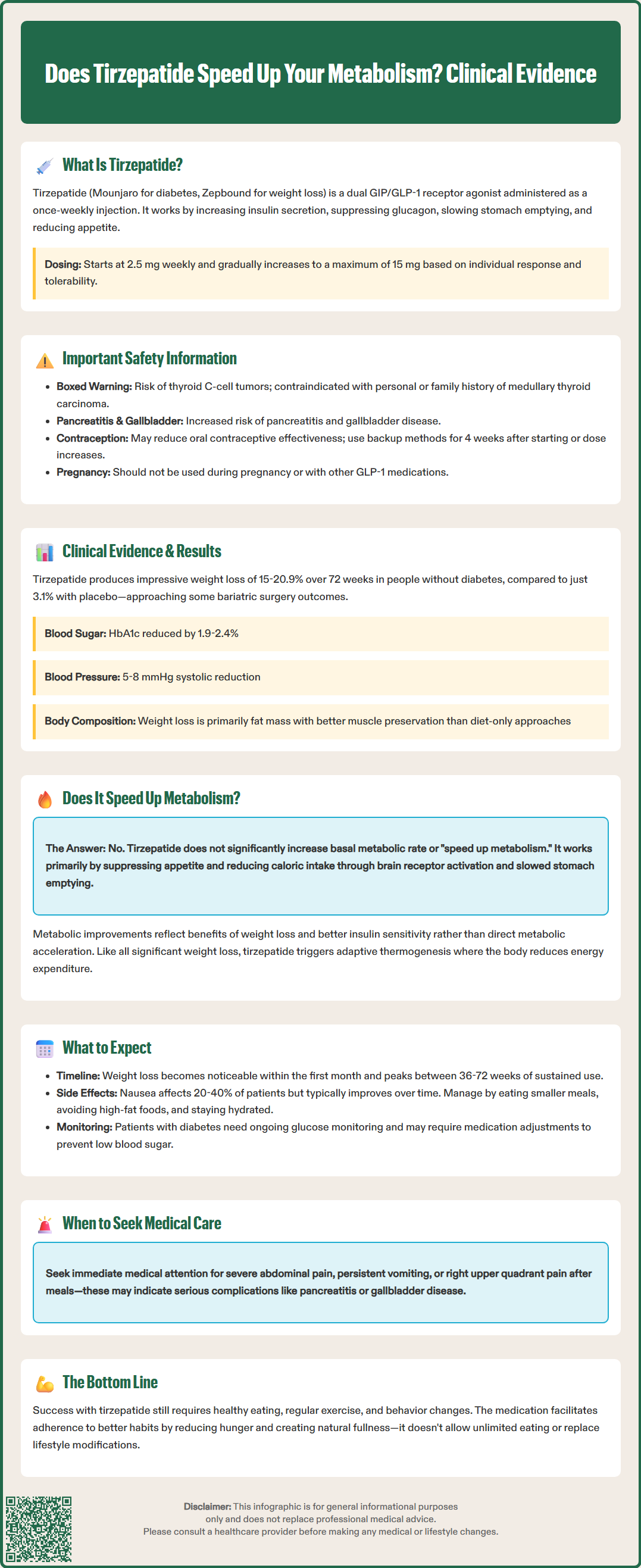
Does tirzepatide speed up your metabolism? This question arises frequently as patients and clinicians explore this dual GIP/GLP-1 receptor agonist for weight management and type 2 diabetes. Approved by the FDA as Mounjaro for diabetes and Zepbound for chronic weight management, tirzepatide produces significant weight loss and metabolic improvements. However, understanding precisely how these benefits occur—and whether they involve increased calorie burning—is essential for setting appropriate expectations. This article examines the clinical evidence on tirzepatide's metabolic effects, clarifying what patients can realistically expect from this medication.
Quick Answer: Tirzepatide does not substantially increase basal metabolic rate; instead, it produces weight loss primarily through appetite suppression and reduced caloric intake.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (brand name Mounjaro) and chronic weight management (brand name Zepbound). For weight management, Zepbound is indicated for adults with a BMI ≥30 kg/m², or ≥27 kg/m² with at least one weight-related comorbidity, as an adjunct to reduced-calorie diet and increased physical activity.
The medication works through multiple complementary mechanisms. By activating GLP-1 receptors, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. The additional GIP receptor activation appears to augment insulin secretion further, though the precise contribution of GIP agonism to clinical outcomes, including potential effects on fat metabolism and energy expenditure, remains an area of active investigation with limited human data.
Tirzepatide is administered as a once-weekly subcutaneous injection, with dosing typically initiated at 2.5 mg and gradually titrated upward based on glycemic control and tolerability. Maximum approved doses are 15 mg weekly for diabetes management and up to 15 mg weekly for weight management. The medication's extended half-life of approximately five days enables weekly dosing while maintaining therapeutic levels.
Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, which are generally mild to moderate and tend to diminish with continued use. Tirzepatide carries a Boxed Warning for thyroid C-cell tumors (based on rodent studies), making it contraindicated in patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. Other important safety considerations include risk of pancreatitis, gallbladder disease, hypoglycemia (especially when used with insulin or sulfonylureas), and delayed gastric emptying that may reduce oral contraceptive effectiveness (requiring backup contraception for 4 weeks after initiation and each dose escalation). Tirzepatide should not be used in type 1 diabetes, diabetic ketoacidosis, or severe gastrointestinal disease including gastroparesis. It should be discontinued if pregnancy occurs and is not recommended during pregnancy or breastfeeding. Tirzepatide should not be coadministered with other GLP-1 receptor agonists.
The SURPASS clinical trial program and the SURMOUNT weight management studies have provided extensive data on tirzepatide's metabolic effects. In the SURMOUNT-1 trial, participants without diabetes achieved weight reductions of 15% to 20.9% from baseline over 72 weeks, depending on dose, compared to 3.1% with placebo. These results exceeded those typically seen with lifestyle interventions alone and approached outcomes from some bariatric surgical procedures in certain analyses, though bariatric surgery generally produces greater average weight loss.
Beyond weight loss, tirzepatide demonstrates favorable effects on multiple cardiometabolic parameters. Clinical trials have documented improvements in glycemic control (HbA1c reductions of 1.9% to 2.4% in diabetes patients), blood pressure reductions (typically 5-8 mmHg systolic, placebo-adjusted), and lipid profile improvements including reductions in triglycerides and modest increases in HDL cholesterol. These changes reflect comprehensive metabolic benefits extending beyond simple caloric restriction.
Body composition analyses from clinical studies reveal that weight loss with tirzepatide consists predominantly of fat mass reduction, with relative preservation of lean body mass compared to the proportion typically lost with diet-induced weight loss alone. While the majority of weight lost is fat mass, some lean mass loss does occur, as expected with any significant weight reduction.
Metabolic rate measurements in clinical research have shown mixed findings. The primary driver of weight loss appears to be reduced caloric intake secondary to appetite suppression and delayed gastric emptying, rather than a substantial increase in basal metabolic rate. Improvements in insulin sensitivity and glucose metabolism likely contribute to the overall metabolic benefits but do not constitute a traditional "metabolism boost" in the sense of increased calorie burning at rest. As with any significant weight loss, adaptive thermogenesis (a decrease in resting energy expenditure) typically occurs, which may partially offset any metabolic changes.
Patients initiating tirzepatide should anticipate a gradual titration schedule designed to minimize gastrointestinal side effects while optimizing therapeutic response. Treatment typically begins at 2.5 mg weekly for four weeks, followed by increases of 2.5 mg every four weeks as tolerated. This stepwise approach allows physiological adaptation and helps identify the minimum effective dose for each individual.
Weight loss typically becomes noticeable within the first month of treatment, with progressive reductions continuing throughout the titration phase and beyond. Peak weight loss generally occurs between 36 and 72 weeks of treatment, though individual responses vary considerably. Patients should understand that tirzepatide is not a rapid weight-loss solution but rather a long-term intervention requiring sustained use and lifestyle modification for optimal results.
Gastrointestinal symptoms represent the most common treatment-emergent adverse effects, affecting approximately 20-40% of patients depending on dose. Nausea is typically most pronounced during dose escalation periods and often improves with continued treatment. Practical management strategies include eating smaller, more frequent meals, avoiding high-fat foods, staying well-hydrated, and timing doses consistently. Patients experiencing persistent or severe gastrointestinal symptoms should consult their healthcare provider, as dose adjustment or temporary dose reduction may be appropriate.
Monitoring during tirzepatide therapy should be individualized based on indication and comorbidities. Patients with diabetes require ongoing glucose monitoring, as tirzepatide may necessitate adjustments to other diabetes medications, particularly insulin or sulfonylureas, to prevent hypoglycemia. Those with diabetic retinopathy should be monitored for worsening of this condition. For patients using Zepbound, monitoring for depression or suicidal thoughts is recommended per FDA labeling. Women of childbearing potential should use nonoral contraception or add a backup method for 4 weeks after initiation and each dose escalation due to potential reduced effectiveness of oral contraceptives. Tirzepatide should be discontinued if pregnancy occurs.
Immediate medical attention is warranted for severe abdominal pain (possible pancreatitis), persistent vomiting with inability to tolerate oral intake (risk of dehydration and acute kidney injury), or symptoms of gallbladder disease such as right upper quadrant pain, particularly after meals. Patients should inform surgical teams about tirzepatide use due to its effects on gastric emptying. Healthcare providers should also counsel patients about the importance of adequate protein intake and resistance exercise to help preserve lean muscle mass during weight loss.
The straightforward answer is that tirzepatide does not substantially increase basal metabolic rate in the traditional sense of "speeding up metabolism." While the medication produces significant effects on weight and metabolic health, these benefits arise primarily through mechanisms other than increased calorie burning at rest. This distinction is important for setting appropriate patient expectations and understanding how tirzepatide differs from stimulant-based weight loss approaches.
Tirzepatide's primary mechanism for weight reduction is appetite suppression and reduced caloric intake. By activating GLP-1 receptors in appetite-regulating brain regions and slowing gastric emptying, the medication creates earlier satiety and prolonged fullness after meals. Clinical trial participants typically report decreased hunger, reduced food cravings, and smaller portion sizes—all contributing to a sustained caloric deficit without the conscious effort and hunger typically associated with caloric restriction.
Some metabolic improvements do occur with tirzepatide treatment, but these largely reflect the beneficial consequences of weight loss and improved insulin sensitivity rather than direct metabolic acceleration. As patients lose weight and reduce visceral adiposity, insulin resistance improves, allowing more efficient glucose utilization and reduced hepatic glucose production. Enhanced insulin sensitivity may improve substrate metabolism, but this represents normalization of previously impaired metabolic function rather than supraphysiologic metabolic enhancement.
While preclinical studies have suggested potential mechanisms by which GIP receptor activation might influence adipose tissue metabolism or mitochondrial function, human data have not demonstrated a meaningful increase in basal metabolic rate with tirzepatide. Furthermore, as with any significant weight loss, adaptive thermogenesis (metabolic adaptation) occurs, whereby the body reduces energy expenditure in response to weight reduction, which would likely counteract any minor metabolic effects.
For patients considering tirzepatide, realistic expectations are crucial. The medication offers support for weight management through appetite regulation and metabolic improvements, but it does not override the fundamental principles of energy balance. Successful outcomes still require attention to dietary quality, regular physical activity, and behavioral modifications. Patients should not expect to "eat whatever they want" and lose weight simply because their metabolism has been altered. Rather, tirzepatide facilitates adherence to healthier eating patterns by reducing hunger and food preoccupation, making sustainable lifestyle changes more achievable for many individuals who have struggled with conventional weight loss approaches.
Tirzepatide causes weight loss primarily by suppressing appetite and slowing gastric emptying, which leads to reduced caloric intake. Patients typically experience decreased hunger, earlier satiety, and smaller portion sizes, creating a sustained caloric deficit without the intense hunger associated with traditional dieting.
Tirzepatide improves insulin sensitivity, glycemic control, blood pressure, and lipid profiles as beneficial consequences of weight loss and reduced visceral fat. These represent normalization of previously impaired metabolic function rather than supraphysiologic metabolic enhancement.
Tirzepatide is contraindicated in patients with personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. It should not be used in type 1 diabetes, diabetic ketoacidosis, severe gastrointestinal disease, or during pregnancy.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.