LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Hitting a plateau on tirzepatide is a common experience during weight loss treatment, typically defined as minimal weight change over four consecutive weeks despite continued medication use and lifestyle adherence. This temporary stall doesn't mean the medication has stopped working—it reflects normal metabolic adaptation as your body adjusts to a lower weight. Understanding why plateaus occur and how to address them through dose optimization, dietary adjustments, and activity modifications can help you resume progress toward your weight goals. This guide explains the science behind tirzepatide plateaus and provides evidence-based strategies to overcome them.
Quick Answer: A weight loss plateau on tirzepatide—defined as less than 1% body weight change over four weeks—is a normal physiological response to metabolic adaptation and can often be addressed through dose escalation, dietary reassessment, or increased physical activity.
A weight loss plateau on tirzepatide refers to a period of several weeks during which body weight remains stable despite continued medication use and adherence to lifestyle modifications. As a practical clinical rule of thumb, this is often described as minimal or no weight change—typically less than 1% of body weight—over a consecutive four-week period. Plateaus are a normal physiological response during extended weight loss treatment and do not necessarily indicate treatment failure or medication resistance.
Tirzepatide (Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. Clinical trials demonstrate that most patients experience substantial weight reduction, with the rate of loss typically slowing as treatment continues. The SURMOUNT-1 trial showed that while average weight loss at 72 weeks reached 15–21% depending on dose, the trajectory was not linear, with many participants experiencing temporary plateaus.
It is important to distinguish a true plateau from expected treatment response patterns. During the initial months of tirzepatide therapy, rapid weight loss occurs as the medication reduces appetite, slows gastric emptying (an effect that may attenuate somewhat over time), and improves insulin sensitivity. As the body adapts to a lower weight, metabolic rate adjusts downward—a protective mechanism that can slow further weight reduction. Understanding this physiological adaptation helps patients maintain realistic expectations and avoid premature discontinuation of effective therapy. A plateau does not mean the medication has stopped working; rather, it may signal that dose optimization, lifestyle adjustments, or patience is needed to resume progress toward weight goals.
Weight loss plateaus during tirzepatide treatment result from multiple interconnected physiological and behavioral factors. The primary mechanism involves metabolic adaptation, a well-documented phenomenon in which the body reduces energy expenditure in response to sustained caloric deficit and weight loss. As body mass decreases, basal metabolic rate naturally declines because less energy is required to maintain a smaller body. Additionally, adaptive thermogenesis—a compensatory reduction in energy expenditure beyond what would be predicted by weight loss alone—can further slow metabolic rate, often by approximately 100-300 kcal/day, making continued weight reduction progressively more difficult.
Hormonal changes also contribute significantly to plateau development. Weight loss triggers increases in ghrelin (the hunger hormone) and decreases in leptin (the satiety hormone), creating a biological drive to regain lost weight. While tirzepatide's dual GIP/GLP-1 agonism helps counteract some of these hormonal shifts by enhancing satiety signals and reducing appetite, the body's homeostatic mechanisms remain active. Furthermore, as patients lose weight, the absolute caloric deficit created by the same dietary intake diminishes—what constituted a 500-calorie daily deficit at a higher weight may only represent a 300-calorie deficit after significant weight loss.
Behavioral factors frequently play an underappreciated role in plateau development. Dietary adherence often relaxes over time as initial motivation wanes or as patients unconsciously increase portion sizes. Physical activity levels may decrease due to fatigue, injury, or simple routine disruption. Additionally, some patients may reach a dose that was initially effective but becomes insufficient as treatment progresses. The FDA-approved dosing schedule for tirzepatide allows for escalation from 2.5 mg to a maximum of 15 mg weekly, with increases of 2.5 mg at minimum four-week intervals based on clinical response and tolerability.
Certain medications can also impede weight loss, including some antipsychotics, antidepressants, steroids, insulin, and sulfonylureas. Underlying medical conditions such as hypothyroidism, Cushing's syndrome, or polycystic ovary syndrome may contribute to weight loss resistance. Fluid retention and changes in body composition can mask continued fat loss on the scale. As patients increase physical activity or resistance training, they may gain lean muscle mass while simultaneously losing fat tissue, resulting in stable weight despite favorable body composition changes. Hormonal fluctuations, sodium intake variations, and medication effects can cause temporary water retention that obscures ongoing fat reduction. These factors underscore the importance of using multiple metrics—including waist circumference, body composition analysis, and clinical markers like hemoglobin A1c and blood pressure—rather than relying solely on scale weight to assess treatment response.
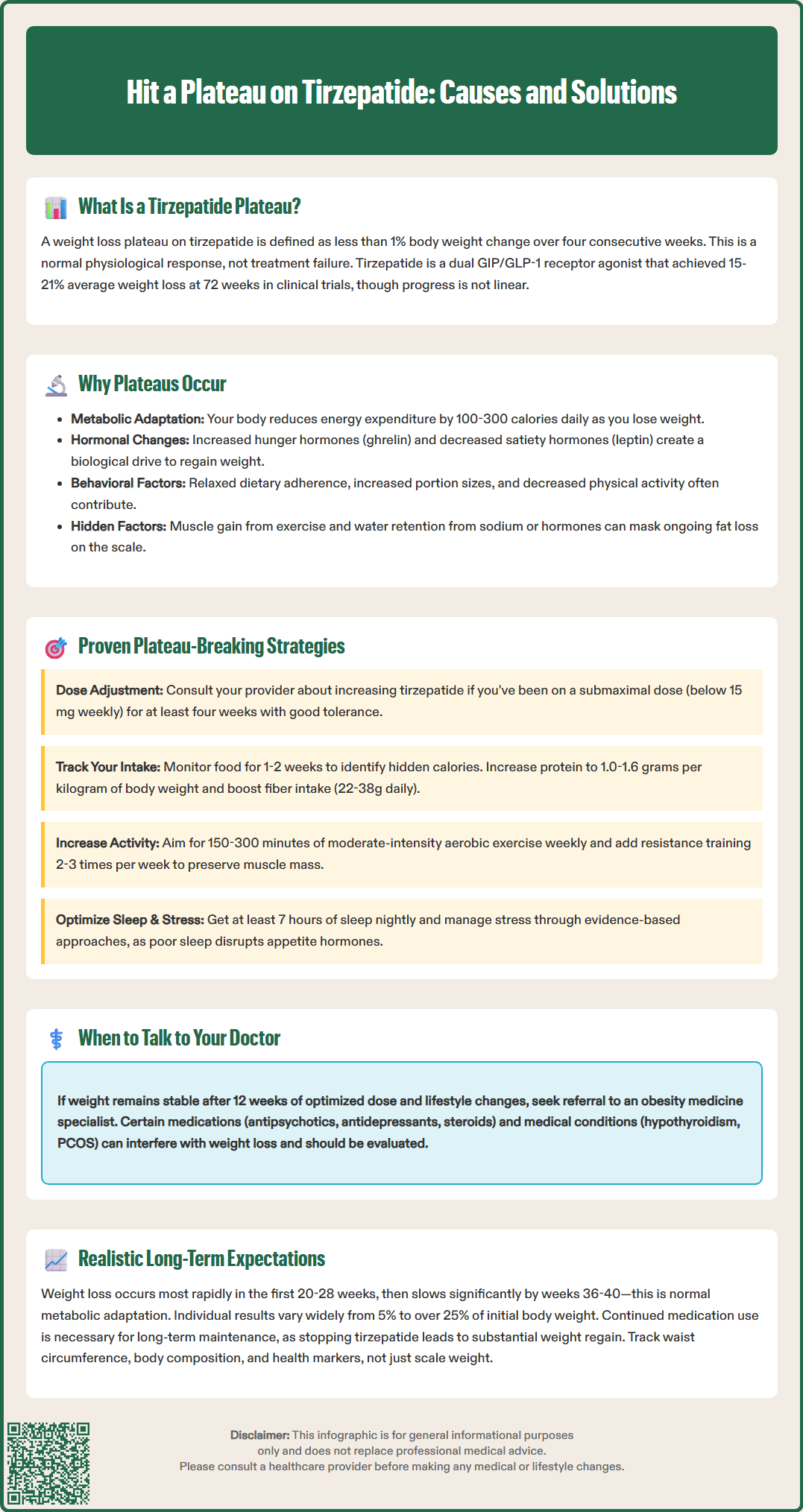
Breaking through a tirzepatide plateau requires a systematic, evidence-based approach that addresses both medication optimization and lifestyle factors. The first step involves consultation with the prescribing healthcare provider to assess whether dose escalation is appropriate. If a patient has been stable on a submaximal dose (below 15 mg weekly) for at least four weeks and has tolerated the current dose well, increasing to the next dose level may restore weight loss momentum. Dose titration should follow FDA-approved guidelines, with increases of 2.5 mg occurring at minimum four-week intervals to minimize gastrointestinal adverse effects such as nausea, vomiting, and diarrhea.
Dietary reassessment is essential when addressing a plateau. Patients should work with a registered dietitian to conduct a thorough review of current eating patterns, as caloric intake often increases gradually without conscious awareness. Strategies that may prove effective include:
Dietary modifications:
Tracking food intake for one to two weeks to identify hidden calories or portion creep
Increasing protein intake to 1.0–1.6 grams per kilogram of body weight to preserve lean muscle mass and enhance satiety (with appropriate adjustments for patients with kidney disease)
Reducing ultra-processed foods and increasing whole food consumption
Implementing structured meal timing to prevent grazing behavior
Ensuring adequate fiber intake (women ~22–28g, men ~30–38g daily, per USDA Dietary Guidelines) to support satiety and metabolic health
Physical activity modification represents another critical intervention point. The Physical Activity Guidelines for Americans recommends 150–300 minutes of moderate-intensity aerobic activity weekly for general health, with higher volumes often needed for weight loss and maintenance. Incorporating resistance training two to three times weekly helps preserve lean muscle mass during weight reduction and can increase resting metabolic rate. Patients who have maintained the same exercise routine throughout treatment may benefit from periodization—systematically varying exercise intensity, duration, or type to prevent physiological adaptation.
Addressing behavioral and psychological factors is equally important. Cognitive-behavioral strategies can help patients identify and modify patterns that contribute to plateau, such as emotional eating, stress-related food choices, or decreased treatment adherence. Sleep optimization is often overlooked but critical—inadequate sleep (less than seven hours nightly) disrupts appetite-regulating hormones and increases cravings for high-calorie foods. Stress management through mindfulness practices, counseling, or other evidence-based approaches can reduce cortisol-driven weight retention and improve overall treatment adherence.
Patients should be counseled that breaking through a plateau typically requires four to eight weeks of consistent intervention. Weekly weigh-ins under standardized conditions (same time of day, same scale, similar clothing) provide sufficient data for most patients, though some may benefit from daily weighing if it doesn't cause undue anxiety. If weight remains stable despite dose optimization and comprehensive lifestyle modifications for 12 weeks or more, referral to an obesity medicine specialist or endocrinologist may be warranted to evaluate for underlying metabolic conditions, medication interactions, or the need for additional treatment approaches. Note that combining tirzepatide with other anti-obesity medications is considered off-label with limited evidence, and tirzepatide should not be used with other GLP-1 receptor agonists.
Establishing realistic expectations for long-term tirzepatide treatment is essential for patient satisfaction and sustained adherence. Clinical trial data from the SURMOUNT program provide the most robust evidence for expected outcomes. In SURMOUNT-1, which enrolled adults with obesity or overweight without diabetes, participants receiving tirzepatide 5 mg, 10 mg, or 15 mg weekly achieved mean weight reductions of 15.0%, 19.5%, and 20.9% respectively at 72 weeks, compared to 3.1% with placebo. However, these averages mask substantial individual variation—while some patients lost more than 25% of their initial body weight, others experienced more modest reductions of 5–10%.
Weight loss trajectory typically follows a predictable pattern during tirzepatide therapy. The most rapid reduction occurs during the first 20–28 weeks of treatment, with the rate of loss gradually slowing thereafter. By week 36–40, many patients reach a weight nadir or experience significantly slower ongoing reduction. This deceleration is physiologically normal and reflects metabolic adaptation rather than treatment failure. Patients should understand that achieving 10–15% total body weight loss represents a clinically significant outcome associated with meaningful improvements in cardiovascular risk factors, glycemic control, sleep apnea severity, and joint pain.
Long-term weight maintenance on tirzepatide requires continued medication use in most patients. The SURMOUNT-4 trial demonstrated that participants who discontinued tirzepatide after achieving weight loss regained a substantial portion of their lost weight over the subsequent 52 weeks, while those who continued treatment maintained their weight reduction. This finding underscores that obesity is a chronic disease requiring ongoing management rather than a condition that can be permanently "cured" with temporary intervention. Patients should be counseled that tirzepatide is likely a long-term or indefinite therapy, similar to medications for hypertension or diabetes.
Key expectations for long-term treatment include:
Weight loss velocity decreases over time, with most reduction occurring in the first 9–12 months
Plateaus lasting 4–8 weeks are common and do not indicate treatment failure
Individual response varies based on genetics, baseline metabolic health, adherence, and lifestyle factors
Continued medication use is typically necessary to maintain weight loss
Non-scale victories—improved mobility, reduced medication burden for comorbidities, better quality of life—are equally important outcomes
Patients should also be aware of potential adverse effects that may affect long-term adherence. Gastrointestinal symptoms (nausea, diarrhea, constipation, abdominal pain) are most common, typically occurring during dose escalation and often improving with continued use. More serious but rare adverse effects include pancreatitis, gallbladder disease, and potential thyroid C-cell tumors (based on rodent studies; human relevance uncertain). The FDA label includes a boxed warning regarding thyroid C-cell tumors and contraindicates tirzepatide in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
Important safety considerations include: tirzepatide is not recommended during pregnancy or breastfeeding; it may reduce the effectiveness of oral contraceptives during initiation/dose escalation; it can increase hypoglycemia risk when used with insulin or sulfonylureas; severe gastrointestinal adverse events may lead to dehydration and acute kidney injury; and caution is needed in patients with severe gastrointestinal disease. Tirzepatide should not be used in combination with other GLP-1 receptor agonists.
Regular monitoring is essential for safe long-term use. Patients should have follow-up appointments every 4–12 weeks during dose titration and every 3–6 months once on a stable dose. Monitoring should include assessment of weight, blood pressure, heart rate, and symptoms of adverse effects. For patients with diabetes, hemoglobin A1c should be checked every 3–6 months. Individualized laboratory monitoring may include renal function, lipid profiles, and thyroid testing when clinically appropriate. Patients should promptly report severe or persistent abdominal pain (possible pancreatitis), persistent vomiting/diarrhea (dehydration risk), jaundice or right upper quadrant pain (gallbladder disease), neck masses/voice changes/difficulty swallowing (thyroid concerns), or visual changes (diabetic retinopathy concerns in patients with diabetes). With appropriate patient selection, realistic goal-setting, and comprehensive monitoring, tirzepatide represents an effective long-term tool for chronic weight management as part of a multifaceted treatment approach.
A typical plateau lasts 4–8 weeks and is considered normal during tirzepatide treatment. If weight remains stable despite dose optimization and lifestyle modifications for 12 weeks or more, consultation with your healthcare provider or referral to an obesity medicine specialist may be warranted.
Dose escalation may be appropriate if you've been on a submaximal dose (below 15 mg weekly) for at least four weeks and have tolerated it well. Your healthcare provider can determine if increasing by 2.5 mg is suitable based on your clinical response and tolerability.
Combining tirzepatide with other anti-obesity medications is considered off-label with limited evidence, and it should not be used with other GLP-1 receptor agonists. Discuss any combination therapy considerations with your healthcare provider to evaluate safety and appropriateness for your situation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.