LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Weight loss plateaus on tirzepatide are a common concern for patients and clinicians managing obesity and type 2 diabetes. Tirzepatide, a dual GIP and GLP-1 receptor agonist marketed as Mounjaro and Zepbound, demonstrates substantial weight reduction in clinical trials, yet most patients experience periods where weight loss slows or temporarily stalls. Understanding whether plateaus occur, why they happen, and how to manage them is essential for optimizing long-term outcomes. This article examines the science behind weight loss plateaus during tirzepatide therapy, explores physiological mechanisms that contribute to slowed progress, and provides evidence-based strategies for maintaining therapeutic benefits throughout extended treatment.
Quick Answer: Yes, most patients experience weight loss plateaus on tirzepatide, typically after the first several months of treatment, though the medication continues to provide metabolic benefits throughout extended therapy.
Weight loss plateaus are a common phenomenon during pharmacotherapy with tirzepatide, and understanding this pattern is essential for both clinicians and patients. A plateau refers to a period where weight loss slows significantly or stops temporarily despite continued medication adherence and lifestyle efforts.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist with two FDA-approved formulations: Mounjaro for type 2 diabetes management and Zepbound for chronic weight management. Clinical trials demonstrate substantial weight reduction, with participants losing an average of 15-21% of body weight over 72 weeks in the SURMOUNT-1 trial. However, these trials also reveal that weight loss velocity typically decreases over time, with more rapid reduction generally occurring in the earlier months of treatment.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
Plateaus should be distinguished from treatment failure. While initial weight loss may be substantial for many patients in early months, a plateau does not necessarily indicate medication ineffectiveness. Rather, it reflects complex physiological adaptations as the body approaches a new metabolic equilibrium. Research indicates that most patients on tirzepatide experience some degree of weight loss deceleration, particularly after the first several months of therapy.
Understanding that plateaus are a normal part of the weight loss trajectory helps set realistic expectations and prevents premature discontinuation of effective therapy. The key clinical question is not whether plateaus occur, but how to recognize, manage, and potentially overcome them while maintaining the metabolic benefits tirzepatide provides.
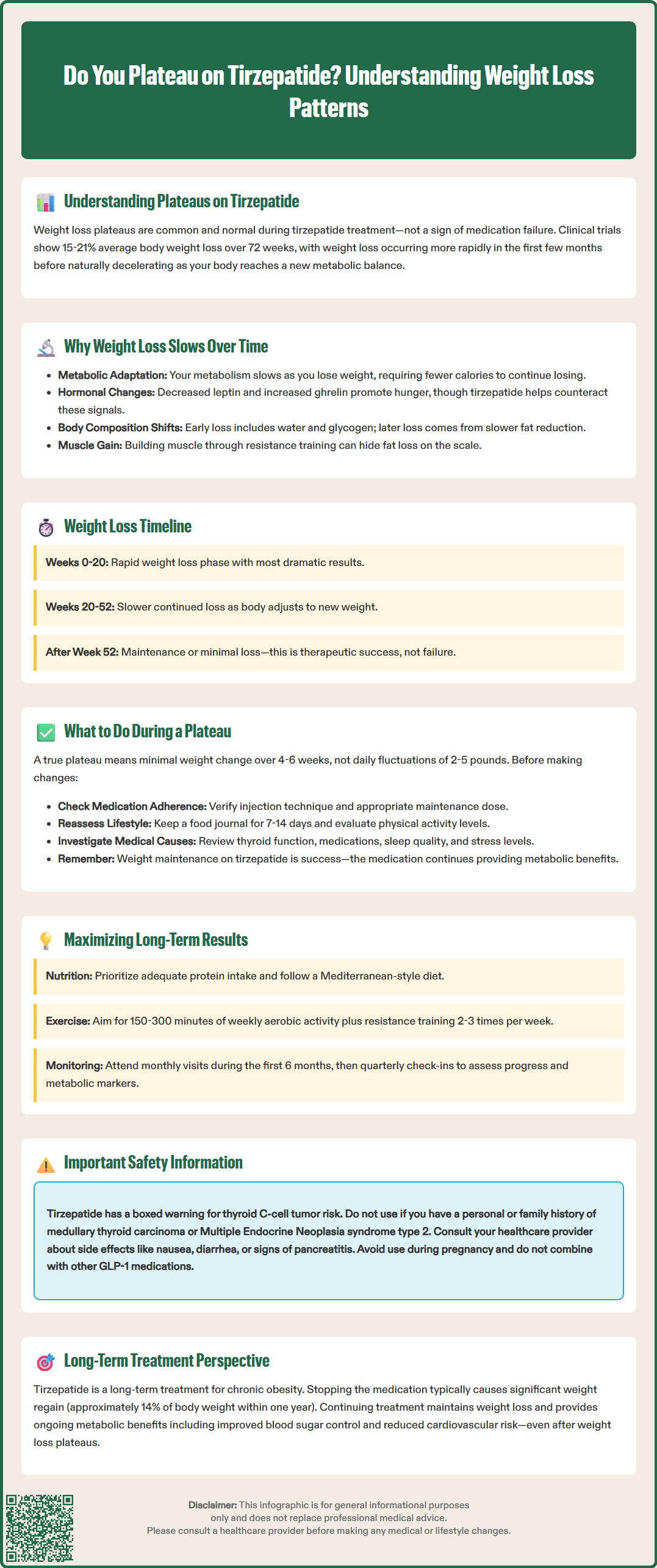
Multiple physiological mechanisms contribute to weight loss plateaus during tirzepatide therapy, reflecting the body's sophisticated homeostatic responses to caloric restriction and weight reduction.
Metabolic Adaptation and Adaptive Thermogenesis
As body weight decreases, basal metabolic rate (BMR) declines proportionally—and sometimes disproportionally—to the loss of metabolic tissue. This phenomenon, termed adaptive thermogenesis or metabolic adaptation, means the body requires fewer calories to maintain its new lower weight. Research suggests that metabolic rate may decrease beyond what would be predicted by tissue loss alone, creating a moving target where the caloric deficit that initially produced weight loss becomes insufficient over time.
Hormonal Counter-Regulation
Weight loss triggers compensatory hormonal changes that promote weight regain. Leptin levels decrease with fat mass reduction, signaling energy deficiency to the hypothalamus. Simultaneously, ghrelin (the hunger hormone) often increases. Although tirzepatide's GLP-1 and GIP agonism helps counteract some hunger signals, these counter-regulatory mechanisms can still exert influence, particularly as treatment duration extends.
Body Composition Changes
Initial weight loss often includes significant water weight and glycogen depletion, which occurs rapidly. As treatment continues, weight loss shifts primarily to fat mass reduction, which occurs more slowly. Additionally, patients who incorporate resistance training may experience relative preservation of lean muscle mass, which can mask fat loss on the scale while representing favorable body composition changes.
Medication Response and Receptor Dynamics
While true pharmacological tolerance to GLP-1 receptor agonists appears limited based on current evidence, individual variation in receptor expression, desensitization patterns, and downstream signaling may influence long-term response. There is no definitive evidence that tirzepatide loses effectiveness due to receptor downregulation, but individual pharmacodynamic responses vary.
Clinical trial data provide reassuring evidence that tirzepatide maintains therapeutic efficacy throughout extended treatment periods, though the pattern of weight loss evolves over time.
The landmark SURMOUNT-1 trial followed participants for 72 weeks (approximately 18 months), demonstrating continued weight reduction throughout the study period. Participants receiving the maximum 15 mg dose achieved mean weight loss of 20.9% by week 72, with weight loss curves showing continued downward trajectory, albeit at a slower rate in later months. Importantly, weight stabilization rather than regain was observed in most participants who reached their nadir weight, suggesting sustained pharmacological effect.
The temporal pattern typically follows a predictable course:
Weeks 0-20: Rapid weight loss phase, with the steepest decline in body weight. Many patients experience their most significant weekly losses during dose escalation, though individual results vary considerably.
Weeks 20-52: Continued but decelerating weight loss. The rate typically slows as patients approach substantial total body weight reduction.
Weeks 52-72 and beyond: Weight maintenance or slow continued loss. Many patients reach a plateau where weight stabilizes, representing a new equilibrium between medication effects, metabolic adaptation, and lifestyle factors.
The SURMOUNT-4 trial demonstrated that participants who discontinued tirzepatide after initial weight loss regained significant weight (approximately 14% regain over 52 weeks following randomized withdrawal), while those continuing treatment maintained their weight loss, confirming ongoing medication efficacy.
Glycemic control benefits in patients with type 2 diabetes similarly persist throughout extended treatment, with sustained HbA1c reductions maintained at 18-24 months in the SURPASS clinical trials. This suggests that the medication's metabolic effects remain active even when weight loss plateaus, providing continued cardiometabolic benefit beyond weight reduction alone.
Encountering a weight loss plateau on tirzepatide warrants systematic evaluation and evidence-based management strategies rather than immediate treatment discontinuation or dramatic intervention.
Clinical Assessment and Monitoring
First, confirm that a true plateau exists. Weight fluctuates naturally by 2-5 pounds daily due to hydration, sodium intake, and bowel patterns. A plateau generally refers to minimal weight change over 4-6 weeks at a stable dose with confirmed adherence. Document weight trends over time rather than reacting to single measurements.
Review medication adherence carefully. Missed doses, improper injection technique, or inadequate dose escalation may contribute to suboptimal response. Verify that patients have reached an appropriate maintenance dose (5, 10, or 15 mg weekly, as tolerated) per FDA labeling.
Safety Monitoring
Patients should be advised to seek immediate medical attention for severe abdominal pain (potential pancreatitis), signs of gallbladder disease, uncontrollable vomiting, or dehydration. Patients with type 2 diabetes using insulin or sulfonylureas should monitor blood glucose closely, as medication adjustments may be needed to prevent hypoglycemia.
Lifestyle Modification Reassessment
Even with effective pharmacotherapy, lifestyle factors remain crucial. Conduct a thorough dietary review, as caloric intake often increases unconsciously as appetite suppression diminishes or patients become less vigilant. Food journaling for 7-14 days can reveal hidden caloric sources. Consider referral to a registered dietitian nutritionist (RDN) for medical nutrition therapy.
Physical activity assessment is equally important. Evaluate both structured exercise and non-exercise activity thermogenesis (NEAT). Resistance training becomes particularly valuable during plateaus, as it helps preserve lean muscle mass and improves body composition even when scale weight stabilizes.
Medical Evaluation
Investigate potential medical contributors to weight loss resistance:
Thyroid function: Check TSH if not recently assessed, as hypothyroidism impairs weight loss
Medications: Review for weight-promoting drugs (antipsychotics, certain antidepressants, corticosteroids)
Sleep disorders: Screen for sleep apnea and insufficient sleep, both associated with weight loss resistance
Stress and cortisol: Chronic stress elevates cortisol, promoting central adiposity and metabolic dysfunction
Dose Optimization
If patients have not reached the maximum tolerated dose, consider further titration according to FDA labeling. The 15 mg dose demonstrated superior weight loss compared to lower doses in clinical trials. However, balance efficacy against gastrointestinal tolerability, as adverse effects may compromise adherence.
Setting Realistic Expectations
Counsel patients that plateaus are normal and that weight maintenance represents therapeutic success, not failure. Even without further weight loss, tirzepatide provides ongoing metabolic benefits including improved glycemic control, reduced cardiovascular risk markers, and decreased hepatic steatosis. Shifting focus from scale weight to overall health improvements and body composition changes can maintain motivation during plateau periods.
Achieving and maintaining optimal outcomes with tirzepatide requires a comprehensive, long-term approach that extends beyond pharmacotherapy alone.
Integrated Lifestyle Medicine
Tirzepatide is most effective when combined with evidence-based lifestyle interventions. The medication facilitates behavioral change by reducing hunger and food preoccupation, creating a therapeutic window for establishing sustainable habits. Key components include:
Nutrition strategies: Emphasize adequate protein intake to preserve lean muscle mass during weight loss, with targets individualized based on patient factors including renal function. Focus on nutrient-dense, minimally processed foods with high satiety value. The Mediterranean dietary pattern has strong evidence for cardiovascular health and weight maintenance, aligning with the Dietary Guidelines for Americans 2020-2025.
Physical activity: Current U.S. Physical Activity Guidelines recommend 150-300 minutes of moderate-intensity aerobic activity weekly, plus resistance training 2-3 times weekly. Resistance training is particularly important during weight loss to help preserve metabolic rate and functional capacity.
Behavioral support: Cognitive-behavioral strategies, mindful eating practices, and stress management techniques enhance long-term success. Consider referral to behavioral health specialists for patients with emotional eating patterns or binge eating disorder.
Safety Considerations
Tirzepatide should not be used concurrently with other GLP-1 receptor agonists. Patients should be reminded of the boxed warning regarding thyroid C-cell tumors and contraindication in patients with personal/family history of MTC or MEN2.
Monitor for signs of pancreatitis, gallbladder disease, and in patients with diabetes, potential retinopathy progression with rapid glycemic improvement. Advise patients to use effective contraception during treatment, as weight loss medications are generally not recommended during pregnancy.
Patients should be cautioned against using compounded tirzepatide products, as the FDA has issued safety warnings about these non-FDA-approved formulations.
Monitoring and Follow-Up
Establish a structured monitoring schedule:
Monthly visits during dose titration and the first 6 months
Quarterly visits once stable, assessing weight, tolerability, and metabolic parameters
Annual comprehensive evaluation including lipid panel, HbA1c (if diabetic), liver function tests, and cardiovascular risk assessment
Regular monitoring allows early identification of plateaus, adverse effects, or emerging medical issues that may require intervention.
Managing Expectations and Treatment Duration
Current evidence supports continued tirzepatide for weight maintenance, as discontinuation typically results in weight regain. The SURMOUNT-4 trial demonstrated that patients who stopped tirzepatide after achieving weight loss regained approximately 14% of body weight over 52 weeks, while those continuing treatment maintained their loss.
Counsel patients that tirzepatide treats obesity as a chronic disease requiring ongoing management, similar to medications for hypertension or diabetes. This framework helps patients understand that long-term treatment is expected rather than representing treatment failure.
Addressing Tolerability Issues
Gastrointestinal adverse effects (nausea, vomiting, diarrhea, constipation) are the most common reasons for discontinuation. Management strategies include:
Slower dose titration if standard escalation causes intolerable symptoms
Dietary modifications: smaller, more frequent meals; avoiding high-fat foods; adequate hydration
Symptomatic treatment: antiemetics for nausea, fiber supplementation or laxatives for constipation
Temporary dose reduction if needed, with re-escalation attempt after symptom resolution
Cost and Access Considerations
Insurance coverage for weight management indications varies significantly. For patients facing access barriers, discuss:
Manufacturer savings programs and patient assistance programs
Alternative FDA-approved medications if tirzepatide is not covered
Prioritization for patients with obesity-related comorbidities where medical necessity is clearer
Combination and Sequential Therapies
For patients with inadequate response to tirzepatide monotherapy, combination approaches should be considered only under specialist oversight, as most combinations are off-label and safety data remain limited. Referral to obesity medicine specialists or endocrinologists is recommended for complex cases requiring advanced therapeutic strategies.
Ultimately, maximizing long-term results requires viewing tirzepatide as one component of comprehensive obesity management, integrated with lifestyle medicine, behavioral support, and ongoing clinical monitoring to achieve sustained metabolic health improvements.
Clinical trials demonstrate that tirzepatide maintains therapeutic efficacy through at least 72 weeks of treatment, with continued weight reduction or maintenance throughout this period. The SURMOUNT-4 trial confirmed ongoing medication effectiveness, as patients who discontinued tirzepatide regained significant weight while those continuing treatment maintained their weight loss.
Weight loss plateaus result from metabolic adaptation (decreased basal metabolic rate), hormonal counter-regulation (reduced leptin and increased ghrelin), and shifts in body composition from rapid initial water loss to slower fat mass reduction. These physiological responses represent normal homeostatic mechanisms rather than medication failure.
Dose optimization may be appropriate if you have not reached the maximum tolerated dose according to FDA labeling (up to 15 mg weekly). However, this decision should be made with your healthcare provider after confirming medication adherence, reassessing lifestyle factors, and evaluating for medical contributors to weight loss resistance.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.