LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Metformin, the first-line medication for type 2 diabetes, is routinely held before surgery to prevent a rare but serious complication called lactic acidosis. Surgical stress, anesthesia, dehydration, and contrast dye can temporarily impair kidney function, potentially causing metformin to accumulate in the bloodstream. While the absolute risk remains low in patients with normal renal function, the severity of metformin-associated lactic acidosis has led to widespread perioperative discontinuation protocols. Understanding when to stop and restart metformin ensures safe surgical outcomes while maintaining glycemic control.
Quick Answer: Metformin is typically held on the morning of surgery to prevent rare but serious lactic acidosis caused by reduced kidney function during surgical stress.
Metformin, a first-line oral medication for type 2 diabetes, is commonly held before surgery due to concerns about a rare but serious complication called lactic acidosis. This biguanide medication works by decreasing hepatic glucose production, modestly reducing intestinal glucose absorption, and improving insulin sensitivity in peripheral tissues. Under normal circumstances, metformin is eliminated unchanged by the kidneys and carries a very low risk of lactic acidosis in patients with normal renal function.
The concern during surgery arises from several physiological stressors that can temporarily impair kidney function. Surgical procedures often involve periods of reduced blood flow to organs, dehydration from fasting requirements, administration of contrast dye for imaging studies, and hemodynamic instability from anesthesia or blood loss. These factors can acutely reduce glomerular filtration rate, potentially leading to metformin accumulation in the bloodstream.
When metformin levels rise in the setting of compromised renal function, the drug can interfere with cellular metabolism, particularly through inhibition of mitochondrial complex I in the liver and muscles. This disruption can lead to increased lactate production and decreased lactate clearance, creating conditions favorable for lactic acidosis. Although the absolute risk remains low in most surgical patients, the potentially serious nature of metformin-associated lactic acidosis has led to widespread adoption of perioperative metformin discontinuation protocols.
The decision to hold metformin is particularly important for procedures involving iodinated contrast media, major surgery with significant fluid shifts, or operations in patients with baseline renal impairment or other risk factors for acute kidney injury. Current guidelines from the American Diabetes Association and surgical societies recommend individualized assessment of each patient's risk profile when determining the need for metformin discontinuation.
The timing of metformin discontinuation before surgery depends on the type of procedure, the patient's baseline kidney function, and institutional protocols. For most elective surgeries, current evidence supports holding metformin on the morning of the procedure, particularly in patients with normal renal function. This approach minimizes the duration of suboptimal glycemic control while still providing adequate drug clearance.
For minor outpatient procedures performed under local anesthesia with minimal physiological stress and no contrast exposure, some clinicians may not discontinue metformin, though this should be determined on a case-by-case basis. For procedures requiring general or regional anesthesia, metformin is typically held on the day of surgery. The patient should take their usual evening dose the night before but skip the morning dose on the day of the procedure.
More conservative approaches are warranted for certain high-risk scenarios. For procedures involving iodinated contrast media, FDA labeling recommends stopping metformin at or before the procedure in patients with an eGFR of 30-60 mL/min/1.73m², hepatic impairment, alcoholism, heart failure, or those receiving intra-arterial contrast. The American College of Radiology (ACR) 2024 guidance indicates no need to discontinue metformin for intravenous contrast if eGFR is ≥30 mL/min/1.73m² and there is no acute kidney injury, but recommends holding for eGFR <30, acute kidney injury, or certain intra-arterial first-pass studies. Patients should follow their institution's specific policy.
Patients with pre-existing chronic kidney disease require special consideration. Metformin is contraindicated in patients with an eGFR <30 mL/min/1.73m² and should be used with caution in those with an eGFR of 30-45 mL/min/1.73m². For patients in these higher-risk categories undergoing procedures with anticipated hemodynamic instability or high risk of acute kidney injury, earlier discontinuation may be appropriate based on individualized assessment.
Healthcare providers should provide clear written instructions specifying exactly when to take the last dose of metformin and document this in the preoperative assessment. Patients should also be advised to bring their medication list to all preoperative appointments to ensure coordinated care.
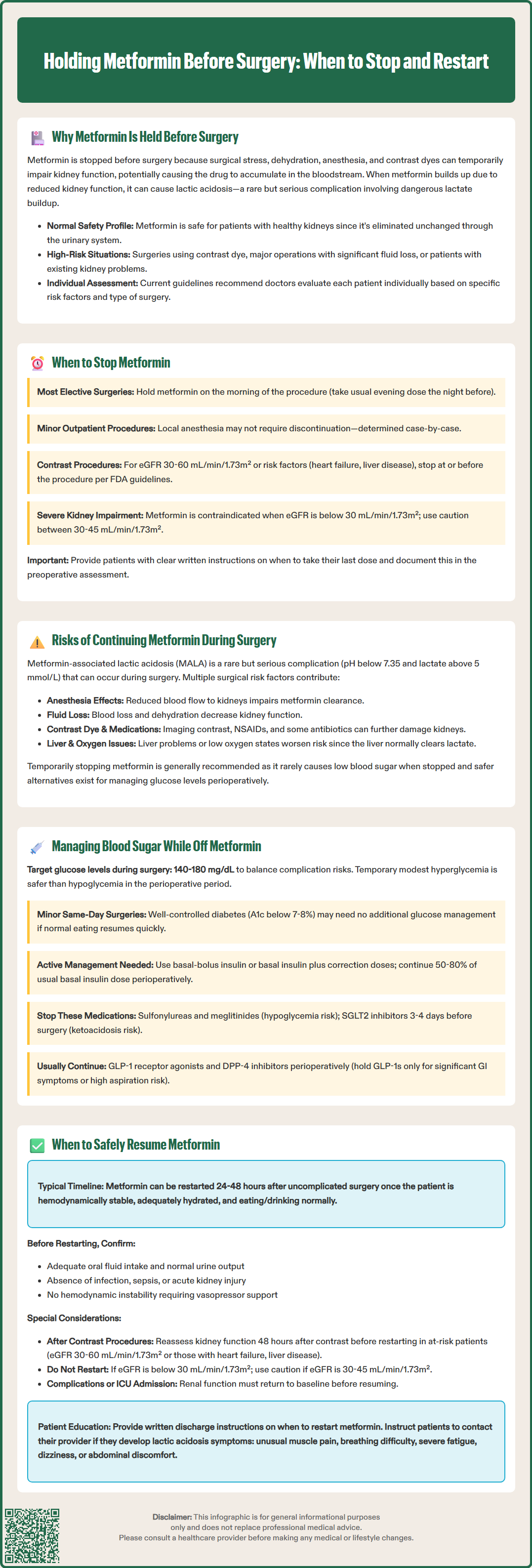
The primary risk of continuing metformin through the perioperative period is metformin-associated lactic acidosis (MALA), a rare but serious condition characterized by metabolic acidosis with pH below 7.35 and lactate levels exceeding 5 mmol/L. While MALA is uncommon in patients with normal kidney function, the surgical environment creates multiple risk factors that can precipitate this complication.
Surgical stress triggers a cascade of physiological responses that can compromise metformin clearance. Anesthesia can cause vasodilation and reduced cardiac output, decreasing renal perfusion. Intraoperative blood loss, third-spacing of fluids, and inadequate fluid replacement can lead to hypovolemia and prerenal azotemia. Certain procedures, particularly those involving the gastrointestinal or urinary tracts, carry infection risks that can progress to sepsis, further impairing tissue perfusion and oxygen delivery. These hypoperfusion states reduce the kidney's ability to excrete metformin while simultaneously increasing lactate production in hypoxic tissues.
Additional perioperative factors compound these risks. Administration of iodinated contrast media for imaging studies can increase the risk of post-contrast acute kidney injury, particularly in patients with diabetes or pre-existing renal impairment. Certain medications used during surgery, including nonsteroidal anti-inflammatory drugs and some antibiotics, can further compromise kidney function. Pre-existing hepatic impairment or hypoxic states can impair lactate metabolism, as the liver is the primary site of lactate clearance.
Regarding glycemic effects, metformin alone rarely causes hypoglycemia, even during fasting. However, the perioperative period involves complex metabolic changes, and patients on multiple glucose-lowering medications may experience unpredictable glycemic patterns. The risk-benefit analysis consistently favors temporary discontinuation in most surgical contexts, given the availability of alternative strategies for perioperative glucose management.
Maintaining glycemic control during the perioperative period when metformin is held requires a tailored approach based on the duration of discontinuation, baseline glucose control, and the nature of the surgical procedure. For patients undergoing minor same-day procedures with metformin held only on the morning of surgery, no additional glucose management may be necessary if baseline hemoglobin A1c is well-controlled (below 7-8%) and the patient resumes normal eating quickly postoperatively.
For longer periods off metformin or more extensive surgeries, several management strategies exist. Patients with well-controlled diabetes (A1c below 7%) may be monitored with point-of-care glucose testing every 4-6 hours without immediate intervention, treating only if glucose exceeds 180 mg/dL. This approach recognizes that temporary modest hyperglycemia is generally safer than hypoglycemia in the perioperative setting. Target glucose ranges during surgery typically aim for 140-180 mg/dL, balancing the risks of hyperglycemia-related complications against hypoglycemia.
For patients requiring active glucose management, insulin remains the most flexible and titratable option. The American Diabetes Association and Endocrine Society discourage the use of sliding-scale insulin alone. Instead, a basal-bolus regimen or basal insulin plus correction doses is preferred. Patients already using basal insulin should typically continue 50-80% of their usual dose during the perioperative period. Intravenous insulin infusions provide the most precise control for major surgeries or critically ill patients, allowing minute-to-minute titration based on hourly glucose monitoring.
Other oral diabetes medications should also be reviewed during this period. Sulfonylureas and meglitinides should generally be held due to hypoglycemia risk during fasting. SGLT2 inhibitors require discontinuation before surgery (canagliflozin, dapagliflozin, and empagliflozin: 3 days; ertugliflozin: 4 days) due to concerns about euglycemic diabetic ketoacidosis. DPP-4 inhibitors may be continued in most cases. According to 2024 multi-society guidance, most patients can continue GLP-1 receptor agonists perioperatively, with consideration for holding only in patients with significant gastrointestinal symptoms or high aspiration risk. Patients should receive clear instructions about which medications to hold and which to continue, with specific guidance about timing.
The decision to restart metformin after surgery requires careful assessment of kidney function, hemodynamic stability, and resumption of normal oral intake. For uncomplicated outpatient procedures in patients with normal baseline renal function who are eating and drinking normally, metformin can typically be resumed 24-48 hours after surgery once the patient is hemodynamically stable and adequately hydrated. This conservative approach allows time for any procedure-related physiological stress to resolve and ensures the kidneys are functioning adequately to clear the medication.
Before restarting metformin, several clinical criteria should be met. The patient should be maintaining adequate oral fluid intake without significant nausea or vomiting. Urine output should be normal, indicating adequate kidney perfusion. There should be no signs of infection, sepsis, acute kidney injury, or ongoing hemodynamic instability requiring vasopressor support or large-volume fluid resuscitation.
For procedures involving iodinated contrast media, FDA labeling recommends reassessing renal function 48 hours after contrast administration before restarting metformin in at-risk patients (eGFR 30-60 mL/min/1.73m², hepatic impairment, alcoholism, heart failure, or those receiving intra-arterial contrast). For other patients with normal renal function receiving intravenous contrast, the American College of Radiology indicates metformin can be continued if eGFR is ≥30 mL/min/1.73m² and there is no acute kidney injury.
Patients who experienced significant intraoperative complications, required intensive care admission, or developed acute kidney injury require more cautious management. Metformin should remain held until renal function returns to baseline or near-baseline levels and the patient is hemodynamically stable. Metformin is contraindicated if eGFR is <30 mL/min/1.73m² and should be used with caution if eGFR is 30-45 mL/min/1.73m².
Clear discharge instructions are essential for patient safety. Patients should receive written guidance specifying when to restart metformin, typically with the first meal after the specified waiting period. They should be counseled to contact their healthcare provider if they develop symptoms potentially indicating lactic acidosis, including unusual muscle pain, difficulty breathing, severe fatigue, dizziness, or abdominal discomfort. Follow-up appointments should include review of the medication restart plan and assessment of glycemic control during the transition period. For complex cases or patients with multiple comorbidities, coordination between the surgical team, anesthesiologist, and primary care provider or endocrinologist ensures safe medication resumption and optimal perioperative diabetes management.
For most elective surgeries, metformin is held on the morning of the procedure. Take your usual evening dose the night before surgery, but skip the morning dose on the day of the procedure.
Metformin is stopped to prevent lactic acidosis, a rare but serious complication that can occur when surgical stress, anesthesia, or dehydration impairs kidney function, causing metformin to accumulate in the bloodstream.
Metformin can typically be restarted 24-48 hours after uncomplicated surgery once you are eating and drinking normally, hemodynamically stable, and have adequate kidney function. For procedures involving contrast dye, renal function should be reassessed before restarting in at-risk patients.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.