LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is a GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management. Understanding how long semaglutide stays in your system is essential for treatment planning, medication transitions, pregnancy considerations, and managing side effects. With a half-life of approximately one week, semaglutide remains in the body for about five weeks after the final dose. This extended presence influences clinical decisions around surgery, switching medications, and discontinuation strategies. This article examines semaglutide's pharmacokinetics, elimination timeline, and practical implications for patients and healthcare providers.
Quick Answer: Semaglutide remains in your system for approximately 5 weeks after the final dose, based on its one-week half-life and standard elimination principles.
Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Available under brand names including Ozempic, Wegovy, and Rybelsus, this medication mimics the action of naturally occurring GLP-1, a hormone that plays a crucial role in glucose regulation and appetite control.
The mechanism of action involves binding to GLP-1 receptors located throughout the body, particularly in the pancreas, brain, and gastrointestinal tract. In pancreatic beta cells, semaglutide stimulates glucose-dependent insulin secretion, meaning it promotes insulin release only when blood glucose levels are elevated. This reduces the risk of hypoglycemia compared to some other diabetes medications, though this risk increases when semaglutide is used with insulin or sulfonylureas. Simultaneously, it suppresses glucagon secretion from pancreatic alpha cells, further contributing to improved glycemic control.
Beyond glycemic effects, semaglutide slows gastric emptying, which prolongs the sensation of fullness after meals and reduces appetite through central nervous system pathways. This dual action on glucose metabolism and satiety explains its efficacy in both diabetes management and weight reduction. The medication is structurally modified to resist degradation by the enzyme dipeptidyl peptidase-4 (DPP-4) and includes an albumin-binding side chain, which extends its duration of action compared to native GLP-1.
Important safety information: Semaglutide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
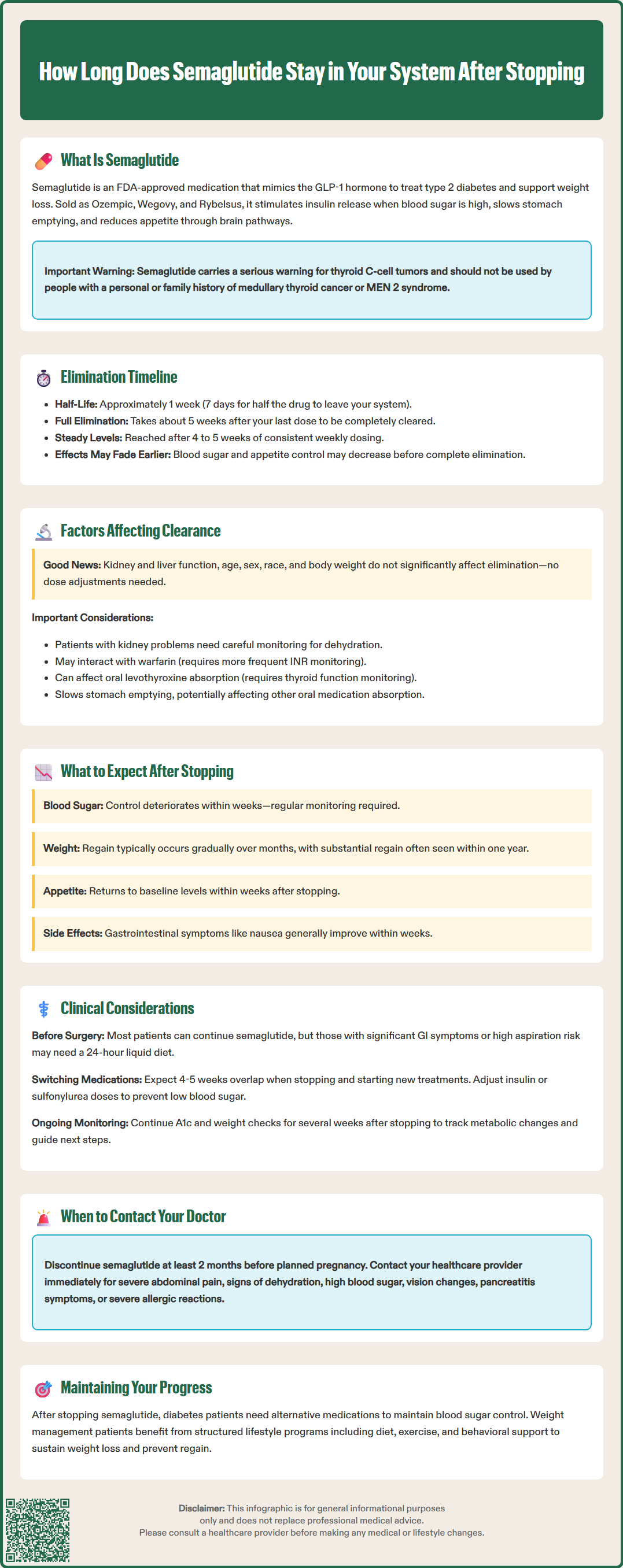
Semaglutide has a terminal half-life of approximately 1 week (about 7 days or 168 hours), according to FDA prescribing information. The half-life represents the time required for the plasma concentration of the drug to decrease by 50%. This relatively long half-life is a result of the medication's structural modifications, particularly its binding to serum albumin and resistance to enzymatic breakdown.
Based on standard pharmacokinetic principles, it takes approximately five half-lives for a medication to be essentially eliminated from the body, reaching less than 3% of the original concentration. For semaglutide, this translates to a clearance period of approximately 5 weeks after the final dose. This elimination timeline applies to both injectable formulations (Ozempic and Wegovy) and the oral formulation (Rybelsus), though the latter requires daily administration due to its absorption characteristics.
The subcutaneous formulations are administered once weekly, with steady-state concentrations achieved after approximately 4 to 5 weeks of consistent dosing. While the drug is largely eliminated within 5 weeks of the last dose, the pharmacodynamic effects—the actual clinical impact on blood glucose and appetite—may begin to wane earlier as concentrations fall below therapeutic thresholds.
This prolonged systemic presence has important implications for treatment planning, particularly when considering pregnancy, switching medications, or managing adverse effects. Patients and clinicians should be aware that semaglutide's effects gradually diminish over several weeks following discontinuation.
Several physiological and clinical factors can influence the elimination rate of semaglutide, though the medication's pharmacokinetics are generally consistent across most patient populations. Renal function has minimal impact on semaglutide clearance. According to FDA labeling, no dose adjustment is required for patients with renal impairment, including those with end-stage renal disease (ESRD). Semaglutide is primarily degraded proteolytically rather than excreted unchanged by the kidneys. However, patients with renal impairment may be at higher risk for dehydration from gastrointestinal side effects, which requires clinical vigilance.
Hepatic function similarly shows minimal impact on semaglutide elimination. FDA labeling indicates no clinically relevant pharmacokinetic changes across the spectrum of hepatic impairment (Child-Pugh classes A-C), and no dose adjustment is recommended based on hepatic function. Body weight and composition may theoretically influence distribution volume, but clinical studies have not demonstrated clinically significant differences in elimination based on body mass index or weight alone.
Age does not appear to meaningfully alter semaglutide pharmacokinetics, and no dose adjustments are recommended for elderly patients. Similarly, sex and race have not been shown to significantly affect drug clearance. However, individual variability in albumin levels, metabolic rate, and overall health status can contribute to minor differences in how long the medication remains active.
Regarding drug interactions, while semaglutide has few direct interactions affecting its elimination, patients should be aware of two important considerations: 1) Monitor INR more frequently when initiating semaglutide in patients taking warfarin, and 2) Increased levothyroxine exposure may occur with oral semaglutide (Rybelsus), requiring monitoring of thyroid function tests. Additionally, semaglutide's effect on gastric emptying can alter the absorption of other oral medications.
Discontinuing semaglutide results in a gradual decline in therapeutic benefits over several weeks as the medication is eliminated from the body. Blood glucose control in patients with type 2 diabetes may begin to deteriorate within weeks after the last dose, with effects diminishing as drug levels decline. The exact timeline varies by individual, making regular glucose monitoring essential during this transition period.
Weight regain is a common concern following semaglutide discontinuation. Clinical studies, including the STEP trial extensions, have demonstrated that many patients experience gradual weight increase after stopping treatment. Weight regain typically occurs over months, with substantial regain often seen within one year of discontinuation. Appetite and food intake patterns often return toward baseline levels within weeks after stopping treatment. The rate and extent of weight regain vary considerably among individuals and depend on lifestyle factors, dietary habits, and physical activity levels maintained after discontinuation.
Adverse effects, if present during treatment, typically resolve gradually as drug concentrations decline. Gastrointestinal symptoms such as nausea, which are among the most common side effects, generally improve within weeks after the final dose, though individual experiences vary.
Important safety considerations include the recommendation to discontinue semaglutide at least 2 months before a planned pregnancy, as specified in FDA labeling. Patients should contact their healthcare provider promptly for severe or persistent abdominal pain (possible pancreatitis or gallbladder disease), signs of dehydration from vomiting or diarrhea, marked hyperglycemia, or new/worsening vision changes. Patients should work closely with their healthcare provider to implement alternative diabetes management or weight maintenance strategies before stopping semaglutide.
Healthcare providers must account for semaglutide's systemic presence when making clinical decisions. Preoperative planning requires particular attention: according to 2024 multi-society guidance (including the American Society of Anesthesiologists), most patients can continue GLP-1 receptor agonists perioperatively. Individualized planning is recommended based on gastrointestinal symptoms and aspiration risk. For patients with significant GI symptoms or high aspiration risk, a 24-hour liquid diet before surgery may be considered. Clear communication between surgical and anesthesia teams remains essential.
Medication switching presents unique challenges. When transitioning from semaglutide to another diabetes medication, clinicians should anticipate overlapping drug effects for several weeks. Conversely, when switching to semaglutide from shorter-acting agents, the gradual onset of full therapeutic effect (4 to 5 weeks to steady state) must be considered. Careful glucose monitoring during transition periods helps prevent both hyperglycemia and hypoglycemia. Dose adjustments of insulin or sulfonylureas are often necessary when starting or stopping semaglutide to mitigate hypoglycemia risk.
Adverse event management may require patience given the gradual elimination of the medication. For persistent gastrointestinal symptoms or other tolerability issues, supportive care and symptomatic treatment are the primary approaches while awaiting natural drug elimination. Monitoring for gallbladder disease and acute kidney injury (particularly from dehydration) is important. In cases of serious adverse effects such as acute pancreatitis or severe allergic reactions, discontinuation is warranted with appropriate specialist referral.
Laboratory monitoring should continue for several weeks after discontinuation, particularly hemoglobin A1c and weight measurements, to assess metabolic trajectory and guide subsequent management. Patients with type 2 diabetes require alternative pharmacotherapy to maintain glycemic targets, while those using semaglutide for weight management benefit from structured lifestyle intervention programs to sustain weight loss.
Weight regain typically begins within weeks after discontinuation as appetite returns toward baseline, with substantial regain often occurring within one year. The rate and extent vary considerably based on maintained lifestyle factors, dietary habits, and physical activity levels.
Yes, patients with type 2 diabetes require alternative pharmacotherapy to maintain glycemic targets after stopping semaglutide. Blood glucose control may begin deteriorating within weeks, making regular monitoring and medication adjustments essential during the transition period.
Gastrointestinal side effects such as nausea typically improve gradually within weeks after the final dose as drug concentrations decline. Individual experiences vary, but most adverse effects resolve as the medication is eliminated over the 5-week clearance period.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.