LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
How long does it take for oral semaglutide to work? Many patients starting Rybelsus® for type 2 diabetes want to know when they'll see results. Oral semaglutide, the first GLP-1 receptor agonist available in tablet form, works gradually rather than immediately. While some early effects on blood sugar may appear within 2-4 weeks, meaningful improvements in hemoglobin A1c typically require 12-16 weeks at the maintenance dose. Understanding this timeline helps set realistic expectations and supports treatment adherence during the critical early months of therapy.
Quick Answer: Oral semaglutide typically requires 12-16 weeks to achieve maximal reductions in hemoglobin A1c, though some blood sugar improvements may appear within 2-4 weeks of starting treatment.
Oral semaglutide (marketed as Rybelsus®) is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) approved by the FDA for the treatment of type 2 diabetes mellitus in adults. It represents the first and only oral formulation of a GLP-1 receptor agonist, offering an alternative to injectable semaglutide preparations. The medication is available in 3 mg, 7 mg, and 14 mg tablets, with dosing typically initiated at the lowest strength and titrated upward based on glycemic response and tolerability.
The mechanism of action involves mimicking the endogenous incretin hormone GLP-1, which plays a crucial role in glucose homeostasis. Semaglutide binds to and activates GLP-1 receptors on pancreatic beta cells, stimulating glucose-dependent insulin secretion. This means insulin release occurs primarily when blood glucose levels are elevated, reducing the risk of hypoglycemia compared to some other antidiabetic agents. Additionally, semaglutide suppresses glucagon secretion from pancreatic alpha cells, further contributing to improved glycemic control.
Beyond its effects on pancreatic hormone secretion, oral semaglutide slows gastric emptying, which moderates the postprandial rise in blood glucose. It also acts on appetite-regulating centers in the brain, promoting satiety and reducing caloric intake. These combined mechanisms result in both improved glycemic parameters and modest weight reduction in many patients. The oral formulation utilizes a specialized absorption enhancer (SNAC) to facilitate absorption across the gastric mucosa, as peptide medications are typically degraded in the gastrointestinal tract.
Importantly, Rybelsus is not FDA-approved for chronic weight management and should not be used for weight loss. It is not indicated for type 1 diabetes or diabetic ketoacidosis. Rybelsus carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Tablets should be swallowed whole and not split, crushed, or chewed. Semaglutide products (Rybelsus, Ozempic, Wegovy) are not interchangeable on a mg-to-mg basis.
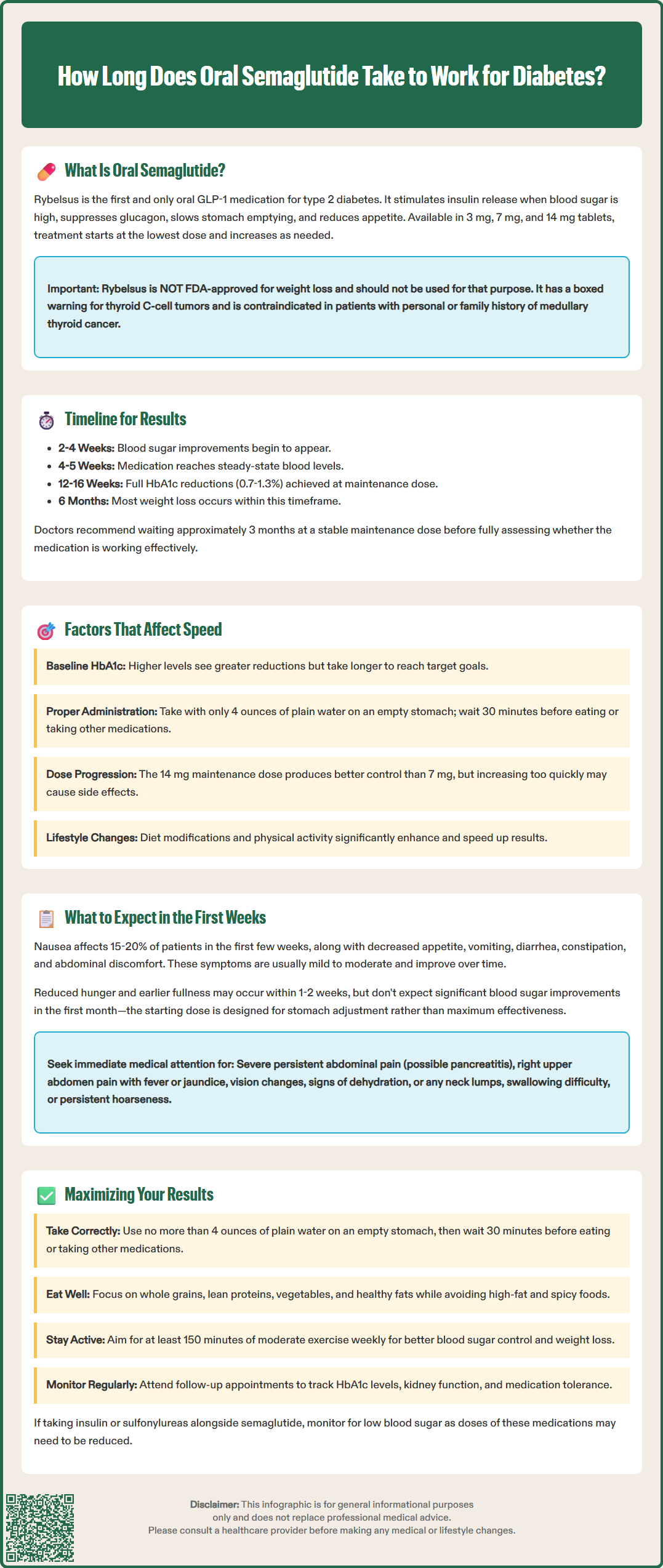
The timeline for oral semaglutide to demonstrate clinical effects varies depending on the specific outcome being measured. Pharmacologically, the medication reaches steady-state plasma concentrations after approximately 4 to 5 weeks of daily administration at a consistent dose. However, patients and clinicians should understand that pharmacokinetic steady state does not necessarily correspond to maximal therapeutic benefit.
For glycemic control, measurable reductions in fasting plasma glucose may be observed within the first 2 to 4 weeks of treatment, though individual responses vary considerably. More substantial improvements in hemoglobin A1c (HbA1c)—the primary marker of long-term glycemic control—typically require 12 to 16 weeks to become fully apparent. Clinical trials have demonstrated that maximal HbA1c reduction generally occurs after approximately 3 to 4 months of therapy at the maintenance dose. In the PIONEER clinical trials, mean HbA1c reductions ranged from approximately 0.7% to 1.3%, depending on the dose and baseline characteristics. The American Diabetes Association recommends reassessing glycemic control and treatment efficacy after approximately 3 months of therapy at a stable maintenance dose.
Weight loss effects, when they occur, tend to follow a more gradual trajectory. Patients may notice modest weight reduction within the first month, but clinically meaningful weight loss typically accumulates over several months. In pivotal trials, the majority of weight loss occurred within the first 6 months of treatment, with some continued gradual reduction thereafter.
It is important to emphasize that oral semaglutide is initiated at a sub-therapeutic dose (3 mg daily) for the first 30 days to improve gastrointestinal tolerability. This means that patients should not expect optimal therapeutic effects during the initial month. The dose is then increased to 7 mg daily, and may be further escalated to 14 mg daily after an additional 30 days if greater glycemic control is needed and the medication is well-tolerated.
Multiple patient-specific and medication-related factors influence the rate and magnitude of response to oral semaglutide. Understanding these variables helps set realistic expectations and optimize therapeutic outcomes.
Baseline glycemic status significantly impacts the observed response. Patients with higher baseline HbA1c levels typically experience greater absolute reductions in blood glucose, though they may require longer to achieve target glycemic goals. Conversely, those with HbA1c values closer to target may see more modest improvements but may reach therapeutic goals more quickly.
Adherence to administration instructions is critical for oral semaglutide due to its unique absorption requirements. The medication must be taken on an empty stomach with no more than 4 ounces of plain water, and patients must wait at least 30 minutes before consuming food, beverages, or other oral medications. Failure to follow these specific instructions can substantially reduce bioavailability, delaying or diminishing therapeutic effects. According to the FDA prescribing information, taking oral semaglutide with food or beverages markedly reduces absorption.
Dose escalation schedule directly affects the timeline to therapeutic effect. Patients who tolerate dose increases well and progress to the 14 mg maintenance dose typically achieve greater glycemic improvements than those who remain at 7 mg. However, aggressive dose escalation may increase gastrointestinal adverse effects, potentially compromising adherence.
Concomitant medications and therapies also play a role. Patients taking other glucose-lowering agents may experience more rapid glycemic improvements, though this must be balanced against increased hypoglycemia risk when combined with insulin or sulfonylureas. Oral semaglutide increases levothyroxine exposure, so thyroid function should be monitored in patients taking both medications. Other oral medications should be taken at least 30 minutes after Rybelsus. Additionally, combining GLP-1 RAs with DPP-4 inhibitors is generally not recommended due to minimal additive efficacy. Lifestyle modifications—including dietary changes and increased physical activity—can substantially enhance and accelerate the medication's effects on both glycemic control and body weight.
The initial weeks of oral semaglutide therapy represent a critical adjustment period during which patients should be prepared for both potential benefits and common adverse effects. Setting appropriate expectations during this time can improve adherence and treatment satisfaction.
Gastrointestinal symptoms are the most frequently reported adverse effects during the early treatment period. Nausea occurs in approximately 15-20% of patients and is typically most pronounced during the first few weeks after initiating therapy or increasing the dose. Other common gastrointestinal effects include decreased appetite, occasional vomiting, diarrhea, constipation, and abdominal discomfort. These symptoms are generally mild to moderate in severity and tend to diminish over time as physiologic adaptation occurs. If vomiting occurs after taking a dose, do not take another tablet until the next scheduled dose. Patients should be counseled that these effects are expected and usually transient, though they should report severe or persistent symptoms to their healthcare provider.
Early metabolic changes may include modest reductions in fasting blood glucose and decreased appetite. Some patients notice reduced hunger and earlier satiety within the first 1-2 weeks, even at the 3 mg starting dose. However, clinically significant improvements in overall glycemic control should not be expected during the initial month, as this dose is primarily intended for gastrointestinal adaptation rather than maximal therapeutic effect.
Monitoring recommendations during the early treatment period include regular self-monitoring of blood glucose, particularly for patients taking insulin or sulfonylureas, as dose adjustments of these medications may be necessary to prevent hypoglycemia. Patients should be alert for signs of pancreatitis (severe, persistent abdominal pain radiating to the back), gallbladder disease (persistent pain in the right upper abdomen, fever, or jaundice), and dehydration that could lead to acute kidney injury. Those with preexisting diabetic retinopathy should report any visual changes, as rapid improvement in blood glucose can temporarily worsen retinopathy. Patients should also be aware of the boxed warning regarding thyroid C-cell tumors and report any symptoms such as a lump in the neck, difficulty swallowing, or persistent hoarseness.
Rybelsus is not recommended during pregnancy or breastfeeding and should be discontinued at least 2 months before a planned pregnancy. Patients should maintain consistent daily dosing at the same time each morning and strictly adhere to the administration instructions.
Optimizing therapeutic outcomes with oral semaglutide requires a comprehensive approach that extends beyond simply taking the medication. Evidence-based strategies can enhance both glycemic control and weight management while minimizing adverse effects.
Strict adherence to administration guidelines is paramount. Taking oral semaglutide with the stomach empty, using only plain water (no more than 4 ounces), and waiting a full 30 minutes before eating or taking other medications ensures optimal absorption. Setting a consistent morning routine—such as taking the medication immediately upon waking—can help establish this habit. Patients should avoid coffee, tea, or other beverages during the 30-minute waiting period, as these can significantly impair absorption. Always swallow the tablet whole; do not split, crush, or chew it. Take only one tablet once daily.
Lifestyle modifications work synergistically with semaglutide to improve outcomes. The American Diabetes Association emphasizes that pharmacologic therapy should complement, not replace, therapeutic lifestyle changes. A balanced diet emphasizing whole grains, lean proteins, vegetables, and healthy fats supports both glycemic control and weight management. Regular physical activity—aiming for at least 150 minutes of moderate-intensity aerobic exercise weekly, as recommended by the ADA Standards of Care—enhances insulin sensitivity and contributes to weight loss. These lifestyle interventions may accelerate the medication's effects and improve overall cardiometabolic health.
Managing gastrointestinal side effects can improve adherence and quality of life. Eating smaller, more frequent meals; avoiding high-fat and spicy foods; and staying well-hydrated may reduce nausea and other digestive symptoms. Some patients find that ginger tea or bland foods help manage nausea, but remember that any beverages (including ginger tea) should only be consumed outside the 30-minute post-dose window.
Regular monitoring and follow-up enable timely dose adjustments and identification of any safety concerns. Patients should attend scheduled appointments to assess HbA1c, renal function, and treatment tolerability. Those not achieving adequate glycemic control after 3-4 months at the maximum tolerated dose may require additional glucose-lowering therapy. Throughout treatment, patients taking insulin or sulfonylureas should continue to monitor for hypoglycemia, as dose reductions of these medications may be necessary. Open communication with healthcare providers about both benefits and adverse effects ensures personalized optimization of the treatment regimen.
Some patients may notice modest reductions in fasting blood glucose within 2-4 weeks, but the initial 3 mg dose is primarily for gastrointestinal adaptation. Clinically significant improvements in hemoglobin A1c typically require 12-16 weeks at the maintenance dose of 7 mg or 14 mg daily.
Oral semaglutide requires specific administration instructions because food and beverages markedly reduce its absorption. Taking it with only plain water (no more than 4 ounces) on an empty stomach, then waiting 30 minutes before eating, ensures optimal bioavailability and therapeutic effectiveness.
Nausea is common during the first few weeks and typically diminishes over time. Eating smaller, more frequent meals, avoiding high-fat and spicy foods, and staying well-hydrated may help manage symptoms. If nausea is severe or persistent, contact your healthcare provider to discuss management strategies.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.