LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
How to get tirzepatide out of your system is a common question for patients discontinuing Mounjaro or Zepbound. Tirzepatide is a dual GIP/GLP-1 receptor agonist with a 5-day half-life, meaning it takes approximately 25 days (3-4 weeks) for the medication to be substantially eliminated from your body after your final injection. Unlike some medications, there is no proven method to accelerate this natural clearance process. Understanding tirzepatide's elimination timeline is essential for managing side effects, planning surgical procedures, preparing for pregnancy, or transitioning to alternative therapies. This guide provides evidence-based information on clearance timelines, factors affecting elimination, and managing the transition period safely.
Quick Answer: Tirzepatide cannot be actively removed from your system; it must naturally clear over approximately 25 days (3-4 weeks) after your last injection through normal metabolic breakdown.
Tirzepatide (Mounjaro, Zepbound) is a long-acting glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist with a prolonged elimination half-life of approximately 5 days (around 120 hours). This pharmacokinetic property means that after your last dose, it takes roughly 5 days for half of the medication to be cleared from your bloodstream.
Based on standard pharmacokinetic principles, it typically takes 4 to 5 half-lives for a medication to be substantially eliminated from the body. For tirzepatide, this translates to approximately 25 days (3.5 to 4 weeks) after your final injection before the drug is largely cleared from your system. However, trace amounts may persist slightly longer in some individuals.
The medication is administered once weekly via subcutaneous injection, and its extended half-life is intentionally designed to maintain stable therapeutic levels between doses. After discontinuation, tirzepatide levels decline gradually rather than abruptly. Peak plasma concentrations occur 8 to 72 hours post-injection, and steady-state concentrations are achieved after approximately 4 weeks of consistent weekly dosing.
It's important to understand that even after tirzepatide is no longer detectable in blood samples, some physiological effects—particularly on gastric emptying and appetite regulation—may persist for a variable period as your body readjusts to baseline function. The FDA-approved prescribing information for both Mounjaro and Zepbound confirms these elimination timelines, which are consistent across the approved dose ranges (2.5 mg to 15 mg weekly).
Several physiological and clinical factors can influence how quickly tirzepatide is eliminated from your system, though the variation among individuals is generally modest compared to some other medications.
Renal function has minimal impact on tirzepatide clearance. According to FDA labeling, no clinically meaningful differences in tirzepatide pharmacokinetics have been observed across all levels of renal function, including severe renal impairment and end-stage renal disease. No dose adjustment is required for patients with kidney impairment.
Hepatic function similarly has minimal impact on tirzepatide clearance. The medication is primarily eliminated through protein catabolism rather than traditional hepatic metabolism, meaning liver disease typically does not substantially affect elimination rates. No dose adjustments are recommended for patients with hepatic impairment based on current evidence.
Body weight and composition contribute to normal population variability in pharmacokinetics. Tirzepatide has been studied across a wide range of body weights (from 40 kg to over 200 kg), with only minor differences in exposure that are not clinically significant enough to warrant dose modifications.
Age does not appear to meaningfully affect tirzepatide elimination. Studies have included patients ranging from young adults to those over 75 years, with no clinically relevant age-related differences in pharmacokinetics. Similarly, sex does not significantly impact elimination rates, and no gender-based dosing adjustments are necessary.
It's worth noting that tirzepatide's effect on slowing gastric emptying may affect the absorption of oral medications taken concurrently. This is particularly important for medications with a narrow therapeutic index or those requiring rapid onset of action.
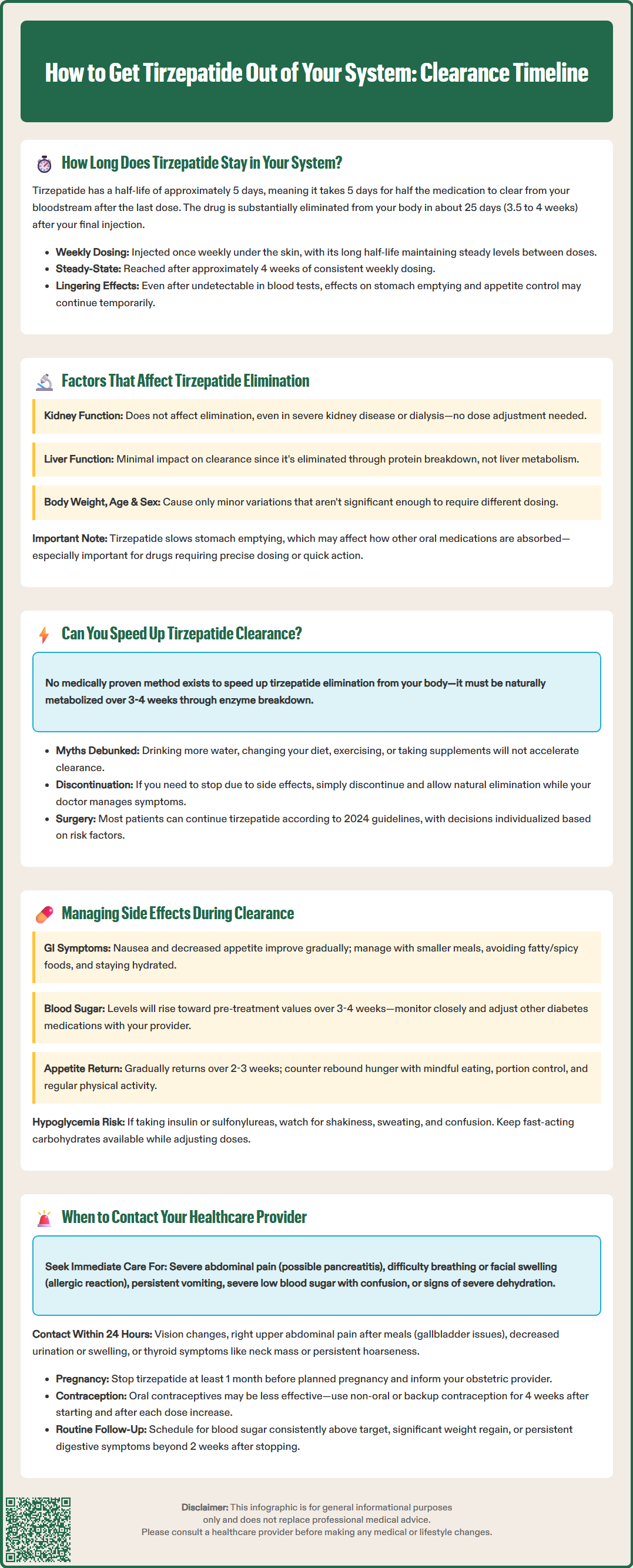
There is no medically proven method to accelerate the elimination of tirzepatide from your system once it has been administered. Unlike some medications that can be removed through dialysis or specific antidotes, tirzepatide must be naturally metabolized and cleared by your body over its predetermined timeframe.
The medication is eliminated primarily through proteolytic degradation—meaning it is broken down by enzymes into smaller peptide fragments and amino acids, which are then processed through normal metabolic pathways. This biological process cannot be meaningfully hastened through dietary changes, increased fluid intake, exercise, or any over-the-counter supplements. Claims suggesting otherwise lack scientific support and should be viewed with skepticism.
Hydration is important for overall health and kidney function, but increasing water intake will not significantly speed tirzepatide clearance since the drug is not primarily eliminated unchanged through the kidneys. Similarly, there is no evidence that specific foods, herbal supplements, or detoxification regimens can accelerate elimination.
If you are experiencing concerning side effects or need to discontinue tirzepatide for medical reasons (such as upcoming surgery or pregnancy), the most appropriate approach is to simply stop taking the medication and allow natural elimination to occur over the expected 3-to-4-week timeframe. Your healthcare provider can offer supportive care for any symptoms during this period.
For patients requiring surgical procedures, recent 2024 multi-society guidance (including the American Society of Anesthesiologists) indicates that most patients can continue GLP-1 receptor agonists perioperatively. Management should be individualized based on risk factors for delayed gastric emptying, with strategies such as a 24-hour liquid diet before surgery for higher-risk patients rather than a blanket recommendation to discontinue the medication.
As tirzepatide gradually clears from your system over 3 to 4 weeks, you may experience a transition period during which side effects evolve and your body readjusts to functioning without the medication's effects.
Gastrointestinal symptoms—including nausea, decreased appetite, and altered bowel habits—are among the most common side effects during active treatment. These typically improve gradually as drug levels decline, though some patients report a temporary worsening of nausea during the first week after discontinuation before improvement occurs. Managing these symptoms includes eating smaller, more frequent meals; avoiding high-fat or spicy foods; staying adequately hydrated; and considering over-the-counter remedies such as ginger or vitamin B6 for nausea (though evidence for these specific remedies is limited). If symptoms are severe or persistent, discuss prescription antiemetics with your healthcare provider.
Blood glucose changes are particularly important to monitor if you have type 2 diabetes. As tirzepatide leaves your system, its glucose-lowering effects will diminish, and blood sugar levels may rise toward pre-treatment values. Patients should work closely with their healthcare provider to adjust other diabetes medications appropriately and monitor glucose levels more frequently during this transition period. The American Diabetes Association recommends individualized glucose targets and medication adjustments based on regular monitoring.
Hypoglycemia risk requires special attention if you take tirzepatide with insulin or sulfonylureas. As tirzepatide levels decrease, these medications may need dose adjustments to prevent low blood sugar. Monitor for symptoms like shakiness, sweating, confusion, or dizziness and have a fast-acting carbohydrate source available.
Appetite and weight changes may occur as the medication's appetite-suppressing effects wane. Many patients notice a gradual return of appetite over 2 to 3 weeks, which can be managed through mindful eating practices, portion control, and maintaining regular physical activity. Some individuals may experience rebound hunger, making behavioral strategies particularly important during this period.
Injection site reactions, if present, typically resolve within days of the last injection. Supportive care with cool compresses and over-the-counter antihistamines may provide relief if needed.
While tirzepatide elimination is generally well-tolerated, certain situations warrant prompt medical attention during the discontinuation period.
Seek immediate medical care if you experience: severe, persistent abdominal pain (particularly if radiating to the back), which could indicate pancreatitis; signs of severe allergic reaction including difficulty breathing, facial swelling, or widespread rash; persistent vomiting preventing fluid intake; symptoms of severe hypoglycemia such as confusion or loss of consciousness; or symptoms of severe dehydration such as decreased urination, dizziness, or confusion. These represent potentially serious complications requiring urgent evaluation.
Contact your healthcare provider within 24 hours if you develop: significant changes in vision; symptoms of gallbladder disease (right upper abdominal pain, especially after meals, with nausea); signs of kidney problems including decreased urination or swelling; or symptoms of thyroid abnormalities such as a neck mass, persistent hoarseness, or difficulty swallowing. Tirzepatide carries a boxed warning about thyroid C-cell tumors observed in rodent studies and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Any concerning thyroid symptoms should be promptly evaluated.
Schedule a routine follow-up if you experience: blood glucose levels consistently above your target range (for patients with diabetes); significant weight regain or difficulty managing appetite; persistent gastrointestinal symptoms beyond 2 weeks after discontinuation; or questions about transitioning to alternative diabetes or weight management therapies.
Patients who discontinued tirzepatide due to planned pregnancy should inform their obstetric provider, as the medication should be stopped at least 1 month before a planned conception according to FDA labeling. Those who discontinued for upcoming surgery should ensure their surgical team is aware of recent tirzepatide use, as delayed gastric emptying effects may persist beyond complete drug elimination.
Women using oral contraceptives should be aware that tirzepatide may reduce the effectiveness of these medications due to delayed gastric emptying. The FDA recommends using a non-oral contraceptive method or a backup method for 4 weeks after starting tirzepatide and after each dose increase.
Your healthcare provider can help develop an individualized plan for monitoring and managing the transition off tirzepatide, including adjustments to other medications and strategies for maintaining therapeutic benefits achieved during treatment.
Tirzepatide takes approximately 25 days (3-4 weeks) to be substantially eliminated from your system after your final injection. With a half-life of 5 days, it requires 4-5 half-lives for the medication to be largely cleared, though trace amounts may persist slightly longer in some individuals.
No, increased water intake will not significantly speed tirzepatide clearance. The medication is eliminated primarily through protein breakdown rather than kidney excretion, so hydration does not accelerate the elimination process beyond supporting normal kidney function.
As tirzepatide clears over 3-4 weeks, gastrointestinal symptoms typically improve gradually, appetite may return, and blood glucose levels may rise in patients with diabetes. Some patients experience temporary symptom fluctuations during the first week after discontinuation before improvement occurs.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.