LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Many patients wonder whether tirzepatide loses effectiveness over time or what happens when treatment stops. Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) is a dual GIP and GLP-1 receptor agonist that maintains consistent therapeutic effects when taken as prescribed. Understanding how this medication works in your body, what occurs after discontinuation, and how to sustain results helps you make informed decisions about your treatment. This article examines tirzepatide's duration of action, factors affecting its effectiveness, and when to consult your healthcare provider about your therapy.
Quick Answer: Tirzepatide does not wear off during consistent use but its effects gradually diminish over 3-4 weeks after discontinuation as the medication clears from your system.
The medication enhances glucose-dependent insulin secretion from pancreatic beta cells, meaning it stimulates insulin release only when blood glucose levels are elevated. This mechanism reduces the risk of hypoglycemia, though this risk increases when tirzepatide is used with insulin or sulfonylureas. Simultaneously, tirzepatide suppresses glucagon secretion in a glucose-dependent manner, which helps prevent the liver from releasing excess glucose into the bloodstream. These combined actions help maintain more stable blood sugar levels throughout the day.
Tirzepatide also slows gastric emptying, which prolongs the feeling of fullness after meals and reduces appetite through central nervous system pathways. This gastric emptying effect may diminish somewhat over time (tachyphylaxis) despite continued use. The medication has a half-life of approximately five days, reaching steady-state concentrations after four weeks of consistent weekly dosing. This pharmacokinetic profile means the drug maintains therapeutic levels in your system between doses when taken as prescribed.
The dual receptor activation distinguishes tirzepatide from single GLP-1 receptor agonists. Clinical trials, including SURPASS-2, have demonstrated significant improvements in HbA1c levels and substantial weight loss compared to other treatments, with effects becoming apparent within the first few weeks of treatment and continuing to improve over several months of consistent use.
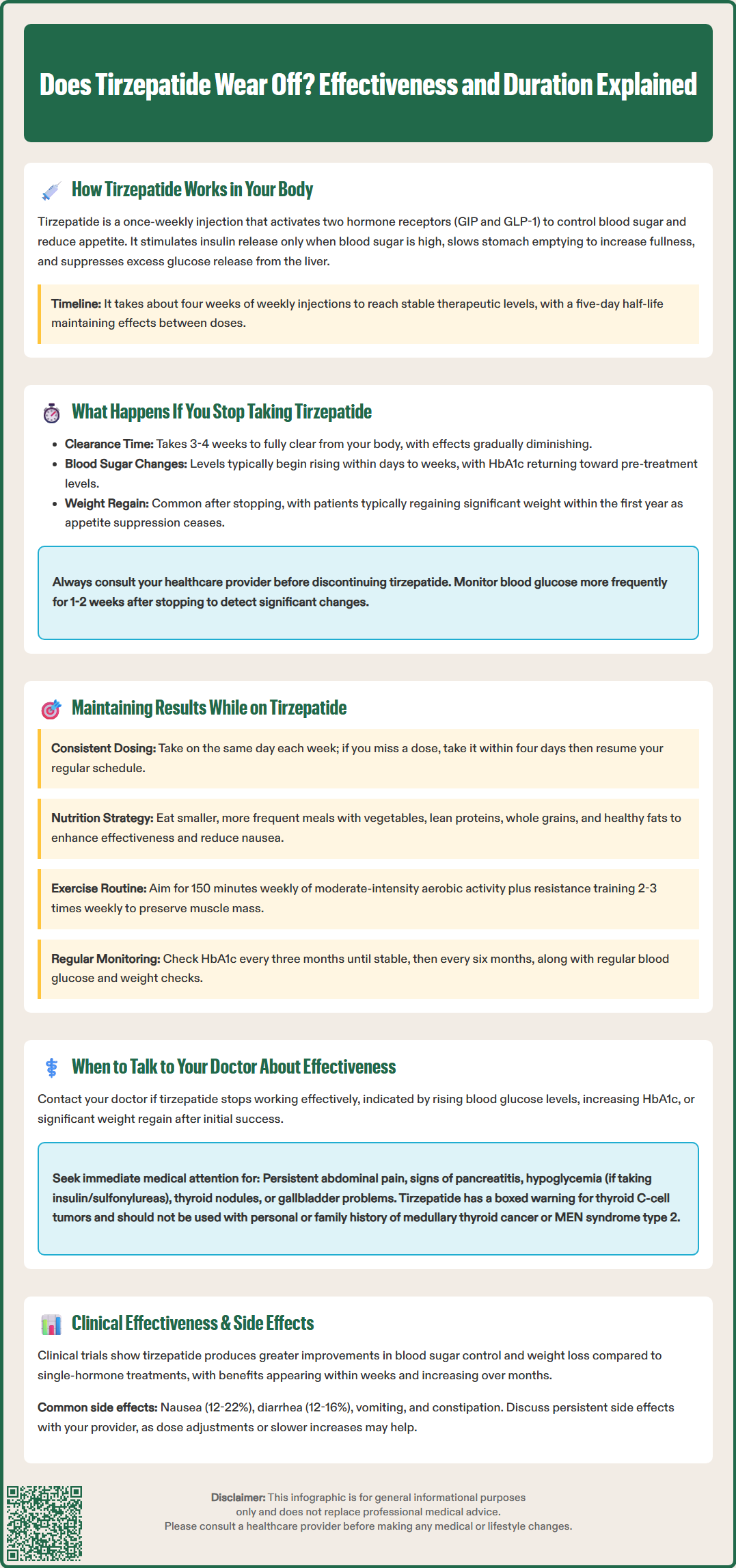
When you discontinue tirzepatide, the medication's effects gradually diminish as drug levels decline in your system. The drug is eliminated over approximately 3-4 weeks (about 4-5 half-lives), with most of the medication cleared from your body during this period. This is not a sudden "wearing off" but rather a gradual return to your body's baseline metabolic state without the medication's support.
Blood glucose values typically begin to rise within days to weeks after stopping tirzepatide, though HbA1c changes will take longer to appear since this test reflects average blood sugar over 2-3 months. Patients with type 2 diabetes often see their HbA1c levels rise back toward pre-treatment values over time. The American Diabetes Association emphasizes that type 2 diabetes is a chronic progressive condition requiring ongoing management, and discontinuing effective therapy without medical supervision can lead to worsening glycemic control and increased risk of diabetes-related complications.
Weight regain is another common consequence of stopping tirzepatide. Clinical studies, including SURMOUNT-4, have shown that patients who discontinue GLP-1 receptor agonists typically regain a significant portion of lost weight within the first year. This occurs because the appetite-suppressing effects cease, gastric emptying returns to normal speed, and the metabolic advantages provided by the medication are no longer present. The rate and extent of weight regain vary considerably among individuals and depend heavily on lifestyle factors maintained after discontinuation.
It's important to discuss stopping tirzepatide with your healthcare provider before making any changes. Your doctor may need to adjust other diabetes medications, implement alternative weight management strategies, or address underlying reasons for discontinuation. Consider increasing blood glucose monitoring for 1-2 weeks after stopping, as some patients may experience changes in blood sugar levels, making medical supervision during any treatment changes essential for your safety and continued health management.
Sustaining the benefits of tirzepatide requires consistent medication adherence combined with comprehensive lifestyle modifications. Taking your weekly injection on the same day each week helps maintain steady therapeutic drug levels and optimizes metabolic effects. Missing doses or irregular administration can lead to fluctuating blood sugar control and diminished weight management results. If you miss a dose, FDA labeling recommends taking it as soon as possible within four days, then resuming your regular schedule.
Dietary modifications significantly enhance tirzepatide's effectiveness and help maintain long-term results. Focus on a balanced diet rich in vegetables, lean proteins, whole grains, and healthy fats while limiting processed foods and added sugars. Because tirzepatide slows gastric emptying, eating smaller, more frequent meals may improve tolerability and reduce gastrointestinal side effects such as nausea, which affects approximately 12-22% of patients depending on dose. Adequate hydration is essential, particularly given the medication's effects on appetite and potential for reduced fluid intake.
Regular physical activity complements tirzepatide's metabolic benefits and is fundamental to sustained weight management and glycemic control. The American Diabetes Association and U.S. Department of Health and Human Services recommend at least 150 minutes of moderate-intensity aerobic activity weekly, along with resistance training 2-3 times weekly. Exercise improves insulin sensitivity, supports cardiovascular health, and helps preserve lean muscle mass during weight loss—all critical factors for maintaining results.
Routine monitoring helps ensure continued effectiveness. Regular HbA1c testing (typically every three months until stable, then potentially every six months), self-monitoring of blood glucose as directed, and periodic weight checks allow you and your healthcare provider to assess treatment response. Tirzepatide is available in escalating doses (2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, and 15 mg), with 2.5 mg used as an initiation dose for 4 weeks before escalating. If you're also taking insulin or sulfonylureas, dose adjustments of these medications may be needed to reduce hypoglycemia risk. Maintaining open communication with your healthcare team about your progress, challenges, and any side effects ensures optimal ongoing management.
Schedule a conversation with your healthcare provider if you notice diminishing effectiveness of tirzepatide despite consistent use. Signs that warrant discussion include rising fasting blood glucose readings, increasing HbA1c levels on routine testing, or weight loss plateau or regain after initial success. While some stabilization of weight loss is normal after several months, significant regain or lack of glycemic improvement may indicate the need for dose adjustment or evaluation of other contributing factors.
Certain situations require prompt medical attention rather than waiting for your next scheduled appointment. Contact your doctor immediately if you experience severe or persistent gastrointestinal symptoms including severe abdominal pain, persistent nausea and vomiting, or signs of pancreatitis. Seek urgent care for symptoms of hypoglycemia if you're also taking insulin or sulfonylureas. Additionally, seek guidance if you develop symptoms of thyroid nodules (neck lump, difficulty swallowing, persistent hoarseness), or gallbladder problems (persistent right upper quadrant pain, fever, jaundice). Note that tirzepatide carries a boxed warning regarding thyroid C-cell tumors observed in animal studies and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
Discuss medication effectiveness if you're experiencing significant side effects that interfere with adherence. Common adverse effects include nausea (12-22%), diarrhea (12-16%), vomiting (6-9%), and constipation (6-7%), with rates varying by dose. While these often improve after the first few weeks, persistent symptoms may require dose adjustment, slower titration, or additional supportive measures. Your doctor can help balance therapeutic benefits against tolerability concerns.
Bring up concerns about long-term treatment planning, including financial considerations, insurance coverage changes, or life circumstances affecting your ability to continue therapy. Your healthcare provider can explore alternative medications, adjust your diabetes management plan, or connect you with resources to maintain treatment continuity. Regular follow-up appointments—typically every three months until stable, then potentially every six months per ADA guidance—provide opportunities to assess ongoing effectiveness, review laboratory results, screen for complications, and adjust your treatment plan as needed to ensure optimal outcomes and sustained metabolic health.
Tirzepatide is eliminated over approximately 3-4 weeks after your last dose, with most of the medication cleared during this period. The drug has a half-life of about five days, meaning therapeutic effects gradually diminish rather than stopping suddenly.
Most patients regain a significant portion of lost weight within the first year after discontinuing tirzepatide, as appetite-suppressing effects cease and gastric emptying returns to normal. The extent of weight regain varies depending on lifestyle factors maintained after stopping treatment.
Tirzepatide maintains consistent effectiveness with regular weekly dosing, though some gastric emptying effects may diminish slightly over time. If you notice reduced effectiveness despite adherence, consult your healthcare provider about potential dose adjustment or other contributing factors.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.