LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Discontinuing tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) requires careful planning and medical supervision. This dual GIP/GLP-1 receptor agonist can typically be stopped without formal tapering, but the decision should never be made independently. Whether you're considering stopping due to achieving treatment goals, experiencing side effects, cost concerns, or pregnancy planning, understanding the safe discontinuation process and potential metabolic consequences is essential. This guide provides evidence-based information on how to stop taking tirzepatide safely, what to expect after discontinuation, and strategies for maintaining your health outcomes long-term.
Quick Answer: Tirzepatide can typically be stopped abruptly without tapering, but discontinuation should always be discussed with your healthcare provider to develop an individualized plan that addresses potential weight regain and glycemic control deterioration.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist with FDA-approved indications: Mounjaro for type 2 diabetes management and Zepbound for chronic weight management. This once-weekly subcutaneous injection works by enhancing insulin secretion in response to meals, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways. Tirzepatide is not indicated for type 1 diabetes management.
Patients may consider discontinuing tirzepatide for several legitimate reasons. Common scenarios include achieving target weight loss goals, experiencing intolerable adverse effects such as persistent nausea or gastrointestinal disturbances, financial constraints related to medication costs, pregnancy planning or confirmation (tirzepatide should be discontinued when pregnancy is recognized), or development of contraindications. Some individuals may also wish to transition to lifestyle-based maintenance after significant metabolic improvements.
It is important to understand that tirzepatide does not cure diabetes or obesity—it manages these conditions while actively taken. The medication's effects on glucose regulation and appetite suppression diminish after discontinuation, as the drug has a half-life of approximately five days, meaning it clears from the system within several weeks. There is no official evidence that tirzepatide causes physical dependence or withdrawal symptoms in the traditional sense, but the underlying metabolic conditions will reassert themselves without ongoing pharmacological support.
Before making any decision to stop tirzepatide, patients should carefully evaluate their reasons and understand the potential metabolic consequences. Abrupt discontinuation without a management plan may result in weight regain and deterioration of glycemic control in individuals with diabetes.
Seek immediate medical attention if you experience severe abdominal pain (possible pancreatitis), persistent vomiting leading to dehydration, signs of gallbladder disease, or blood glucose levels persistently above 300 mg/dL with symptoms such as excessive thirst or urination.
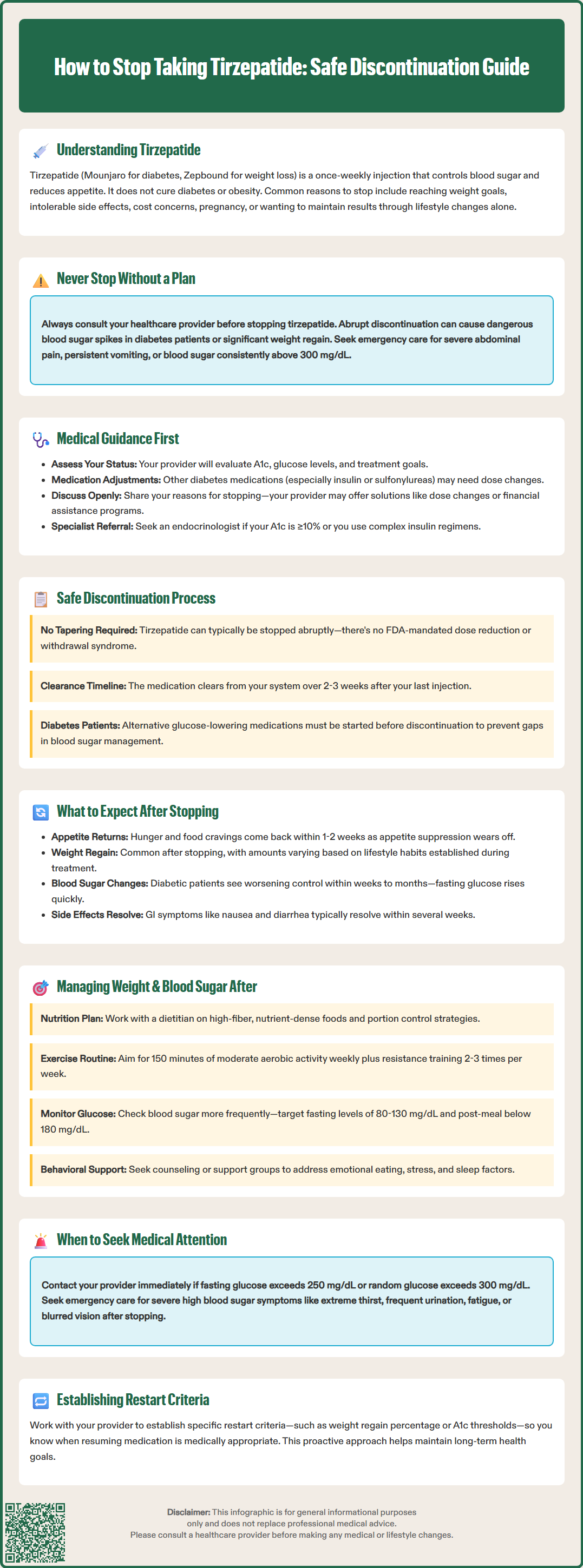
Discontinuing tirzepatide should be discussed with your healthcare provider before stopping this medication, regardless of your reasons. Your physician needs to assess your current metabolic status, review your treatment goals, and develop an individualized discontinuation strategy that protects your health.
During your consultation, your provider will likely evaluate several clinical parameters. For patients with type 2 diabetes, this includes reviewing recent hemoglobin A1c levels, fasting glucose readings, and overall glycemic trends. Your provider will assess whether alternative diabetes medications are necessary to maintain glucose control after tirzepatide cessation. For those using tirzepatide primarily for weight management, discussion will focus on sustainable lifestyle strategies and whether other interventions might be appropriate.
Your healthcare team should also review your complete medication list, as stopping tirzepatide may require adjustments to other therapies. Patients taking insulin or sulfonylureas alongside tirzepatide may have had doses reduced during treatment; these may need recalibration after discontinuation to prevent hyperglycemia. The primary concern after stopping is typically worsening glycemic control rather than hypoglycemia.
Be transparent with your provider about your reasons for wanting to stop. If adverse effects are the primary concern, dose adjustment or symptomatic management strategies might allow continuation. If cost is the barrier, your provider may know of patient assistance programs or alternative medications. If you're stopping due to achieving goals, your provider can help establish realistic expectations and monitoring plans. Documentation of your discontinuation plan in your medical record ensures continuity of care and appropriate follow-up scheduling.
Consider referral to an endocrinologist if you have an A1c ≥10%, experience symptomatic hyperglycemia, or have a complex insulin regimen. Continuous glucose monitoring may be beneficial during the transition period for some patients.
Unlike some medications that require gradual dose reduction, tirzepatide can typically be stopped abruptly without a formal tapering schedule. The FDA prescribing information does not mandate dose reduction before discontinuation, and there is no official evidence of withdrawal syndrome or rebound effects requiring gradual weaning. However, the approach to stopping should still be methodical and individualized.
For most patients, discontinuation involves simply not administering the next scheduled weekly injection. The medication will gradually clear from your system over approximately two to three weeks due to its pharmacokinetic profile. During this clearance period, you may notice progressive return of appetite and gradual changes in satiety signals as the drug's effects on GLP-1 and GIP receptors diminish.
Some healthcare providers may recommend a modified approach for specific patient populations. Individuals who have experienced dramatic weight loss or significant improvement in diabetes control might benefit from a more structured transition period with intensified lifestyle interventions initiated before the final dose. This proactive strategy can help establish new behavioral patterns while medication effects are still partially active.
Patients with type 2 diabetes require particular attention during discontinuation. Your provider may initiate or adjust alternative glucose-lowering medications before stopping tirzepatide, ensuring continuous glycemic management. This might include metformin optimization, addition of SGLT2 inhibitors (particularly beneficial for those with cardiovascular disease, heart failure, or chronic kidney disease), DPP-4 inhibitors, or other agents depending on your individual clinical profile and contraindications. The goal is preventing any gap in diabetes management that could lead to hyperglycemic complications.
Regardless of your specific situation, establish a clear monitoring plan with your healthcare team. This should include scheduled follow-up appointments, home glucose monitoring protocols if diabetic, and specific parameters that would trigger earlier medical contact. Contact your provider if you experience fasting blood glucose persistently above 250 mg/dL, random blood glucose above 300 mg/dL, or symptoms of hyperglycemia such as increased thirst, frequent urination, or unusual fatigue.
After discontinuing tirzepatide, patients should anticipate several physiological changes as the medication's effects wane. Understanding these expected changes helps distinguish normal responses from concerning developments requiring medical attention.
Appetite changes typically occur first and most noticeably. Within one to two weeks of the last injection, most patients experience return of previous hunger patterns and food cravings. The appetite suppression and early satiety that characterized treatment will gradually diminish. Some individuals report that hunger feels more intense initially, though this likely represents return to baseline rather than true rebound hyperphagia. Gastric emptying returns to normal rates, which may manifest as reduced fullness after meals and quicker return of hunger between eating occasions.
Weight regain is common and well-documented in clinical studies. Research from the SURMOUNT-4 trial specifically demonstrated that patients who discontinued tirzepatide regained significant weight compared to those who continued treatment. The rate and extent of weight regain vary considerably among individuals and depend heavily on lifestyle factors, dietary habits, physical activity levels, and underlying metabolic characteristics. Some patients maintain losses better than others, particularly those who have established sustainable behavioral changes during treatment.
For patients with type 2 diabetes, glycemic control may deteriorate after discontinuation if alternative management strategies are inadequate. Fasting glucose levels and postprandial excursions typically increase within weeks. Hemoglobin A1c will rise more gradually over subsequent months. The degree of deterioration depends on baseline diabetes severity, duration of disease, beta-cell function, and effectiveness of replacement therapies.
Gastrointestinal symptoms that troubled some patients during treatment—nausea, occasional vomiting, diarrhea, or constipation—generally resolve as the drug clears from your system, typically over several weeks, though individual experiences vary. Most patients experience no adverse effects from stopping itself; rather, they notice absence of the medication's therapeutic effects.
Seek urgent medical care if you develop severe hyperglycemia symptoms (extreme thirst, frequent urination, fatigue, blurred vision) during the transition period.
Successful long-term outcomes after stopping tirzepatide require proactive management strategies addressing both weight maintenance and glycemic control. The transition period represents a critical window for establishing sustainable health behaviors.
Dietary management becomes paramount after discontinuation. Work with a registered dietitian to develop an individualized eating plan that accounts for your returned appetite and changed satiety signals. Focus on nutrient-dense, high-fiber foods that promote fullness—vegetables, fruits, whole grains, lean proteins, and legumes. Portion control strategies become especially important as the medication's appetite-suppressing effects fade. Consider structured meal timing, mindful eating practices, and environmental modifications that support healthy choices. Adequate protein intake may help preserve lean muscle mass and support satiety, but should be individualized based on your specific health needs, particularly if you have kidney disease.
Physical activity is essential for weight maintenance and glycemic control. The American Diabetes Association recommends at least 150 minutes of moderate-intensity aerobic activity weekly, spread over at least three days, with no more than two consecutive days without activity. Resistance training two to three times weekly helps maintain muscle mass, which supports metabolic rate and insulin sensitivity. If you weren't physically active during tirzepatide treatment, gradually build an exercise routine with guidance from your healthcare provider or exercise physiologist.
For patients with diabetes, intensified glucose monitoring is crucial after discontinuation. Check fasting and postprandial glucose levels as directed by your provider—often more frequently during the initial transition period. Target ranges should align with American Diabetes Association guidelines: fasting glucose 80–130 mg/dL and 1–2 hour postprandial glucose less than 180 mg/dL for most adults. Your provider will schedule hemoglobin A1c testing approximately three months after discontinuation to assess overall glycemic trends.
Behavioral and psychological support can significantly improve outcomes. Consider ongoing counseling, support groups, or digital health programs focused on weight management and diabetes self-management. Address emotional eating patterns, stress management, and sleep hygiene—all factors that influence both weight and glucose control. Some patients benefit from regular accountability check-ins with healthcare providers or health coaches during the critical first six months after discontinuation.
Establish clear criteria for restarting medication. Discuss with your provider specific thresholds—such as regaining a certain percentage of lost weight or hemoglobin A1c rising above target—that would prompt reconsideration of pharmacological therapy. Tirzepatide or alternative medications can be restarted if lifestyle measures prove insufficient, and there is no penalty for resuming treatment when medically appropriate.
No, tirzepatide does not require gradual tapering and can typically be stopped abruptly by simply not administering the next scheduled weekly injection. However, you should always consult your healthcare provider before discontinuing to develop an appropriate monitoring and management plan for the transition period.
Weight regain is common after discontinuing tirzepatide, as clinical studies have demonstrated significant weight increase in patients who stopped treatment. The extent of regain varies among individuals and depends heavily on lifestyle factors including diet, physical activity, and behavioral changes established during treatment.
For patients with type 2 diabetes, glycemic control typically deteriorates after discontinuation if alternative management strategies are not in place. Your healthcare provider may need to initiate or adjust other glucose-lowering medications before stopping tirzepatide to maintain blood sugar control and prevent hyperglycemic complications.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.