LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management. Knowing when to increase tirzepatide requires understanding the medication's titration schedule, monitoring clinical response, and recognizing signs of inadequate dosing. Dose escalation decisions depend on glycemic control, weight loss progress, tolerability, and individualized treatment goals. The FDA-approved schedule increases doses every four weeks, starting from 2.5 mg to maintenance doses of 5 mg, 10 mg, or 15 mg weekly. This article explains the clinical indicators, guidelines, and decision-making process that determine when tirzepatide dose increases are appropriate.
Quick Answer: Tirzepatide dose increases are considered after at least four weeks at the current dose when HbA1c remains above target, weight loss plateaus despite lifestyle adherence, or the current dose is well-tolerated without achieving therapeutic goals.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. For weight management (Zepbound), it's indicated for adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity, in conjunction with diet and exercise.
The FDA-approved titration schedule begins with a starting dose of 2.5 mg administered subcutaneously once weekly. This initial dose serves primarily as a tolerability step rather than a therapeutic dose. After four weeks, the dose is increased to 5 mg weekly, which represents the first maintenance dose for glycemic control. Subsequent dose increases occur at four-week intervals, with recommended maintenance doses of 5 mg, 10 mg, or 15 mg weekly. Intermediate doses of 7.5 mg and 12.5 mg are available as titration steps if needed.
This gradual titration schedule is designed to allow the gastrointestinal system to adapt to tirzepatide's effects on gastric emptying and satiety signaling. The four-week intervals between dose adjustments align with the medication's pharmacokinetic profile, as steady-state concentrations are achieved after approximately four weeks of consistent dosing.
Patients should understand that dose escalation is individualized and not automatic. The decision to increase tirzepatide depends on multiple clinical factors including glycemic response, weight loss progress, tolerability of current dose, and individual treatment goals. Not all patients require or benefit from maximum dosing, and some achieve optimal outcomes at lower maintenance doses.
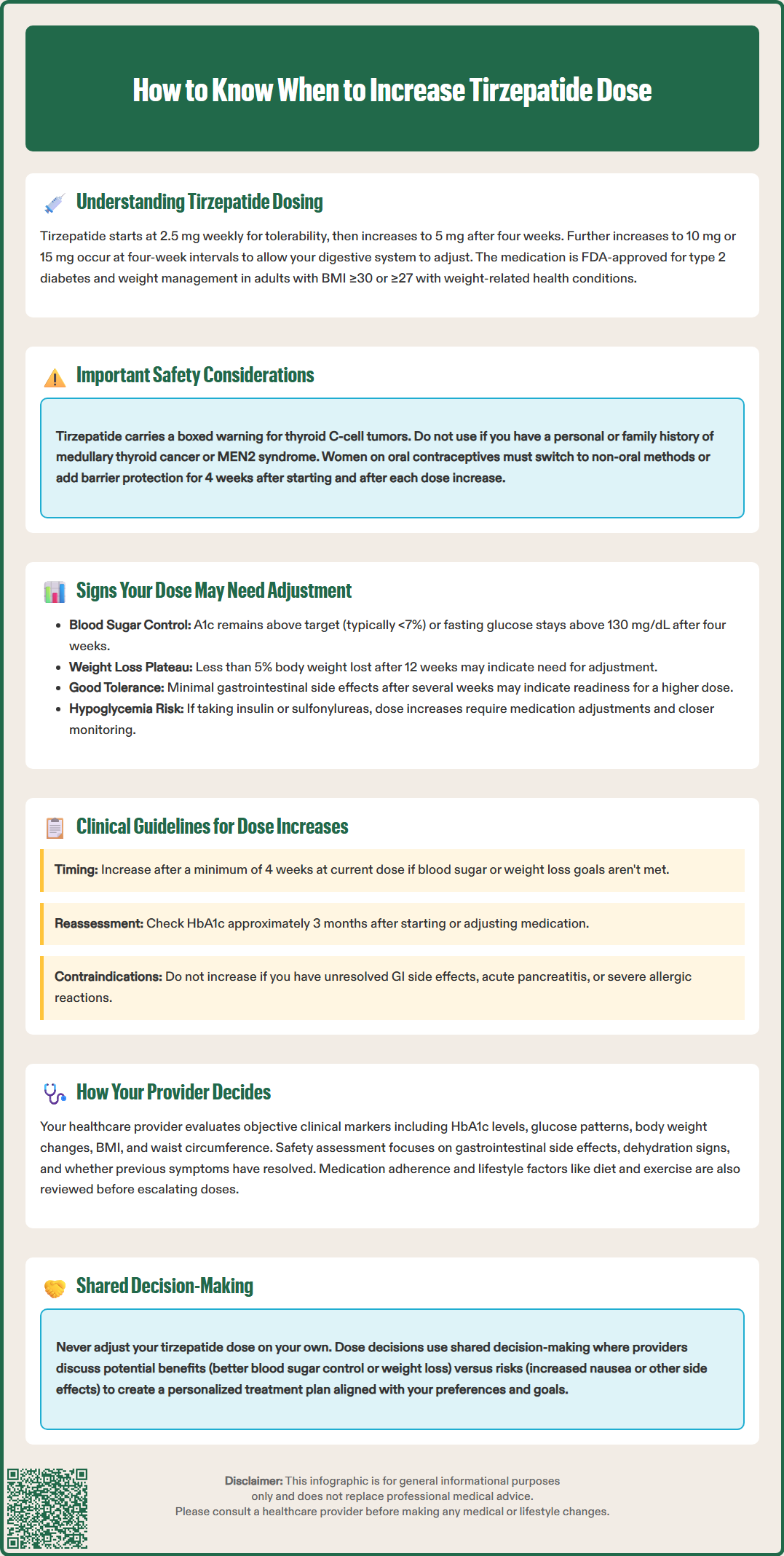
Several clinical indicators suggest that your current tirzepatide dose may be insufficient for achieving your therapeutic goals. The most objective measure is inadequate glycemic control in patients with type 2 diabetes. If your hemoglobin A1c (HbA1c) remains above your individualized target—typically less than 7% for most adults, though targets vary based on age, comorbidities, and hypoglycemia risk—after at least four weeks at your current dose, a dose increase may be warranted. Similarly, fasting blood glucose levels consistently above 130 mg/dL or postprandial glucose readings exceeding 180 mg/dL may indicate suboptimal dosing.
For patients using tirzepatide for weight management, a plateau in weight loss despite adherence to lifestyle modifications can signal the need for dose adjustment. According to obesity treatment guidelines, inadequate response is generally defined as less than 5% body weight reduction after 12 weeks at a therapeutic dose, though this is not a specific FDA requirement for tirzepatide. Weight loss patterns vary considerably among individuals, and temporary plateaus are normal physiological responses that don't always necessitate dose changes.
Tolerability is equally important when considering dose escalation. If you've experienced minimal or no gastrointestinal side effects—such as nausea, vomiting, diarrhea, or decreased appetite—at your current dose for several weeks, this may indicate good tolerance that could support moving to a higher dose. Conversely, persistent or severe adverse effects suggest your current dose may already be at your individual tolerance threshold.
Patients taking insulin or sulfonylureas should be aware that increasing tirzepatide may enhance the risk of hypoglycemia. Your healthcare provider may need to reduce doses of these medications when escalating tirzepatide and will likely recommend more frequent blood glucose monitoring.
Certain symptoms should prompt immediate medical attention before any dose increase, including severe abdominal pain (with or without vomiting), persistent nausea/vomiting leading to dehydration, symptoms of gallbladder disease, allergic reactions, or any unusual thyroid swelling or mass.
It's essential to recognize that the absence of side effects doesn't automatically mean your dose is too low. Tirzepatide's therapeutic effects operate independently of subjective symptoms, and many patients achieve excellent outcomes without experiencing significant adverse effects. Never adjust your dose without consulting your healthcare provider, as self-directed changes can compromise safety and treatment efficacy.
Clinical practice guidelines from the American Diabetes Association (ADA) and American Association of Clinical Endocrinology (AACE) provide evidence-based frameworks for tirzepatide dose escalation. The primary criterion for dose increase is inadequate achievement of individualized glycemic targets after a minimum of four weeks at the current dose. This timeframe allows sufficient evaluation of the medication's full effect at each dose level, as glycemic improvements continue to develop over several weeks.
For type 2 diabetes management, dose escalation is appropriate when HbA1c remains above target despite adherence to the current regimen. The ADA recommends reassessing HbA1c approximately three months after initiating or adjusting glucose-lowering therapy, though clinical judgment may support earlier assessment in certain circumstances. Patients with baseline HbA1c significantly above target (e.g., >9%) may benefit from more aggressive titration, while those closer to goal may require more conservative approaches.
In chronic weight management, the FDA label and clinical guidelines support dose increases when weight loss is insufficient relative to treatment goals. The typical approach involves escalating the dose every four weeks until the patient achieves adequate weight loss, experiences dose-limiting side effects, or reaches the maximum dose of 15 mg weekly. Clinical trials demonstrated that higher doses generally produced greater weight reduction, though individual responses vary substantially.
Situations where dose escalation should be deferred include: persistent gastrointestinal symptoms that haven't resolved, history of severe hypersensitivity reactions, acute pancreatitis during treatment, or patient preference to remain at current dose. Tirzepatide is contraindicated in patients with a personal or family history of MTC or MEN2, and in those with serious hypersensitivity to the medication.
For patients taking insulin or sulfonylureas, dose adjustments of these medications are typically needed when increasing tirzepatide to reduce hypoglycemia risk. Women using oral contraceptives should use a non-oral method or add a barrier method for 4 weeks after each dose increase due to potential reduced contraceptive efficacy.
Regarding perioperative management, current multi-society guidance (2024) recommends individualized assessment rather than routine discontinuation. Patients should coordinate with their surgical and anesthesia teams, as most can continue GLP-1 receptor agonists during the perioperative period. Healthcare providers must balance the potential benefits of higher doses against individual patient factors, comorbidities, and treatment priorities when determining the optimal timing for dose adjustment.
Healthcare providers employ a comprehensive clinical assessment process when determining whether to increase tirzepatide dosing. The decision integrates objective clinical data, patient-reported outcomes, safety considerations, and individualized treatment goals. This multifaceted approach ensures that dose adjustments are both medically appropriate and aligned with patient preferences.
The evaluation begins with reviewing objective clinical markers. For diabetes management, providers assess HbA1c trends, fasting and postprandial glucose patterns from self-monitoring or continuous glucose monitoring data, and time-in-range metrics when available. They compare these values against your individualized glycemic targets, which may differ from standard goals based on factors such as age, diabetes duration, cardiovascular disease risk, hypoglycemia history, and life expectancy. For weight management, providers track body weight changes, body mass index (BMI), waist circumference, and percentage of total body weight lost since treatment initiation.
Safety assessment is paramount in dose escalation decisions. Your provider will review your experience with the current dose, specifically inquiring about gastrointestinal symptoms (nausea, vomiting, diarrhea, constipation, abdominal pain), changes in appetite, signs of dehydration, and any other adverse effects. They'll evaluate whether previous side effects have resolved or persist, as ongoing symptoms may contraindicate further dose increases. Laboratory monitoring may include renal function tests, lipase levels if pancreatitis is suspected, and assessment of volume status.
Before escalating doses, providers will screen for contraindications including personal or family history of MTC or MEN2. For women of childbearing potential, pregnancy status is assessed, as tirzepatide for weight management is not recommended during pregnancy. Patients using oral contraceptives will be counseled on using back-up or non-oral contraception for 4 weeks after each dose increase.
For patients taking insulin or sulfonylureas, providers will often proactively reduce these medications when increasing tirzepatide to minimize hypoglycemia risk, and will recommend more frequent glucose monitoring during the transition.
Providers also consider medication adherence, lifestyle factors, and psychosocial elements. Consistent weekly administration is essential for accurate dose assessment, and irregular adherence may necessitate addressing barriers before escalating therapy. Your dietary patterns, physical activity level, and weight management strategies are reviewed, as lifestyle optimization can enhance medication efficacy and may reduce the need for higher doses.
The decision-making process incorporates shared decision-making principles, where your provider discusses the potential benefits of dose escalation—such as improved glycemic control or enhanced weight loss—against possible risks, including increased gastrointestinal side effects. They'll explain the expected timeline for seeing results at the higher dose and establish clear criteria for assessing response. This collaborative approach ensures that dose adjustments align with your treatment priorities, tolerance for side effects, and overall health goals, creating a personalized titration strategy that optimizes both efficacy and safety throughout your treatment journey.
The FDA-approved titration schedule recommends waiting at least four weeks at each dose level before increasing, as this allows sufficient time to assess the medication's full therapeutic effect and tolerability at that dose.
Signs may include HbA1c remaining above your individualized target, fasting glucose consistently above 130 mg/dL, or inadequate weight loss after 12 weeks at a therapeutic dose despite adherence to lifestyle modifications. However, only your healthcare provider can determine if a dose increase is appropriate based on comprehensive clinical assessment.
No, never adjust your tirzepatide dose without consulting your healthcare provider. Self-directed dose changes can compromise safety and treatment efficacy, and your provider needs to assess multiple clinical factors, screen for contraindications, and potentially adjust other medications before increasing your dose.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.