LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
How to track progress on tirzepatide involves monitoring multiple clinical parameters to assess both therapeutic benefits and tolerability. Tirzepatide, a dual GIP/GLP-1 receptor agonist approved for type 2 diabetes (Mounjaro) and chronic weight management (Zepbound), requires systematic tracking of weight, glycemic control, metabolic markers, and side effects. Establishing individualized treatment goals at baseline—whether targeting hemoglobin A1c reduction, sustained weight loss, or improvement in obesity-related comorbidities—creates a framework for meaningful progress assessment. Regular documentation using standardized measurement protocols enables patients and clinicians to optimize dosing, manage adverse effects, and make informed decisions about treatment continuation.
Quick Answer: Tracking progress on tirzepatide requires monitoring weight, hemoglobin A1c, blood glucose patterns, cardiovascular markers, and gastrointestinal tolerability at regular intervals.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound) in adults. This once-weekly subcutaneous injection works through multiple mechanisms: enhancing insulin secretion in response to elevated glucose levels, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways.
Important safety information: Tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Tirzepatide is not indicated for use in patients with type 1 diabetes.
Establishing clear, individualized treatment goals before initiating tirzepatide is essential for meaningful progress assessment. For patients with type 2 diabetes, primary objectives typically include achieving target hemoglobin A1c levels (generally below 7% for most adults, though individualized based on patient factors), reducing fasting and postprandial glucose excursions, and potentially decreasing reliance on other glucose-lowering medications. The American Diabetes Association emphasizes personalized glycemic targets that balance efficacy with hypoglycemia risk and patient preferences.
For weight management, Zepbound is indicated for adults with either a BMI ≥30 kg/m² (obesity) or BMI ≥27 kg/m² (overweight) with at least one weight-related comorbidity. Realistic expectations involve gradual, sustained weight reduction rather than rapid loss. Clinical trials (SURMOUNT-1) demonstrated significant weight reductions over 72 weeks, though individual responses vary considerably. Secondary goals often include improvements in obesity-related comorbidities such as hypertension, dyslipidemia, obstructive sleep apnea, and metabolic dysfunction-associated steatotic liver disease (MASLD). Documenting baseline measurements across multiple domains creates a comprehensive framework for evaluating treatment effectiveness and guides clinical decision-making regarding dose adjustments or continuation of therapy.
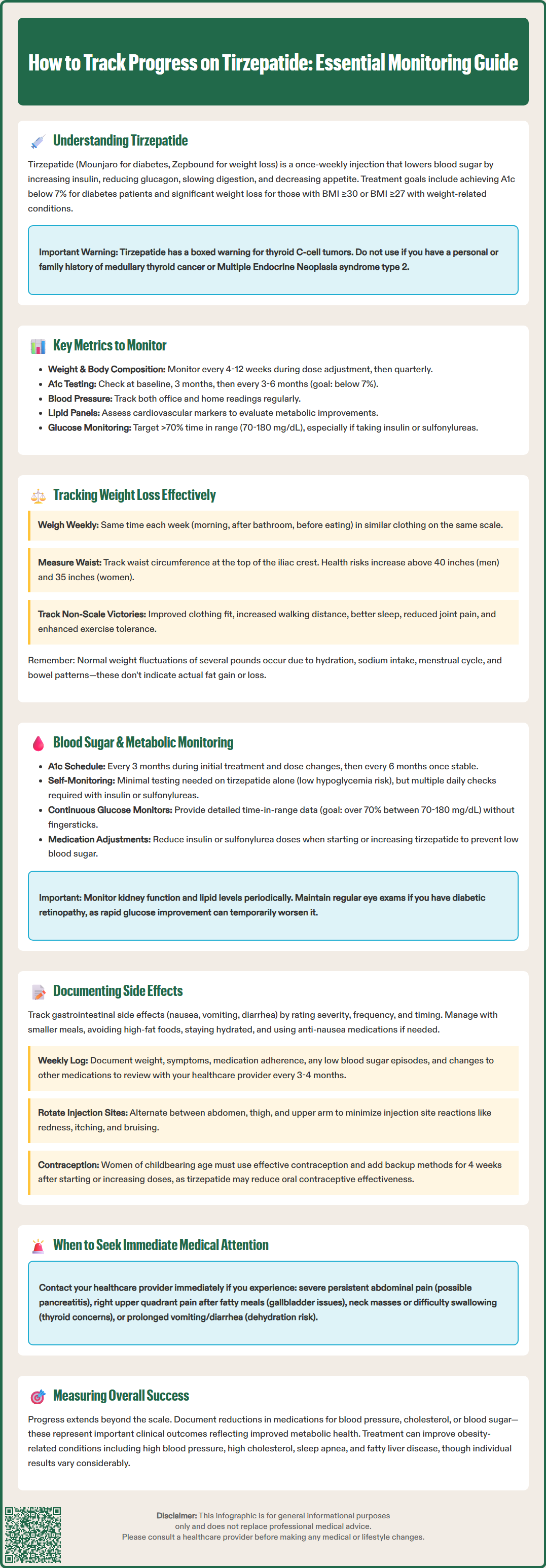
Comprehensive tirzepatide monitoring requires tracking multiple physiological parameters that reflect both therapeutic benefits and potential adverse effects. Weight and body composition represent primary outcome measures, but should be assessed alongside metabolic markers for a complete clinical picture. Regular measurement intervals—typically every 4-12 weeks during titration and quarterly thereafter—allow detection of meaningful trends while avoiding excessive focus on normal day-to-day fluctuations.
Glycemic control parameters are fundamental for patients with diabetes. Hemoglobin A1c provides a 2-3 month average of glucose control and should be measured at baseline, after 3 months of therapy, and then every 3-6 months once stable. Self-monitoring of blood glucose (SMBG) frequency depends on individual circumstances, diabetes type, and concurrent medications—particularly insulin or sulfonylureas that increase hypoglycemia risk. Continuous glucose monitoring (CGM) systems offer detailed glycemic patterns including time-in-range metrics (target: >70% time within 70-180 mg/dL) and time-below-range metrics (target: <4% below 70 mg/dL and <1% below 54 mg/dL), which increasingly inform treatment optimization.
Cardiovascular and metabolic markers warrant regular assessment given tirzepatide's effects on multiple risk factors. Blood pressure monitoring—both in-office and home measurements—tracks improvements in hypertension. Lipid panels (total cholesterol, LDL-C, HDL-C, triglycerides) typically show favorable changes with weight loss. Liver function tests are not routinely required for tirzepatide monitoring unless clinically indicated or abnormal at baseline.
Gastrointestinal tolerability significantly impacts treatment adherence. Systematic documentation of nausea, vomiting, diarrhea, constipation, and abdominal discomfort—including severity, timing relative to injections, and impact on daily functioning—guides dose titration decisions. Patients should monitor hydration status, especially with significant GI symptoms, as dehydration may increase risk of acute kidney injury. Patients should also monitor for signs of more serious complications including pancreatitis (severe persistent abdominal pain radiating to the back) or gallbladder disease, which require immediate medical evaluation. Additionally, patients should report any symptoms of thyroid tumors such as neck mass, dysphagia, hoarseness, or persistent dyspnea.
Accurate weight tracking requires standardized measurement protocols to minimize variability and identify genuine trends. Patients should weigh themselves at the same time of day (preferably morning after voiding, before eating), wearing similar clothing, on the same calibrated scale. Weekly weighing provides sufficient data for trend analysis without promoting obsessive monitoring. Recording weights in a dedicated log, smartphone app, or patient portal facilitates visualization of progress and sharing with healthcare providers. Normal fluctuations of several pounds due to hydration status, dietary sodium, menstrual cycle, and bowel patterns should be expected and not cause undue concern.
Beyond scale weight, body composition assessment offers valuable insights into fat mass versus lean tissue changes. While dual-energy X-ray absorptiometry (DEXA) provides detailed body composition data, it may not be practical or accessible for routine monitoring. More practical alternatives include bioelectrical impedance scales (recognizing their limitations and need for consistent measurement conditions) and circumference measurements. Waist circumference measured at the iliac crest correlates with visceral adiposity and cardiometabolic risk—with reductions often accompanying clinically significant weight loss. The CDC recommends measuring at the top of the iliac crest, with risk thresholds in the US generally considered as >40 inches (102 cm) for men and >35 inches (88 cm) for women, though these may vary by ethnicity. Some patients find progress photos (standardized lighting, clothing, and positioning) helpful for visualizing changes not captured by numbers alone.
Non-scale victories deserve equal documentation as they reflect meaningful health improvements and support sustained motivation. These include clothing fit changes, improved physical function (walking distance, stair climbing ability, exercise tolerance), enhanced sleep quality, reduced joint pain, and better mobility. Standardized questionnaires like the Impact of Weight on Quality of Life-Lite (IWQOL-Lite) quantify these subjective improvements. Patients should also note changes in medication requirements—reductions in antihypertensive, lipid-lowering, or glucose-lowering medications represent important clinical outcomes that may not be immediately apparent from weight alone but reflect improved metabolic health.
For patients with type 2 diabetes, systematic glucose monitoring provides essential feedback on tirzepatide's glycemic efficacy and guides treatment adjustments. Hemoglobin A1c testing every 3 months during initial therapy and dose titration allows assessment of average glucose control, with testing intervals potentially extending to every 6 months once stable target levels are achieved. The American Diabetes Association recommends A1c targets generally below 7% for most non-pregnant adults, though individualized goals may be less stringent (below 8%) for patients with limited life expectancy, extensive comorbidities, or high hypoglycemia risk, and more stringent (below 6.5%) for selected patients early in disease course without significant hypoglycemia or treatment burden.
Self-monitoring of blood glucose frequency should be individualized based on diabetes regimen complexity and hypoglycemia risk. Patients on tirzepatide monotherapy have minimal hypoglycemia risk and may require only periodic fasting and postprandial checks to confirm adequate control. However, those using concurrent insulin or sulfonylureas need more frequent monitoring—potentially multiple daily checks—particularly during dose titration when medication adjustments are common. Dose reductions of insulin or sulfonylureas should be considered when initiating or escalating tirzepatide to reduce hypoglycemia risk. Fasting glucose values typically range 80-130 mg/dL as a target, with postprandial values below 180 mg/dL. Patients should document glucose readings with contextual information (timing relative to meals and injections, unusual food intake, illness, stress) to identify patterns requiring intervention.
Continuous glucose monitoring systems increasingly provide comprehensive glycemic data without fingerstick requirements. CGM metrics include time-in-range (target 70-180 mg/dL for >70% of time), time-below-range (target <4% below 70 mg/dL and <1% below 54 mg/dL), glucose variability, and ambulatory glucose profile patterns. These detailed data help optimize tirzepatide dosing and timing of concurrent medications. Beyond glucose, periodic monitoring of kidney function (serum creatinine, estimated glomerular filtration rate) and lipid profiles documents improvements in cardiovascular risk factors that commonly accompany weight loss and improved glycemic control, though there is no official requirement for more frequent testing than standard diabetes care protocols unless clinically indicated. Patients with diabetic retinopathy should ensure regular eye examinations, as rapid improvement in glucose control may temporarily worsen retinopathy in some cases.
Systematic adverse effect documentation enables early identification of tolerability issues and guides management strategies that support treatment continuation. Gastrointestinal symptoms—nausea, vomiting, diarrhea, constipation, abdominal pain, and decreased appetite—represent the most common tirzepatide side effects, typically emerging after dose initiation or escalation and often improving within days to weeks. Patients should rate symptom severity (mild, moderate, severe), frequency, duration, and functional impact using a consistent scale. Noting temporal relationships to injection timing, meal patterns, and specific foods helps identify modifiable triggers. Dietary modifications (smaller, more frequent meals; avoiding high-fat foods; adequate hydration) and anti-nausea medications may provide relief, while persistent severe symptoms may warrant dose reduction or extended time at current dose before further titration.
Patients should monitor for signs of dehydration and seek medical attention for prolonged vomiting or diarrhea, as these may increase risk of acute kidney injury. Tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis. Persistent severe GI symptoms should prompt medical evaluation.
Injection site reactions—redness, itching, bruising, or discomfort—should be documented with location, size, and duration. Rotating injection sites (abdomen, thigh, upper arm) and proper technique minimize these reactions. More concerning symptoms requiring immediate medical evaluation include signs of pancreatitis (severe persistent abdominal pain radiating to the back, often with nausea and vomiting), gallbladder disease (right upper quadrant pain, particularly after fatty meals), thyroid tumors (neck mass, difficulty swallowing, hoarseness, shortness of breath), or allergic reactions (rash, itching, difficulty breathing). While rare, these serious adverse effects necessitate treatment discontinuation and urgent assessment.
Women of childbearing potential should use effective contraception while taking tirzepatide. Due to potential decreased exposure to oral contraceptives, alternative or backup contraception methods are recommended for 4 weeks after tirzepatide initiation and after each dose increase. Tirzepatide should be discontinued if pregnancy occurs.
Tracking overall treatment response involves documenting both benefits and burdens. A simple weekly log capturing weight, notable symptoms, medication adherence, and general well-being creates a comprehensive record for clinical discussions. Patients should note any hypoglycemic episodes (symptoms, confirmed glucose values, precipitating factors, treatment required) particularly when using concurrent insulin or sulfonylureas. Changes in other medications—dose reductions in antihypertensives, statins, or diabetes medications—represent important positive outcomes. Regular review of this documentation with healthcare providers, typically every 3-4 months or more frequently during titration, ensures appropriate treatment optimization, addresses emerging concerns, and reinforces realistic expectations about the gradual nature of metabolic improvements with tirzepatide therapy.
Weekly weighing at the same time of day (preferably morning after voiding, before eating) provides sufficient data for trend analysis without promoting obsessive monitoring. Normal fluctuations of several pounds due to hydration, dietary sodium, and other factors should be expected.
Hemoglobin A1c should be measured every 3 months during initial therapy and dose titration, then every 3-6 months once stable. Periodic monitoring of kidney function and lipid profiles documents cardiovascular risk factor improvements, though frequency follows standard diabetes care protocols unless clinically indicated.
Seek immediate medical evaluation for severe persistent abdominal pain radiating to the back (possible pancreatitis), right upper quadrant pain after fatty meals (gallbladder disease), neck mass or difficulty swallowing (thyroid concerns), prolonged vomiting or diarrhea (dehydration risk), or allergic reactions. Persistent severe gastrointestinal symptoms also warrant medical assessment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.