LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) is an FDA-approved dual GIP/GLP-1 receptor agonist that significantly reduces appetite and alters eating patterns. Effective meal logging tips for tirzepatide users help ensure adequate nutrition despite appetite suppression, identify food-symptom relationships, and support medication tolerance. Tracking protein, fiber, hydration, and micronutrients becomes essential as reduced food intake may lead to nutritional gaps or irregular eating patterns. This guide provides practical strategies for meal logging that accommodate tirzepatide's pharmacological effects while supporting metabolic health and treatment goals.
Quick Answer: Meal logging on tirzepatide helps ensure adequate nutrition during appetite suppression by tracking protein intake, fiber consumption, hydration, and micronutrients while identifying food-symptom relationships.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). Its mechanism of action includes slowing gastric emptying, enhancing insulin secretion, suppressing glucagon release, and reducing appetite through central nervous system pathways. These pharmacological effects significantly alter eating patterns, making meal logging a helpful tool for supporting treatment.
Patients taking tirzepatide commonly experience appetite suppression and early satiety, which can lead to reduced food intake. Without systematic meal tracking, patients may find it challenging to meet nutritional requirements or may develop irregular eating patterns that could affect their metabolic health. This is particularly important during dose escalation phases when appetite changes are often most pronounced.
Meal logging provides objective data that helps patients and healthcare providers identify eating patterns that may need adjustment. Potential concerns include inadequate protein intake, reduced consumption of fiber-rich foods that may contribute to constipation (a known side effect of tirzepatide), and significant caloric restriction. The American Diabetes Association emphasizes the importance of individualized nutrition therapy for patients on glucose-lowering medications, and meal logging can support this personalized approach.
Tracking food intake can also help identify relationships between specific foods or eating patterns and gastrointestinal symptoms such as nausea, vomiting, or diarrhea. This information allows for dietary modifications that may improve medication tolerance. Patients taking tirzepatide with insulin or sulfonylureas should be particularly vigilant about tracking meals, as reduced food intake increases hypoglycemia risk and may require medication adjustments.
Patients should seek immediate medical attention for persistent vomiting or inability to keep fluids down for more than 24 hours, severe abdominal pain (especially if radiating to the back, which could indicate pancreatitis), or right upper quadrant pain with fever or yellowing of the skin (possible gallbladder issues)—all rare but serious potential complications.
Patients using tirzepatide should prioritize tracking specific macronutrients and micronutrients that may be affected by reduced appetite and food intake. Protein intake represents a critical nutrient to monitor, as inadequate protein consumption during weight loss may affect lean muscle mass. While individual needs vary, general recommendations include at least 0.8 g/kg of body weight daily for most adults, with consideration for higher amounts (1.0-1.2 g/kg/day) during active weight loss. Older adults or those engaging in regular resistance training may benefit from higher protein intake (1.2-1.5 g/kg/day). A registered dietitian can help determine personalized protein targets based on individual factors.
Fiber intake requires careful attention, as tirzepatide's effect on gastric motility can increase the risk of constipation. According to FDA prescribing information, constipation occurs in approximately 17-21% of patients taking Zepbound (depending on dose) and 12-17% of patients taking Mounjaro. Tracking fiber helps ensure adequate intake from vegetables, fruits, whole grains, and legumes. The USDA Dietary Guidelines recommend about 14 grams of fiber per 1,000 calories consumed, with specific targets based on age and sex. Patients should increase fiber gradually to avoid exacerbating gastrointestinal symptoms during medication adjustment.
Micronutrient tracking should focus on nutrients that may be consumed in lower amounts during periods of reduced intake: vitamin B12, vitamin D, calcium, iron, and folate. Patients with significantly reduced caloric intake may benefit from discussing supplementation with their healthcare provider. Vitamin B12 deserves particular attention, as both metformin (often co-prescribed with tirzepatide) and reduced animal product intake can affect B12 status. The American Diabetes Association recommends periodic B12 assessment for patients on long-term metformin therapy.
Hydration monitoring is equally important, as tirzepatide-associated nausea and reduced fluid intake can lead to dehydration. Hydration needs are individualized based on age, body size, activity level, climate, and medical conditions. While the general recommendation of about 8 cups (64 ounces) daily works for many adults, patients should discuss specific targets with their healthcare provider, particularly if they have kidney disease, heart failure, or are taking SGLT2 inhibitors or diuretics. Adequate hydration also helps mitigate constipation during treatment.
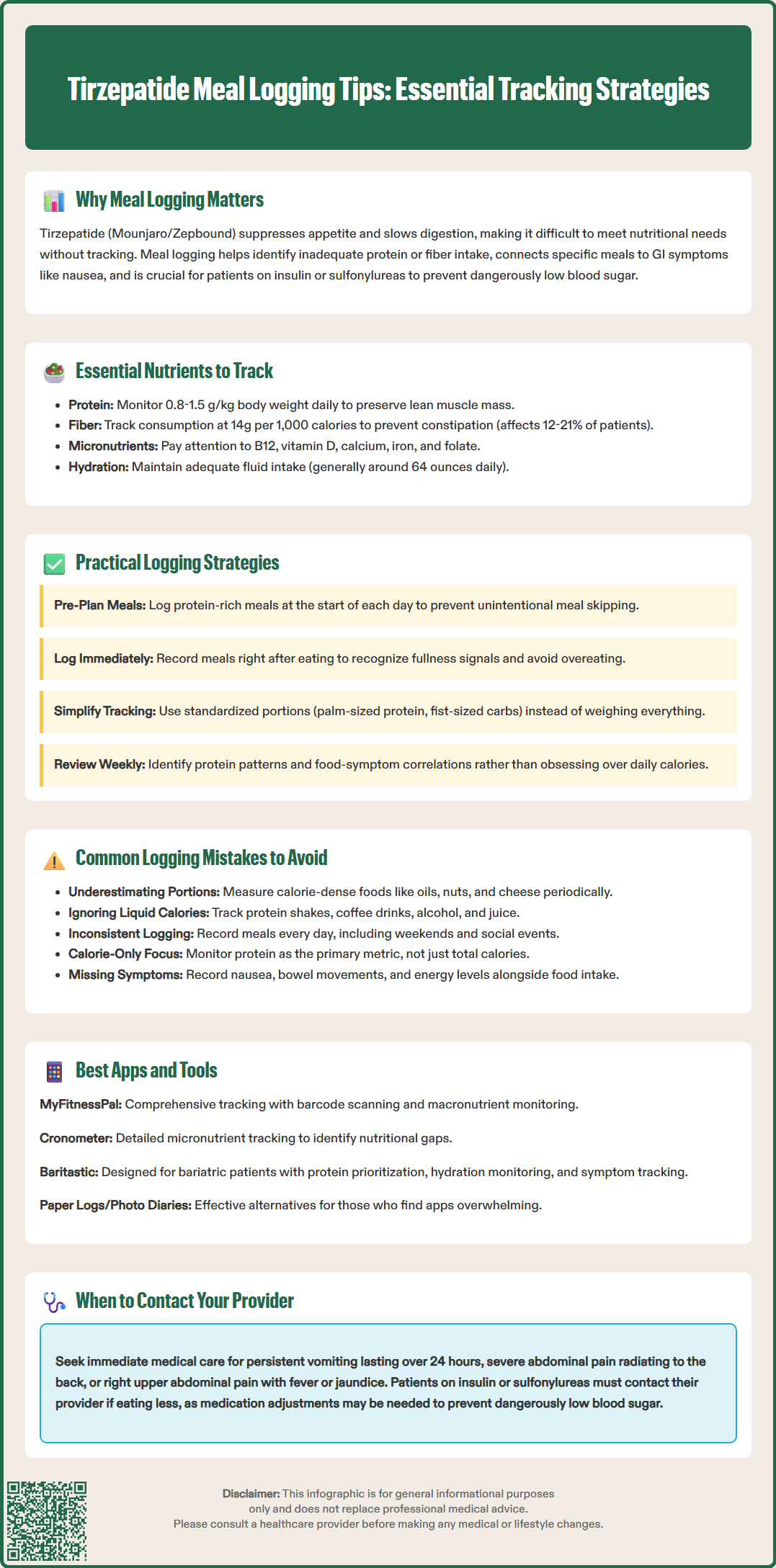
Successful meal logging on tirzepatide requires strategies that accommodate the medication's appetite-suppressing effects and the practical realities of daily life. Pre-planning meals represents an effective approach, as patients often experience minimal hunger and may skip meals unintentionally. Planning protein-rich meals and snacks in advance helps ensure adequate nutrition even when appetite is diminished. Many patients find success preparing a weekly meal template that meets their nutritional targets, then logging planned meals at the start of each day rather than retrospectively.
Real-time logging immediately after eating improves accuracy and helps patients recognize satiety signals before overeating. Tirzepatide's delayed gastric emptying means fullness sensations may occur suddenly; logging in real-time creates awareness of portion sizes that promote comfort. Following FDA label recommendations, patients should consider smaller, lower-fat meals, especially during dose escalation or when experiencing gastrointestinal symptoms. Photographing meals before eating provides visual records that complement numerical data and help identify patterns in food choices.
Simplified tracking methods work better than complex systems for long-term adherence. Rather than weighing every ingredient, patients can use standardized portions (palm-sized protein servings, fist-sized carbohydrate portions) and focus on consistency. For patients experiencing significant nausea, tracking "eating windows" and tolerated foods takes priority over precise calorie counts during symptom management phases.
Weekly review sessions allow patients to analyze trends rather than focusing on daily variations. Reviewing weekly protein averages, identifying days with inadequate intake, and noting correlations between food choices and gastrointestinal symptoms provides actionable insights. Patients taking insulin or sulfonylureas should monitor blood glucose closely and contact their healthcare provider if reduced food intake occurs, as medication adjustments may be needed to prevent hypoglycemia.
Patients should share their meal logs with their healthcare provider at follow-up appointments, particularly during dose escalation periods when eating patterns typically change most dramatically. Those struggling with meal planning or nutritional adequacy should consider requesting a referral to a registered dietitian nutritionist (RDN) for personalized guidance.
Several systematic errors undermine the effectiveness of meal logging for tirzepatide users. Underestimating portion sizes represents a prevalent mistake, particularly for calorie-dense foods like oils, nuts, and cheese. Research shows that individuals frequently underestimate portions without measurement tools. While obsessive weighing isn't necessary long-term, patients should calibrate their portion estimation by measuring foods periodically, especially during the first month of logging.
Neglecting liquid calories creates significant tracking gaps. Patients may meticulously log solid foods while overlooking protein shakes, coffee beverages, alcohol, or juice. These liquids can contribute substantial calories without triggering the same satiety signals as solid foods. On tirzepatide, where appetite suppression already reduces intake, untracked liquid calories may displace nutrient-dense solid foods. Alcohol deserves special attention, as it contributes empty calories and may increase hypoglycemia risk for patients taking certain diabetes medications.
Inconsistent logging during weekends or social events produces incomplete data that obscures true eating patterns. Many patients maintain detailed logs Monday through Friday but abandon tracking on weekends, when eating patterns often differ substantially. This selective logging prevents identification of patterns contributing to suboptimal outcomes. Patients should commit to logging all days or, if that proves unsustainable, consistently track the same days each week to enable meaningful week-to-week comparisons.
Focusing exclusively on calories while ignoring macronutrient distribution represents a critical error for tirzepatide users. A 1,200-calorie day consisting primarily of carbohydrates differs dramatically from one emphasizing protein and healthy fats, particularly regarding satiety, muscle preservation, and glycemic control. Patients should track protein grams as a primary metric, ensuring adequate intake before concerning themselves with total caloric targets.
Skipping meals or excessive restriction can worsen gastrointestinal symptoms and lead to glycemic variability. Regular, smaller meals are often better tolerated than infrequent larger ones. Additionally, failing to log symptoms alongside foods—such as nausea severity, bowel movements, or energy levels—eliminates valuable data for optimizing dietary tolerance during tirzepatide therapy.
Several digital platforms offer features beneficial for tirzepatide users, though no app specifically targets GLP-1 receptor agonist patients. MyFitnessPal provides a comprehensive food database with barcode scanning capability and detailed macronutrient tracking. Its free version offers sufficient functionality for most users, including protein tracking and meal timing records. The premium version adds meal planning features and deeper nutritional analysis that may benefit patients requiring detailed micronutrient monitoring.
Cronometer excels at micronutrient tracking, making it suitable for patients concerned about nutritional adequacy during periods of reduced intake. It provides detailed reports on vitamin and mineral intake relative to recommended daily allowances, helping identify potential gaps. The interface requires slightly more effort than simpler apps, but the comprehensive nutritional data may be valuable for patients working closely with registered dietitians.
Baritastic was designed for bariatric surgery patients but translates well to tirzepatide users facing similar challenges: reduced appetite, protein prioritization, and hydration monitoring. It includes medication reminders, symptom tracking, and progress photos—features that support comprehensive self-monitoring beyond food intake alone. The app's focus on protein-first eating aligns with clinical recommendations for patients experiencing medication-induced appetite suppression.
Simple paper logs or spreadsheets remain viable alternatives for patients who find apps overwhelming or prefer tangible records. A basic template tracking meal times, protein grams, total calories, fluid ounces, and daily symptoms provides sufficient data for clinical decision-making. Some patients prefer photographing meals and maintaining a visual food diary, particularly during periods of significant nausea when detailed logging feels burdensome.
Regardless of the tool selected, consistency matters more than sophistication. Patients should choose a system they'll use regularly, as this allows pattern identification and habit formation. It's important to note that consumer health apps are typically not HIPAA-covered entities; patients should review privacy settings and data-sharing policies. The examples provided are not specific endorsements—patients should select any tool they can use consistently. Healthcare providers should review logs regularly, providing feedback that helps patients interpret their data in the context of their diabetes management or weight loss goals.
Protein intake (0.8-1.5 g/kg/day), fiber (approximately 14 g per 1,000 calories), hydration, and micronutrients including vitamin B12, vitamin D, calcium, iron, and folate are most important to track during tirzepatide treatment to ensure nutritional adequacy despite reduced appetite.
Real-time logging immediately after eating improves accuracy and helps recognize satiety signals before overeating, as tirzepatide's delayed gastric emptying can cause sudden fullness. Pre-planning meals at the start of each day also helps ensure adequate nutrition when appetite is diminished.
MyFitnessPal offers comprehensive macronutrient tracking, Cronometer excels at micronutrient monitoring, and Baritastic includes protein prioritization with symptom tracking. Consistency matters more than app sophistication—choose any tool you'll use regularly and share logs with your healthcare provider.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.