LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Many patients wonder whether tirzepatide is a stimulant medication, particularly given its effects on appetite and weight loss. Tirzepatide is not a stimulant. It is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes (Mounjaro) and chronic weight management (Zepbound). Unlike stimulants such as amphetamines, tirzepatide does not act on dopaminergic or noradrenergic pathways to increase alertness or cardiovascular stimulation. Instead, it works through incretin-based mechanisms that regulate glucose homeostasis and appetite through physiologic pathways.
Quick Answer: Tirzepatide is not a stimulant; it is a dual GIP and GLP-1 receptor agonist that works through incretin-based mechanisms rather than central nervous system stimulation.
Tirzepatide is not a stimulant. It is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand name Mounjaro) and chronic weight management in adults with obesity or overweight with weight-related comorbidities (under the brand name Zepbound). Unlike stimulant medications such as amphetamines or methylphenidate, tirzepatide does not act on the central nervous system's dopaminergic or noradrenergic pathways to increase alertness or blood pressure.
Tirzepatide works through a dual incretin mechanism. It activates both GIP and GLP-1 receptors, which are naturally occurring hormones involved in glucose homeostasis and appetite regulation. When administered subcutaneously once weekly, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. These actions collectively improve glycemic control in patients with type 2 diabetes.
Additionally, tirzepatide acts on receptors in the hypothalamus and other brain regions involved in appetite regulation, leading to reduced food intake and increased satiety. This mechanism contributes to significant weight loss observed in clinical trials. The medication does not produce the euphoria, dependence potential, or cardiovascular stimulation characteristic of true stimulant drugs. Tirzepatide is administered as a subcutaneous injection and is available in multiple doses (2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, and 15 mg). The 2.5 mg dose is a starter dose intended for treatment initiation and should be increased after 4 weeks as tolerated, as it is not intended for long-term glycemic control.
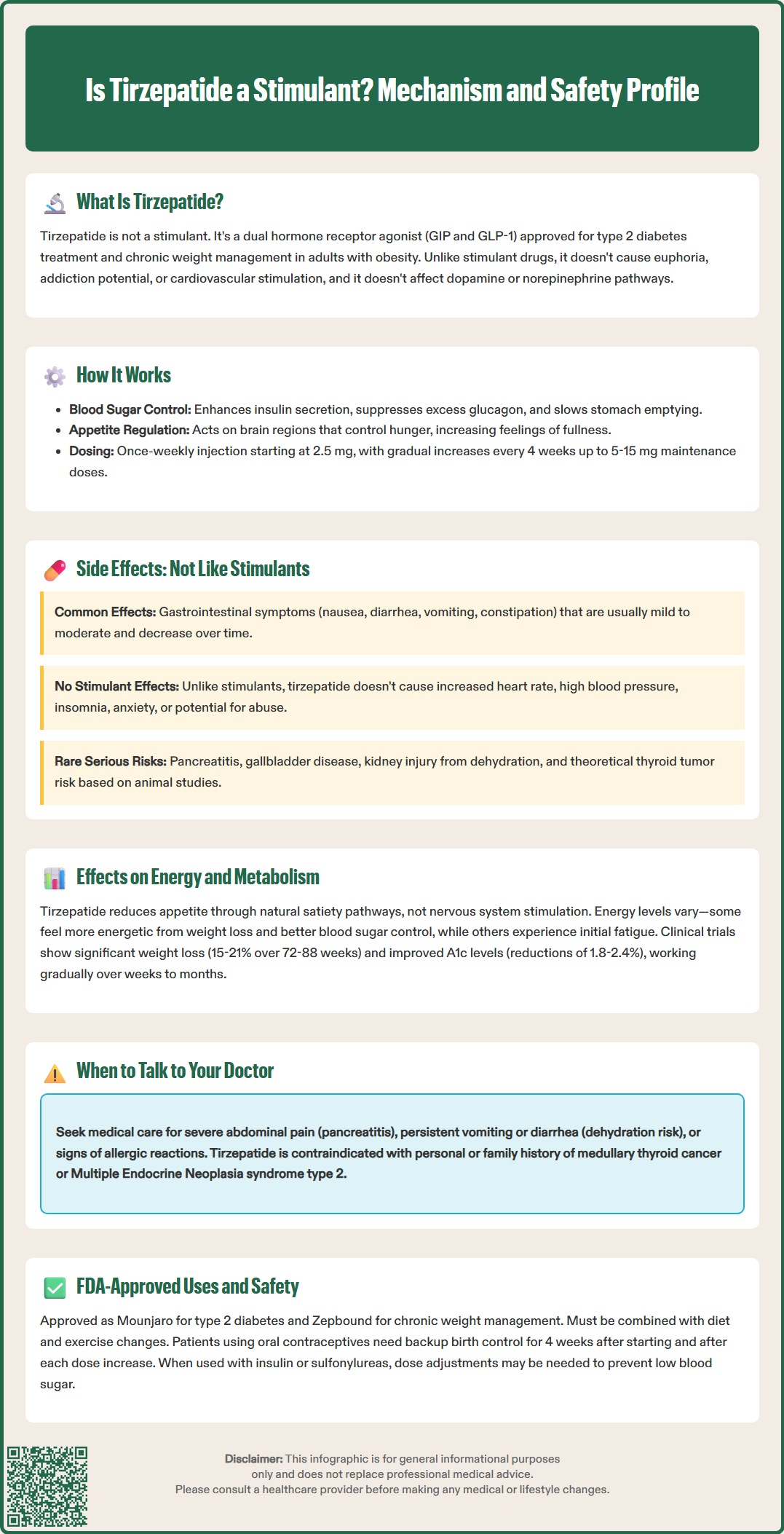
The adverse effect profile of tirzepatide is distinctly different from that of stimulant medications. The most common side effects are gastrointestinal in nature and include nausea, diarrhea, vomiting, constipation, abdominal pain, and dyspepsia. In clinical trials, these effects were generally mild to moderate in severity and tended to diminish over time as patients adapted to the medication. The gastrointestinal symptoms result from tirzepatide's mechanism of slowing gastric emptying and are dose-dependent, which is why gradual dose escalation is recommended.
In contrast, stimulant medications typically cause side effects related to sympathetic nervous system activation. These include increased heart rate (tachycardia), elevated blood pressure, insomnia, anxiety, restlessness, decreased appetite through different mechanisms, and potential for abuse or dependence. While tirzepatide does not cause the same stimulant-related effects, it is associated with small mean increases in heart rate, and patients with cardiac history should be monitored for palpitations or tachycardia symptoms. Modest reductions in blood pressure have been observed with tirzepatide, likely secondary to weight loss.
Other notable adverse effects include injection site reactions, fatigue, and hypoglycemia (particularly when used in combination with insulin or sulfonylureas). Serious but rare risks include pancreatitis, gallbladder disease, acute kidney injury (usually in the context of severe dehydration from gastrointestinal side effects), and hypersensitivity reactions including anaphylaxis and angioedema. There is also a boxed warning regarding thyroid C-cell tumors observed in rodent studies, though the relevance to humans remains uncertain. Importantly, tirzepatide may reduce the effectiveness of oral contraceptives, particularly during initiation and dose escalation; patients should use backup contraception for 4 weeks after starting treatment and after each dose increase.
While tirzepatide is not a stimulant, it does influence energy balance, appetite, and metabolic parameters through its incretin-based mechanism. Patients commonly report reduced appetite and earlier satiety, which are therapeutic effects mediated by GLP-1 and GIP receptor activation in appetite-regulating centers of the brain. This appetite suppression is fundamentally different from stimulant-induced appetite loss; tirzepatide works through physiologic satiety pathways rather than sympathetic nervous system activation.
Regarding energy levels, patient experiences vary. Some individuals report feeling more energetic as they lose weight and achieve better glycemic control, while others may experience fatigue, particularly during the initial weeks of treatment or dose escalation. This fatigue is not related to stimulant withdrawal but may reflect caloric restriction, gastrointestinal side effects, or metabolic adaptation. Unlike stimulants that artificially elevate energy through increased catecholamine activity, any energy improvements with tirzepatide are generally secondary to weight loss and improved metabolic health.
Tirzepatide significantly impacts metabolic parameters beyond glucose control. Clinical trials have demonstrated substantial weight loss (approximately 15-21% at 72-88 weeks with 10-15 mg doses in obesity trials), improvements in hemoglobin A1c (reductions of 1.8-2.4% with higher doses in diabetes trials), favorable changes in lipid profiles, and reductions in markers of cardiovascular risk. These metabolic benefits occur through enhanced insulin sensitivity, reduced hepatic glucose production, and decreased caloric intake. The medication may help preserve lean body mass better than caloric restriction alone, though resistance exercise remains important during weight loss. No completed cardiovascular outcomes trial has yet demonstrated reduction in major adverse cardiovascular events. Patients should understand that tirzepatide's metabolic effects develop gradually over weeks to months and do not produce the immediate, short-lived energy surge characteristic of stimulant medications.
Tirzepatide has two FDA-approved indications with distinct safety considerations. As Mounjaro, it is approved as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. As Zepbound, it is approved for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. The medication is not approved for type 1 diabetes or diabetic ketoacidosis.
Tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2, and in those with serious hypersensitivity to tirzepatide or its excipients. Zepbound is contraindicated during pregnancy. For Mounjaro, the medication should be discontinued when pregnancy is recognized. Concomitant use with other GLP-1 receptor agonists is not recommended.
Important safety considerations include the risk of gastrointestinal adverse effects, which can lead to dehydration and acute kidney injury if not properly managed. Patients should be counseled to maintain adequate hydration and seek medical attention if they experience severe or persistent vomiting or diarrhea. When used in patients with type 2 diabetes, particularly those on insulin or sulfonylureas, dose adjustments of these concomitant medications may be necessary to reduce hypoglycemia risk. Healthcare providers should monitor for signs and symptoms of pancreatitis (severe abdominal pain) and gallbladder disease. History of pancreatitis and severe gastrointestinal disease (such as severe gastroparesis) are important precautions, though not absolute contraindications.
Patients should be advised that tirzepatide is not a controlled substance and does not carry abuse potential like stimulant medications. However, it requires proper medical supervision, and the prescribing clinician should assess for contraindications and precautions. Regular monitoring should include assessment of glycemic control in diabetic patients, renal function, and evaluation for adverse effects. The medication should always be used as part of a comprehensive approach including dietary modification and increased physical activity.
No, tirzepatide's side effects are primarily gastrointestinal (nausea, diarrhea, vomiting) rather than stimulant-related effects like increased heart rate, elevated blood pressure, insomnia, or anxiety. It does not carry abuse potential or require controlled substance classification.
Tirzepatide reduces appetite through GIP and GLP-1 receptor activation in appetite-regulating brain centers, working through physiologic satiety pathways. This differs from stimulants, which suppress appetite through sympathetic nervous system activation and increased catecholamine activity.
No, tirzepatide is not a controlled substance and does not carry abuse or dependence potential. It requires medical supervision for safety monitoring but is not regulated as a stimulant medication.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.