LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Lightheadedness while taking tirzepatide (Mounjaro, Zepbound) can be concerning but is often manageable with proper understanding and intervention. This dual GIP/GLP-1 receptor agonist, approved by the FDA for type 2 diabetes and chronic weight management, may cause dizziness through several mechanisms including dehydration from gastrointestinal side effects, medication interactions affecting blood pressure, hypoglycemia when combined with insulin or sulfonylureas, and orthostatic hypotension related to weight loss. Recognizing the underlying causes and implementing targeted strategies helps patients safely continue therapy while minimizing symptoms. This guide provides evidence-based approaches to understanding, managing, and preventing lightheadedness during tirzepatide treatment.
Quick Answer: Lightheadedness on tirzepatide typically results from dehydration due to gastrointestinal side effects, hypoglycemia when combined with insulin or sulfonylureas, medication interactions affecting blood pressure, or orthostatic hypotension from weight loss.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). While lightheadedness is not among the most commonly reported adverse effects in clinical trials, several factors may contribute to this symptom in some individuals.
Dehydration is a primary contributor to lightheadedness during tirzepatide therapy. Gastrointestinal side effects such as nausea, vomiting, or diarrhea can lead to fluid losses, while decreased appetite may reduce overall fluid intake. This volume depletion can affect blood pressure regulation, particularly when changing positions.
Hypoglycemia is another potential cause of lightheadedness, especially when tirzepatide is combined with other glucose-lowering medications. According to FDA labeling and American Diabetes Association guidance, the risk of hypoglycemia is significantly higher when tirzepatide is used with insulin or sulfonylureas compared to tirzepatide monotherapy.
Medication interactions may increase the risk of lightheadedness. Patients taking antihypertensives (particularly diuretics, alpha-blockers, or nitrates) or SGLT2 inhibitors may experience additive effects on blood pressure or volume status when starting tirzepatide.
Rapid weight loss associated with tirzepatide therapy may contribute to orthostatic hypotension—a drop in blood pressure upon standing. As patients lose weight, adjustments to blood pressure medications are often necessary to prevent hypotension. Understanding these mechanisms helps patients and clinicians identify contributing factors and implement appropriate management strategies.
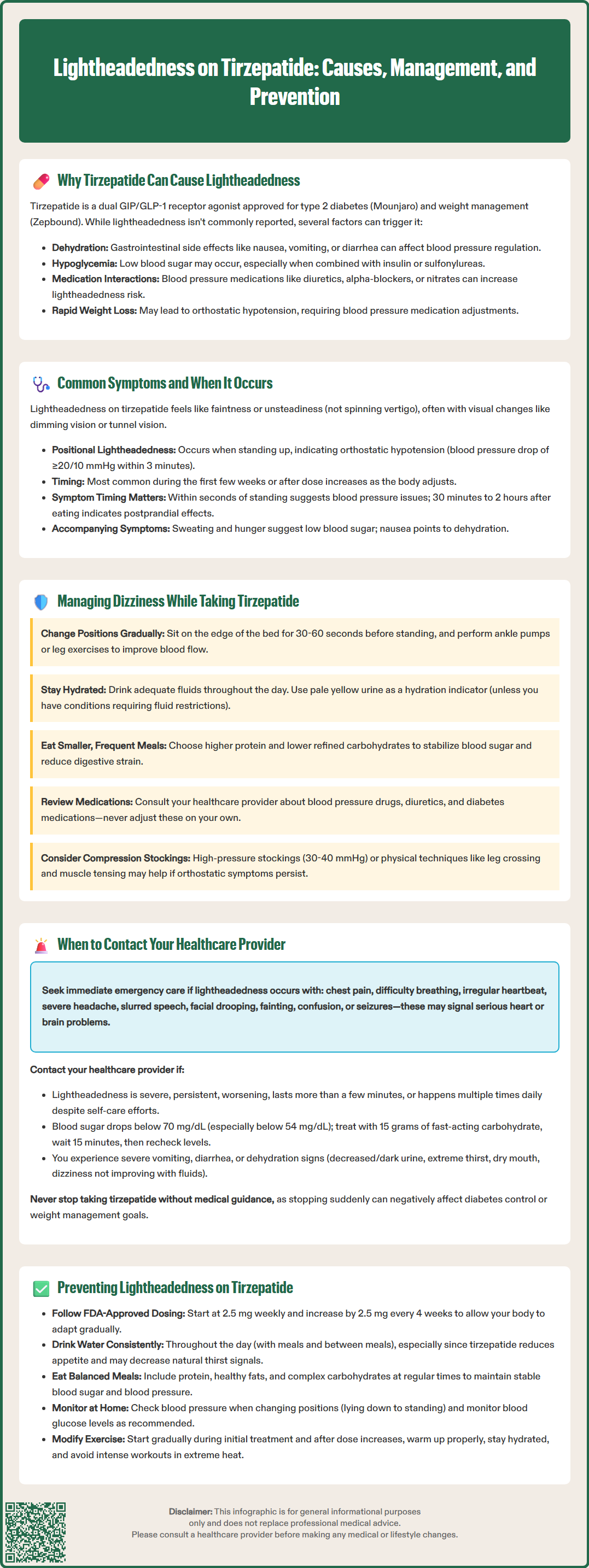
Lightheadedness (presyncope) associated with tirzepatide typically manifests as a sensation of feeling faint, unsteady, or as though one might pass out. Patients may describe feeling "woozy," experiencing visual changes such as dimming or tunnel vision, or having difficulty maintaining balance. These symptoms differ from true vertigo, which specifically involves a spinning sensation and has different causes.
The timing of lightheadedness provides important diagnostic clues. Positional lightheadedness occurs most commonly when transitioning from sitting or lying to standing, suggesting orthostatic hypotension. Clinically, orthostatic hypotension is defined as a drop of ≥20 mmHg in systolic or ≥10 mmHg in diastolic blood pressure within 3 minutes of standing. This typically happens within seconds to minutes of position change and may improve after remaining upright for a brief period. Postprandial lightheadedness develops 30 minutes to two hours after eating, particularly after large or carbohydrate-rich meals.
Lightheadedness may be more pronounced during the initial weeks of tirzepatide therapy or following dose escalation. The standard titration schedule increases the dose every four weeks, and patients may experience transient symptoms as their body adjusts to higher medication levels. Due to tirzepatide's long half-life (approximately five days) and delayed peak concentration (8-72 hours after injection), symptoms typically reflect steady-state effects rather than immediate post-injection peaks.
Accompanying symptoms help differentiate causes. Lightheadedness with sweating, tremor, palpitations, and hunger suggests hypoglycemia (blood glucose <70 mg/dL). When associated with nausea, early satiety, or abdominal discomfort, volume depletion from gastrointestinal effects may be responsible. Symptoms accompanied by excessive thirst, decreased urine output, or dry mucous membranes point toward dehydration. Recognizing these patterns enables targeted intervention and appropriate medical evaluation when necessary.
Effective management of lightheadedness on tirzepatide begins with identifying and addressing the underlying cause. For patients experiencing orthostatic symptoms, gradual position changes are essential. When rising from bed, patients should sit on the edge for 30 to 60 seconds before standing. From a seated position, standing slowly while holding onto stable furniture reduces fall risk. Performing ankle pumps or leg exercises before standing helps promote venous return.
Adequate hydration is fundamental to preventing volume depletion-related lightheadedness. Patients should maintain consistent fluid intake throughout the day, guided by thirst, urine color (pale yellow indicates adequate hydration), and individual needs. Those experiencing gastrointestinal side effects may require additional fluid replacement. Patients with heart failure, kidney disease, or other conditions requiring fluid restrictions should follow their healthcare provider's specific recommendations for fluid intake.
Dietary modifications can help stabilize blood pressure and glucose. Eating smaller, more frequent meals rather than large portions reduces the hemodynamic demands of digestion. Limiting refined carbohydrates and increasing protein intake helps stabilize blood glucose. Avoiding alcohol, which causes vasodilation and can worsen hypotension, is advisable, particularly during the adjustment period.
For patients taking concomitant medications, medication review with a healthcare provider is crucial. Blood pressure medications, diuretics, and SGLT2 inhibitors may require dose adjustment as weight loss and improved insulin sensitivity occur. Similarly, doses of sulfonylureas or insulin often need reduction to prevent hypoglycemia. Patients should never adjust these medications independently.
Compression garments may benefit individuals with persistent orthostatic symptoms. For orthostatic hypotension, higher-pressure compression stockings (30-40 mmHg) or abdominal binders are more effective than lower-pressure options. Physical countermaneuvers such as leg crossing, squatting, or tensing leg muscles before standing can also raise blood pressure acutely. If symptoms persist despite these measures, patients should discuss with their provider whether maintaining the current tirzepatide dose longer before escalating might be appropriate.
While mild, transient lightheadedness may resolve with conservative measures, certain symptoms warrant prompt medical evaluation. Patients should contact their healthcare provider if lightheadedness is severe, persistent, or worsening despite self-management strategies. Symptoms lasting more than a few minutes or occurring multiple times daily require professional assessment.
Immediate medical attention is necessary if lightheadedness is accompanied by:
Chest pain, pressure, or tightness
Severe shortness of breath or difficulty breathing
Irregular or rapid heartbeat (palpitations)
Severe headache, particularly if sudden onset
Slurred speech, facial drooping, or weakness on one side of the body
Loss of consciousness or fainting episodes
Confusion or altered mental status
Seizure activity
These symptoms may indicate serious cardiovascular or neurological events requiring emergency evaluation. Patients experiencing syncope (actual loss of consciousness) should seek immediate care, as this suggests significant hemodynamic compromise.
Patients should also contact their provider if they experience hypoglycemia (blood glucose below 70 mg/dL) or severe hypoglycemia (below 54 mg/dL), particularly if taking insulin or sulfonylureas. For hypoglycemia, patients should follow the 15-15 rule: consume 15 grams of fast-acting carbohydrate, wait 15 minutes, and recheck blood glucose.
Severe or persistent vomiting or diarrhea requires medical attention due to the risk of dehydration and potential acute kidney injury. Similarly, signs of severe dehydration—including decreased urine output, dark urine, extreme thirst, dry mouth, or dizziness that improves minimally with fluid intake—require medical assessment.
Lightheadedness that interferes with daily activities, increases fall risk, or causes significant anxiety warrants discussion with a healthcare provider. A thorough evaluation can identify contributing factors, rule out alternative diagnoses, and guide appropriate management. Patients should never discontinue tirzepatide without medical guidance, as abrupt cessation may affect diabetes control or weight management goals.
Proactive strategies can significantly reduce the likelihood of experiencing lightheadedness while taking tirzepatide. Proper medication titration following the FDA-approved dosing schedule allows the body to adapt gradually to the medication's effects. Tirzepatide typically starts at 2.5 mg once weekly for four weeks, then increases by 2.5 mg increments every 4 weeks as tolerated, up to a maximum of 15 mg weekly. Rushing dose escalation increases the risk of adverse effects, including lightheadedness.
Maintaining consistent hydration from the outset of therapy prevents volume depletion. Patients should establish a hydration routine, such as drinking a glass of water with each meal and between meals. Those with reduced appetite due to tirzepatide's effects must make conscious efforts to maintain fluid intake despite decreased thirst signals. Patients with heart failure, kidney disease, or hypertension should follow their healthcare provider's specific recommendations regarding fluid and sodium intake.
Dietary planning supports stable blood glucose and blood pressure. Balanced meals containing adequate protein, healthy fats, and complex carbohydrates prevent reactive hypoglycemia. Avoiding prolonged fasting and maintaining regular meal timing helps stabilize metabolic parameters. Sodium intake should be individualized based on underlying medical conditions—patients should consult their provider regarding appropriate levels.
Regular monitoring enables early identification of trends that might lead to lightheadedness. Home blood pressure monitoring, particularly orthostatic measurements (after 5 minutes lying down, then at 1 and 3 minutes after standing), can detect positional blood pressure changes before symptoms become problematic. Patients taking medications that affect blood glucose should monitor levels as recommended by their healthcare team, typically before meals and at bedtime initially.
Physical activity modifications during the adjustment period may be necessary. While exercise is beneficial for diabetes management and weight loss, patients should avoid sudden intense exertion during the first weeks of therapy or after dose increases. Gradual warm-up and cool-down periods, adequate hydration before and during exercise, and avoiding exercise in extreme heat reduce lightheadedness risk. Communication with healthcare providers about preventive strategies, medication interactions, and individual risk factors optimizes safety and treatment success with tirzepatide therapy.
Lightheadedness is typically most pronounced during the initial weeks of tirzepatide therapy or following dose escalation, often improving as the body adjusts over several days to weeks. If symptoms persist beyond the adjustment period or worsen, contact your healthcare provider for evaluation.
Mild, transient lightheadedness can often be managed with hydration, gradual position changes, and dietary modifications while continuing tirzepatide. However, never discontinue or adjust tirzepatide without medical guidance, and contact your provider if symptoms are severe, persistent, or accompanied by concerning signs like chest pain or loss of consciousness.
Yes, checking blood pressure when lightheaded helps identify orthostatic hypotension. Measure after lying down for 5 minutes, then at 1 and 3 minutes after standing—a drop of ≥20 mmHg systolic or ≥10 mmHg diastolic indicates orthostatic hypotension requiring discussion with your healthcare provider.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.