LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Missing a dose of semaglutide, a once-weekly GLP-1 receptor agonist used for type 2 diabetes and chronic weight management, is a common concern for patients. The appropriate action depends on how much time has passed since your scheduled injection. For Ozempic (diabetes treatment), you can take a missed dose within five days of your scheduled time. For Wegovy (weight management), timing depends on when your next dose is due. Understanding the correct steps to take when you miss a dose helps maintain treatment effectiveness and minimizes potential side effects. This guide provides clear, evidence-based instructions for managing missed semaglutide doses safely.
Quick Answer: If you miss a dose of semaglutide, take it within five days for Ozempic or if your next Wegovy dose is more than two days away; otherwise, skip the missed dose and resume your regular schedule.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist administered once weekly for type 2 diabetes management and chronic weight management. Missing a scheduled dose is a common occurrence, and the appropriate response depends on how much time has elapsed since your missed injection.
For injectable semaglutide (Ozempic) used for diabetes: If you remember within five days (120 hours) of your scheduled dose, administer the injection as soon as possible. Then take your next dose on your regularly scheduled day. For example, if your usual injection day is Monday and you remember on Thursday, take the missed dose immediately and then continue with your next dose on the following Monday.
For Wegovy (semaglutide for weight management): If your next scheduled dose is more than 2 days away, take the missed dose as soon as possible. If your next scheduled dose is within 2 days, skip the missed dose and take the next injection on the regular scheduled day.
For both medications, if more than five days have passed since your scheduled Ozempic dose (or if you're outside the Wegovy timing window), skip the missed injection entirely. Do not take a double dose to compensate. Instead, wait until your next regularly scheduled injection day and resume your normal dosing pattern.
Note that these instructions apply only to injectable semaglutide; oral semaglutide (Rybelsus) has different missed-dose instructions.
Contact your healthcare provider if you are uncertain about what to do, if you have missed multiple consecutive doses, or if you experience severe or persistent side effects. If you take insulin or sulfonylureas along with semaglutide, missing doses may affect your blood glucose levels, requiring additional monitoring. Never adjust your dosing schedule without medical guidance, as semaglutide's efficacy depends on maintaining therapeutic levels.
According to FDA labeling, injectable semaglutide offers some flexibility in dosing. For Ozempic, the five-day window represents the period during which you can take a missed dose without skipping it entirely. For Wegovy, timing is relative to your next scheduled dose.
Semaglutide's extended half-life of approximately one week contributes to this flexibility. The medication works by binding to GLP-1 receptors in pancreatic beta cells, enhancing glucose-dependent insulin secretion, suppressing glucagon release, and slowing gastric emptying. These effects require consistent drug levels to maintain glycemic control and appetite suppression.
If you wish to permanently change your weekly injection day, you can do so as long as at least 48 hours have elapsed since your last dose. This allows you to adjust your schedule while maintaining appropriate intervals between injections.
The FDA-approved semaglutide formulations include Ozempic (for type 2 diabetes) and Wegovy (for chronic weight management). Both products contain the same active ingredient but differ in maximum approved doses and indications, with product-specific guidance for missed doses.
Clinical considerations for delayed dosing include the potential for breakthrough hyperglycemia in patients with diabetes and increased appetite in those using semaglutide for weight management. If you consistently find yourself unable to maintain a weekly schedule, discuss alternative injection days with your healthcare provider. Some patients benefit from choosing a day when they have a consistent routine, such as a weekend morning, to improve adherence. The American Diabetes Association's Standards of Care emphasizes that medication adherence is a critical component of diabetes self-management and treatment success.
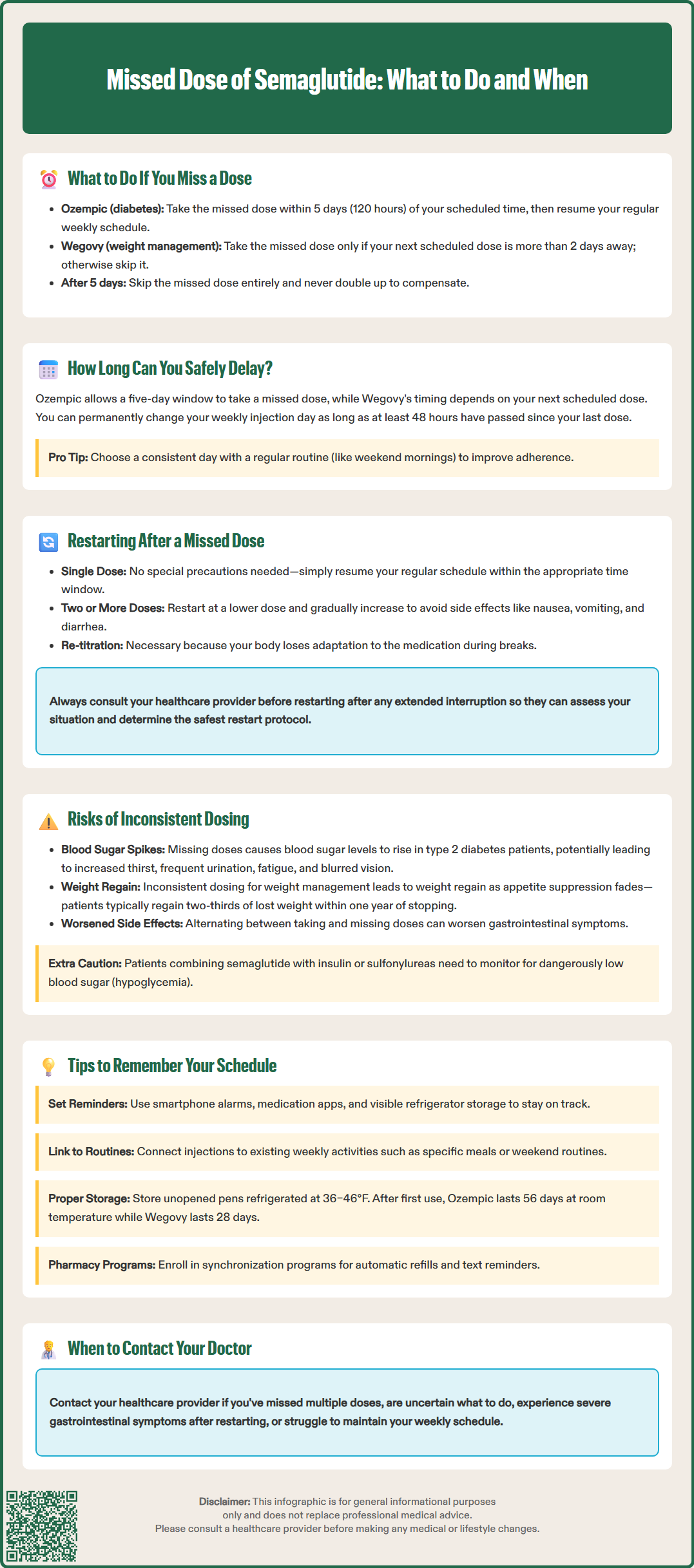
Restarting semaglutide after a single missed dose within the appropriate window typically requires no special precautions beyond resuming your regular schedule. However, the approach differs significantly if you've missed multiple doses or have been off treatment for an extended period.
For Wegovy, if you miss two or more consecutive doses, the FDA labeling recommends considering re-escalation of the dose. For Ozempic, extended interruptions may also benefit from dose re-titration to minimize side effects.
The standard titration for Ozempic begins at 0.25 mg weekly for four weeks, increasing to 0.5 mg weekly, with potential further increases to 1 mg or 2 mg based on glycemic response and tolerability. Wegovy follows a more gradual escalation pattern, starting at 0.25 mg and increasing monthly through 0.5 mg, 1.0 mg, 1.7 mg, to a maintenance dose of 2.4 mg weekly.
The rationale for re-titration relates to gastrointestinal tolerability. Semaglutide's most common adverse effects—nausea, vomiting, diarrhea, and abdominal pain—are dose-dependent and typically occur during dose escalation. When treatment is interrupted for extended periods, the body may lose its adaptation to the medication, and restarting at a full maintenance dose could increase the risk of gastrointestinal symptoms.
Consult your healthcare provider before restarting semaglutide after any extended interruption. Your provider will assess factors including the duration of interruption, your previous dose, your current glycemic control (if diabetic), and any changes in your medical status. Some patients may require clinical evaluation before resuming therapy, particularly if they've experienced significant changes in health status. If you develop severe gastrointestinal symptoms upon restarting, contact your provider, as stepping down to a lower dose and re-escalating may be necessary.
Inconsistent semaglutide dosing can compromise both treatment efficacy and safety. The most immediate concern for patients with type 2 diabetes is loss of glycemic control. Semaglutide typically reduces hemoglobin A1C by approximately 1.0–1.5 percentage points when taken consistently, as demonstrated in the SUSTAIN clinical trials. Missing doses allows blood glucose levels to rise, potentially leading to hyperglycemic symptoms including increased thirst, frequent urination, fatigue, and blurred vision. Prolonged periods of poor glycemic control increase the risk of both acute complications and long-term microvascular and macrovascular damage.
For patients using semaglutide for chronic weight management, inconsistent dosing may result in weight regain and loss of appetite control. The medication's effects on satiety and gastric emptying diminish as drug levels decline, potentially triggering increased hunger and food intake. Clinical trials demonstrate that discontinuation of semaglutide typically results in gradual weight regain, with patients recovering approximately two-thirds of lost weight within one year of stopping treatment, according to STEP trial extension data.
Gastrointestinal side effects may be more noticeable when dosing is inconsistent. When patients alternate between taking and missing doses, the gastrointestinal tract may not fully adapt to the medication. This can make side effects more challenging to manage than with consistent dosing.
Patients taking semaglutide with insulin or sulfonylureas should be particularly vigilant about consistent dosing, as these combinations can increase hypoglycemia risk. If you miss a semaglutide dose and use these medications, monitor your blood glucose more frequently and contact your provider if you notice significant changes.
There is no evidence that occasional missed doses cause serious adverse events such as pancreatitis or thyroid tumors—risks associated with the drug class but not specifically linked to dosing inconsistency. However, patients should report any new or worsening abdominal pain to their healthcare provider, regardless of dosing patterns. The FDA label includes a boxed warning about thyroid C-cell tumors observed in rodent studies, though the relevance to humans remains uncertain. Maintaining consistent dosing as prescribed optimizes the benefit-risk profile of semaglutide therapy.
Establishing a consistent routine is the most effective strategy for maintaining adherence to weekly semaglutide injections. Choose a specific day and time that aligns with your regular schedule—many patients find success with weekend mornings when they have more time and fewer competing demands. Consistency in timing, while not strictly required, helps establish a habit and reduces the likelihood of forgotten doses.
Practical adherence strategies include:
Set multiple reminders: Use smartphone alarms, calendar notifications, or medication reminder apps that alert you on injection day and send follow-up reminders if you don't confirm completion.
Link to existing habits: Pair your injection with an established weekly routine, such as a specific meal, religious service attendance, or weekend activity.
Visible storage: Keep your semaglutide pen in a consistent location in your refrigerator where you'll see it regularly. Store in the original carton to protect from light, and keep out of reach of children. Never store with the needle attached.
Prefill injection logs: Maintain a simple calendar or checklist specifically for tracking injections, checking off each dose as completed.
Involve family members: Ask household members to help remind you, particularly if you have a partner who can provide gentle prompts.
Proper storage is essential: Refrigerate unopened pens at 36–46°F (2–8°C). Do not freeze. After first use, Ozempic pens can be stored at room temperature (up to 86°F/30°C) for up to 56 days. Wegovy single-use pens can be stored at room temperature for up to 28 days. Always protect from light and follow product-specific instructions.
Pharmacy synchronization programs can also improve adherence by ensuring you never run out of medication. Many pharmacies offer automatic refill services and text message reminders when prescriptions are ready. If you travel frequently, plan ahead by checking your supply and understanding proper storage requirements for semaglutide pens during transit.
Consider using a pill box or medication organizer with weekly compartments, even though semaglutide is injectable. Place a note or token in the appropriate day's compartment as a visual reminder. The American Diabetes Association recommends that healthcare providers assess medication adherence at each visit and work collaboratively with patients to identify and address barriers to consistent dosing.
No, never take a double dose of semaglutide to make up for a missed injection. If more than five days have passed for Ozempic (or you're outside the timing window for Wegovy), skip the missed dose entirely and resume your regular weekly schedule.
Missing multiple consecutive doses may require restarting at a lower dose and gradually re-escalating to minimize gastrointestinal side effects. Contact your healthcare provider before resuming treatment after an extended interruption to determine the appropriate restart protocol.
Missing a single dose may cause temporary increases in blood glucose levels for diabetes patients and reduced appetite control for weight management patients. However, semaglutide's one-week half-life provides some buffer, and resuming your regular schedule promptly typically restores therapeutic effects without significant long-term impact.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.