LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, has transformed treatment for type 2 diabetes and obesity. As more patients achieve significant weight loss with this GLP-1 receptor agonist, concerns about semaglutide and hair loss have emerged. While alopecia appears in Wegovy's FDA label at low frequency, the relationship between this medication and hair thinning remains complex. Hair changes may result from rapid weight loss itself, nutritional factors, or metabolic stress rather than direct drug effects. Understanding this connection helps patients and providers make informed decisions about treatment and hair health management.
Quick Answer: Semaglutide may be associated with hair loss, though this typically results from rapid weight loss and nutritional factors rather than direct medication effects.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for two primary indications: type 2 diabetes management (marketed as Ozempic and Rybelsus) and chronic weight management (marketed as Wegovy). This medication mimics the action of naturally occurring GLP-1, a hormone that plays a crucial role in glucose metabolism and appetite regulation.
The mechanism of action involves binding to GLP-1 receptors in multiple tissues throughout the body. In the pancreas, semaglutide stimulates insulin secretion in a glucose-dependent manner, meaning it promotes insulin release only when blood glucose levels are elevated. This reduces the risk of hypoglycemia when used alone, though the risk increases when combined with insulin or sulfonylureas. Simultaneously, it suppresses glucagon secretion, further helping to control blood sugar levels.
Beyond glycemic control, semaglutide acts on receptors in the brain, particularly in areas that regulate appetite and food intake. This leads to increased satiety, reduced hunger, and delayed gastric emptying (an effect that may diminish over time), which collectively contribute to significant weight loss. Clinical trials have demonstrated that patients using semaglutide for weight management can achieve an average weight reduction of approximately 15% of their initial body weight over 68 weeks, with some individuals achieving 20% or greater weight loss.
The medication is administered as a once-weekly subcutaneous injection, with dosing gradually increased over several weeks to minimize gastrointestinal side effects. Common adverse effects include nausea, vomiting, diarrhea, and constipation. Important safety considerations include risks of medullary thyroid carcinoma (contraindicated in patients with MEN2 or family history of MTC), pancreatitis, gallbladder disease, acute kidney injury with severe gastrointestinal adverse effects, and potential diabetic retinopathy complications in patients with type 2 diabetes. Semaglutide should not be used during pregnancy. Understanding how semaglutide works provides important context when considering its potential effects on other body systems, including hair growth.
The relationship between semaglutide and hair loss remains an area of clinical interest. While alopecia is not listed among the adverse reactions in the FDA-approved prescribing information for Ozempic, it is documented in the Wegovy label as occurring at a low frequency and more often than placebo. This difference in labeling highlights the importance of considering the specific semaglutide product when evaluating potential side effects.
Several factors complicate the assessment of whether semaglutide directly causes hair loss. First, the medication is primarily prescribed to patients with obesity or type 2 diabetes—conditions that themselves may be associated with hair changes due to metabolic disturbances, hormonal imbalances, or nutritional deficiencies. Second, the rapid weight loss achieved with semaglutide treatment may trigger a specific type of temporary hair shedding known as telogen effluvium, which is well-documented with significant weight reduction regardless of the method used.
While the Wegovy clinical trials documented alopecia occurring more frequently than in placebo groups, the overall incidence was relatively low, and a direct causal relationship has not been definitively established. It is important to note that correlation does not equal causation—patients experiencing hair thinning while taking semaglutide may be responding to multiple concurrent factors rather than the medication itself.
Healthcare providers should maintain awareness of patient concerns regarding hair changes and approach each case individually. A thorough assessment of potential contributing factors, including nutritional status, rate of weight loss, underlying medical conditions, and concurrent medications, is essential before attributing hair loss specifically to semaglutide therapy.
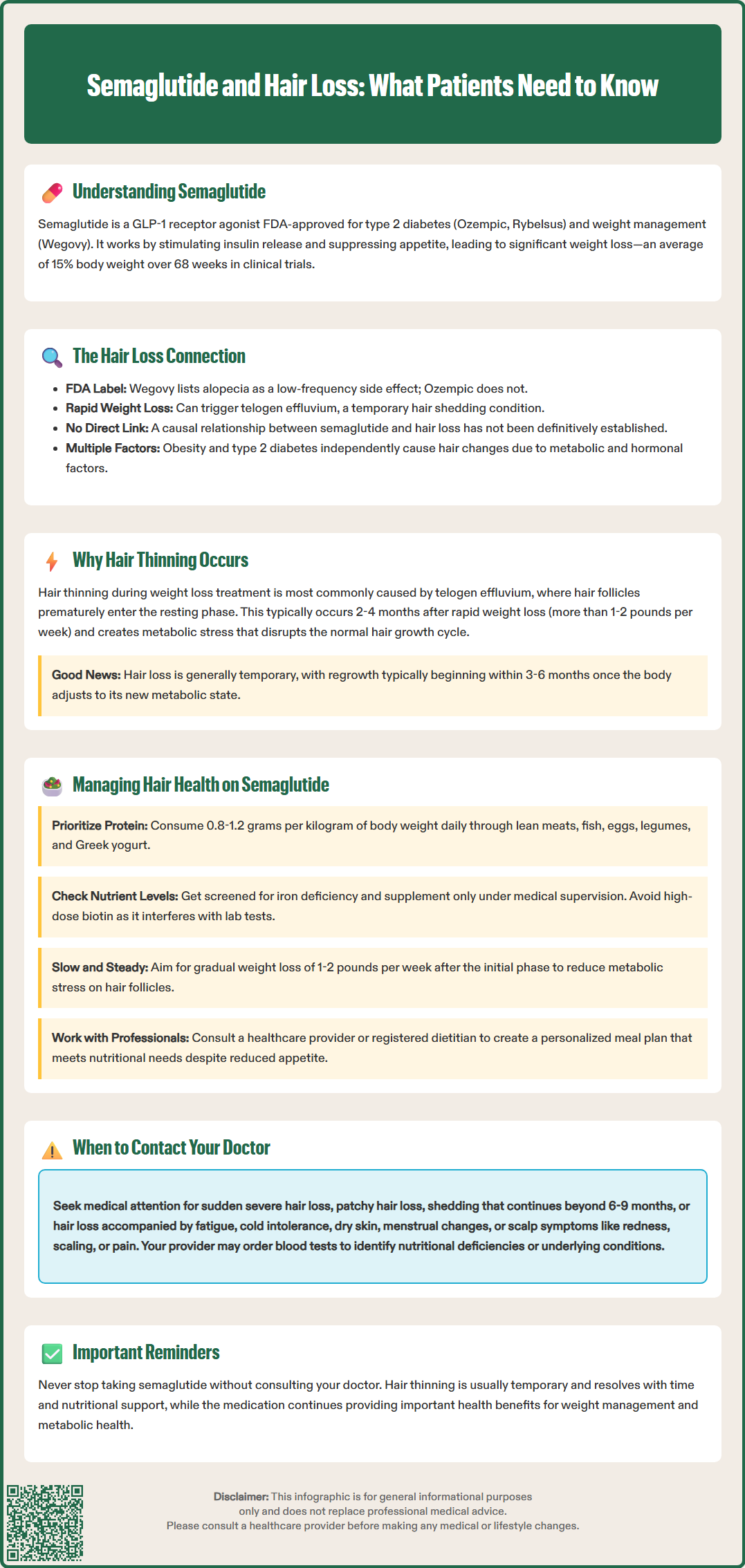
Hair thinning during weight loss treatment, including with semaglutide, can be explained by several physiological mechanisms that are not necessarily drug-specific. The most common cause is telogen effluvium, a temporary condition where a significant number of hair follicles prematurely enter the resting (telogen) phase of the hair growth cycle. This typically occurs 2-4 months after a triggering event, such as rapid weight loss, acute illness, major surgery, or the postpartum period, and results in diffuse hair shedding.
Rapid weight loss—defined as losing more than 1-2 pounds per week—places physiological stress on the body. This metabolic stress can disrupt the normal hair growth cycle, causing follicles to shift from the active growth phase (anagen) to the resting phase. Studies have shown that individuals losing significant weight through any method, including bariatric surgery, very low-calorie diets, or medications like semaglutide, may experience this phenomenon. The hair loss is generally temporary, with regrowth typically beginning within 3-6 months once the body adjusts to the new metabolic state.
Nutritional deficiencies represent another critical factor. Rapid weight loss can lead to inadequate intake of essential nutrients vital for hair health, including protein, iron, zinc, and vitamins D and E. Biotin deficiency is uncommon but may contribute in rare cases, while excessive vitamin A intake can actually worsen hair loss. Protein is particularly important, as hair follicles are among the most metabolically active tissues in the body and require adequate amino acid supply. Patients on aggressive calorie restriction may not consume sufficient protein to support both weight loss and hair maintenance.
Additionally, hormonal changes accompanying significant weight loss may affect hair growth. Thyroid dysfunction should be evaluated as a potential cause of hair loss. Patients with pre-existing conditions such as polycystic ovary syndrome (PCOS) or thyroid disorders may be particularly susceptible to hair changes during weight loss treatment, though the evidence linking other hormonal shifts directly to hair loss is limited.
Proactive strategies can help minimize hair thinning and support hair health during semaglutide treatment. The cornerstone of prevention is ensuring adequate nutritional intake despite reduced appetite and caloric consumption. Patients should work with their healthcare provider or a registered dietitian to develop a meal plan that meets individual protein requirements—typically 0.8-1.2 grams per kilogram of body weight daily, with potentially higher needs during caloric restriction.
Key nutritional considerations include:
Protein intake: Prioritize lean proteins such as chicken, fish, eggs, legumes, and Greek yogurt at each meal to support hair follicle function.
Iron status: Consider screening for iron deficiency with a complete iron panel (ferritin, serum iron, TIBC, transferrin saturation), particularly in menstruating women. Iron supplementation should only be initiated with confirmed deficiency and under clinical supervision.
Vitamin considerations: Discuss appropriate multivitamin support with your healthcare provider. Note that high-dose biotin supplements (often marketed for hair health) can interfere with laboratory test results, including thyroid function tests and cardiac markers.
Hydration: Adequate fluid intake supports overall metabolic function and nutrient delivery to hair follicles.
The rate of weight loss should be monitored and moderated when possible. While semaglutide is highly effective for weight reduction, aiming for a gradual loss of 1-2 pounds per week after the initial phase may reduce metabolic stress on hair follicles. Healthcare providers can adjust dosing schedules if weight loss is occurring too rapidly.
Gentle hair care practices may also be helpful, though evidence for specific approaches is limited. Some dermatologists suggest avoiding excessive heat styling and tight hairstyles that create tension on the scalp. While some patients find that reducing washing frequency or using sulfate-free shampoos helps maintain hair condition, these approaches have limited scientific evidence for preventing telogen effluvium.
For persistent hair thinning, topical minoxidil may be an option to discuss with your healthcare provider or dermatologist. While over-the-counter supplements marketed for hair growth are widely available, evidence supporting their efficacy is limited. Patients should discuss any supplements with their healthcare provider before use, as some may interact with medications or underlying conditions.
While mild hair thinning during significant weight loss may be expected and temporary, certain signs warrant prompt medical evaluation. Patients should contact their healthcare provider if they experience sudden or severe hair loss, particularly if it occurs in patches rather than diffuse thinning, as this may indicate alopecia areata or other dermatological conditions unrelated to weight loss or medication.
Specific situations requiring medical assessment include:
Rapid onset: Hair loss beginning within the first month of treatment, before significant weight loss has occurred, may suggest an alternative cause.
Associated symptoms: Hair changes accompanied by fatigue, cold intolerance, dry skin, or changes in menstrual patterns may indicate thyroid dysfunction requiring investigation.
Scalp changes: Redness, scaling, itching, or pain on the scalp suggests a dermatological condition that needs specific treatment.
Persistent shedding: Hair loss continuing beyond 6-9 months or worsening over time despite nutritional optimization.
Healthcare providers should conduct a thorough evaluation including medical history, physical examination of the scalp and hair, and appropriate laboratory investigations. Recommended screening tests may include complete blood count, comprehensive metabolic panel, iron studies (ferritin, serum iron, TIBC, transferrin saturation), thyroid function tests (TSH, free T4), vitamin B12 (especially in patients taking metformin), vitamin D levels, and potentially other assessments based on clinical suspicion. Pregnancy testing may be appropriate in some cases.
In some cases, referral to a dermatologist specializing in hair disorders may be appropriate, particularly if hair loss is severe, atypical in pattern, or not responding to conservative management. Referral to endocrinology may be warranted if thyroid or other endocrine disorders are suspected. Dermatologists can perform additional diagnostic procedures such as scalp biopsy or trichoscopy if needed.
Patients should never discontinue semaglutide without consulting their healthcare provider, as the medication provides important benefits for diabetes management or weight loss. In most cases, hair thinning is temporary and resolves with time and nutritional support, making medication discontinuation unnecessary. A collaborative approach between patient and provider ensures both the continuation of beneficial treatment and appropriate management of any adverse effects.
While alopecia appears in Wegovy's FDA label at low frequency, hair loss during semaglutide treatment more commonly results from rapid weight loss triggering telogen effluvium rather than direct drug effects. A definitive causal relationship has not been established.
Hair shedding typically begins 2-4 months after rapid weight loss and is usually temporary, with regrowth beginning within 3-6 months once the body adjusts to metabolic changes and nutritional status is optimized.
Ensure adequate protein intake (0.8-1.2 g/kg daily), maintain gradual weight loss of 1-2 pounds weekly when possible, work with a healthcare provider to screen for nutritional deficiencies (especially iron), and stay well-hydrated throughout treatment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.