LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, a GLP-1 receptor agonist approved for type 2 diabetes and weight management, raises important safety questions for patients with ulcerative colitis. While FDA labeling includes no specific contraindication for inflammatory bowel disease, the medication's gastrointestinal side effects—including nausea, diarrhea, and abdominal pain—overlap significantly with ulcerative colitis symptoms. This overlap creates challenges in distinguishing medication effects from disease flares. Understanding the relationship between semaglutide and ulcerative colitis helps patients and clinicians make informed treatment decisions when metabolic conditions coexist with inflammatory bowel disease.
Quick Answer: Semaglutide is not contraindicated in ulcerative colitis, but its gastrointestinal side effects may complicate symptom monitoring and disease management.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for multiple indications: type 2 diabetes mellitus (T2D), chronic weight management, and cardiovascular risk reduction. For diabetes, it's marketed as Ozempic (injectable, up to 2 mg weekly) and Rybelsus (oral, 7-14 mg daily). For weight management, it's available as Wegovy (injectable, up to 2.4 mg weekly). Ozempic is also indicated to reduce cardiovascular risk in adults with T2D and established cardiovascular disease, while Wegovy is indicated for cardiovascular risk reduction in adults with established cardiovascular disease who have overweight or obesity.
The medication works by mimicking the action of endogenous GLP-1, a hormone naturally produced in the intestinal tract. Semaglutide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon release, and slows gastric emptying. These mechanisms collectively improve glycemic control in patients with type 2 diabetes. Additionally, semaglutide acts on appetite-regulating centers in the brain, promoting satiety and reducing caloric intake, which contributes to its effectiveness for weight management.
Semaglutide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Wegovy is contraindicated during pregnancy. The medication is not recommended for patients with severe gastroparesis and requires careful monitoring in patients with diabetic retinopathy due to potential worsening with rapid glucose improvement.
Injectable formulations are typically initiated at low doses (0.25 mg weekly for Ozempic/Wegovy) and gradually titrated upward to minimize gastrointestinal side effects, which are among the most common adverse reactions. Oral semaglutide (Rybelsus) requires specific administration instructions: taking on an empty stomach with a small amount of water and waiting at least 30 minutes before consuming food, beverages, or other medications.
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) characterized by continuous mucosal inflammation of the colon, typically beginning in the rectum and extending proximally to varying degrees. The condition affects approximately 250 per 100,000 adults in the United States, with peak onset between ages 15 and 30 years, though it can develop at any age.
The hallmark symptoms of ulcerative colitis include bloody diarrhea, abdominal cramping, urgency, and tenesmus. Disease severity ranges from mild proctitis affecting only the rectum to severe pancolitis involving the entire colon. Patients may experience periods of remission alternating with acute flares. Extraintestinal manifestations can include arthritis, skin lesions, eye inflammation, and primary sclerosing cholangitis. Chronic inflammation increases the risk of colorectal cancer, necessitating regular surveillance colonoscopy, typically beginning 8 years after disease onset for extensive colitis, with intervals of 1-3 years based on individual risk factors.
Diagnosis requires colonoscopy with mucosal biopsies demonstrating characteristic histologic features: continuous inflammation limited to the mucosa and submucosa, crypt architectural distortion, and increased inflammatory cells. Laboratory markers such as C-reactive protein and fecal calprotectin help assess disease activity.
Management strategies depend on disease extent and severity. Mild-to-moderate disease typically responds to 5-aminosalicylic acid (5-ASA) compounds such as mesalamine. Moderate-to-severe cases may require corticosteroids for acute flares, followed by immunomodulators (azathioprine, 6-mercaptopurine) or biologic agents (anti-TNF therapies, vedolizumab, ustekinumab). Newer JAK inhibitors (tofacitinib, upadacitinib) and S1P modulators (ozanimod) offer additional options. Surgical colectomy becomes necessary in approximately 10-15% of patients with contemporary medical therapy, though rates vary by disease severity and treatment era.
Patients with UC require careful monitoring of nutritional status, as chronic inflammation and diarrhea can lead to malabsorption, anemia, and weight loss. Conversely, some patients gain weight during remission or with corticosteroid therapy, creating complex metabolic considerations.
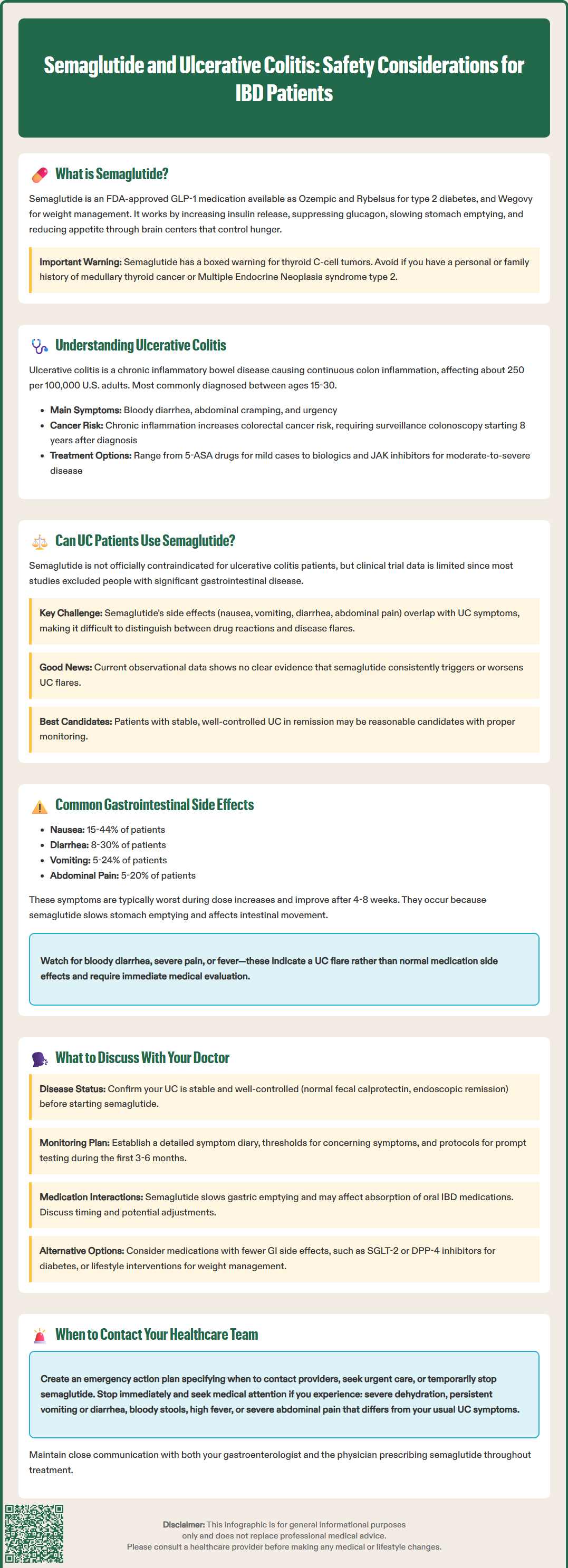
The question of semaglutide safety in patients with ulcerative colitis requires careful consideration. Currently, there is no official contraindication to its use in IBD patients in FDA labeling, but specific clinical trial data addressing this population is limited. Many clinical trials for semaglutide excluded patients with significant gastrointestinal disease, so evidence regarding safety in UC comes primarily from limited observational data and clinical experience.
Several theoretical concerns warrant clinical judgment. Semaglutide's mechanism of slowing gastric emptying and its common gastrointestinal side effects—including nausea, vomiting, diarrhea, and abdominal pain—overlap significantly with UC symptoms. This overlap creates potential challenges in distinguishing medication side effects from disease flares, which could delay appropriate escalation of IBD therapy. Additionally, the medication's effects on gut motility and the gastrointestinal microenvironment have not been extensively studied in the context of active intestinal inflammation.
Available observational data have not identified a clear signal suggesting that semaglutide consistently triggers or exacerbates ulcerative colitis flares, though evidence remains limited. Some gastroenterologists have prescribed GLP-1 receptor agonists to patients with well-controlled IBD, particularly when metabolic benefits outweigh theoretical risks. The decision requires individualized assessment of disease activity, stability of remission, and the presence of comorbid conditions such as diabetes or obesity that might benefit from semaglutide therapy.
Patients with active or poorly controlled ulcerative colitis may benefit from achieving better disease control before initiating semaglutide, based on clinical judgment rather than formal guidelines. Those with stable, quiescent disease may be reasonable candidates, provided they understand the importance of monitoring for symptom changes and maintaining close communication with both their gastroenterologist and prescribing physician. Patients should be counseled about the risk of dehydration and potential acute kidney injury with severe gastrointestinal symptoms, and the need to temporarily hold medication and seek care if severe vomiting or diarrhea occurs. All standard semaglutide contraindications and warnings apply, including the boxed warning for thyroid C-cell tumors and pregnancy contraindication for Wegovy.
Gastrointestinal adverse effects represent the most frequently reported side effects of semaglutide therapy, with rates varying by dose, formulation, and indication. These effects are particularly important to understand for patients with underlying digestive disorders like ulcerative colitis.
The most common gastrointestinal side effects include:
Nausea: Reported in 15-44% of patients (higher rates at Wegovy 2.4 mg), typically most pronounced during dose escalation
Diarrhea: Affects approximately 8-30% of users, ranging from mild to moderate severity
Vomiting: Occurs in 5-24% of patients (higher rates at Wegovy 2.4 mg), often associated with rapid dose increases
Abdominal pain: Experienced by 5-20% of patients, usually described as cramping or discomfort
Constipation: Paradoxically affects 3-24% despite the medication's effects on motility
Dyspepsia and gastroesophageal reflux: Related to delayed gastric emptying
These effects result from semaglutide's pharmacologic action on GLP-1 receptors throughout the gastrointestinal tract. The medication slows gastric emptying, which contributes to satiety but can also cause upper GI symptoms. Effects on intestinal motility and secretion may contribute to changes in bowel habits. Most gastrointestinal side effects are dose-dependent and tend to diminish over time as patients develop tolerance, typically improving after 4-8 weeks at a stable dose.
More serious but rare gastrointestinal complications have been reported, including pancreatitis (though causality remains debated), gallbladder disease, and ileus in susceptible individuals. Persistent vomiting or diarrhea can lead to dehydration and acute kidney injury, requiring prompt medical attention and temporary medication discontinuation.
Semaglutide is not recommended for patients with severe gastroparesis and may affect the absorption of oral medications due to delayed gastric emptying. This is particularly important for Rybelsus (oral semaglutide), which requires specific administration timing.
For patients with ulcerative colitis, the challenge lies in distinguishing these medication-related effects from symptoms of underlying disease activity. New-onset bloody diarrhea, severe abdominal pain, fever, or significant changes in bowel patterns should prompt evaluation for UC flare rather than being attributed solely to medication side effects.
Patients with inflammatory bowel disease considering semaglutide therapy should engage in comprehensive discussions with their healthcare team, ideally involving both their gastroenterologist and the physician prescribing the medication. Several key topics warrant thorough exploration before initiating treatment.
Current disease status and stability should be the first consideration. Patients should provide detailed information about their UC activity level, recent flare history, current medications, and most recent colonoscopy findings. Those with objective evidence of disease control (normal fecal calprotectin, endoscopic remission) may be better candidates than those with frequent flares or active inflammation. Documentation of objective disease markers helps establish a baseline for monitoring rather than relying on an arbitrary duration of remission.
Symptom monitoring strategies require clear planning. Patients and physicians should establish protocols for distinguishing medication side effects from disease flares. This might include:
Keeping a detailed symptom diary during semaglutide initiation
Establishing thresholds for concerning symptoms (bloody stools, fever, severe pain)
Planning for prompt fecal calprotectin testing or limited sigmoidoscopy if symptoms worsen
Scheduling more frequent follow-up during the first 3-6 months of therapy
Alternative treatment options should be explored. For patients with type 2 diabetes, other medication classes with fewer gastrointestinal effects might be preferable, such as SGLT-2 inhibitors or DPP-4 inhibitors. For weight management, lifestyle interventions, nutritional counseling, or alternative pharmacologic options may be considered based on individual risk-benefit assessment.
Medication interactions and timing deserve attention. While semaglutide does not have major drug-drug interactions with IBD medications, its effect on gastric emptying may alter absorption of oral medications. For Rybelsus (oral semaglutide), patients must take it on an empty stomach with a small amount of water and wait at least 30 minutes before food or other medications. Patients taking oral mesalamine, immunosuppressants, or other time-sensitive medications should discuss optimal timing and monitoring.
Patients should also clarify emergency protocols: whom to contact if symptoms worsen, when to seek urgent care, and criteria for temporarily holding semaglutide (such as during severe gastrointestinal symptoms, dehydration, or hospitalization). Women of childbearing potential should be counseled that Wegovy is contraindicated in pregnancy. Patients with diabetes and retinopathy should discuss ophthalmologic monitoring. This collaborative, proactive approach helps maximize safety while allowing appropriate patients to benefit from semaglutide's metabolic advantages when clinically indicated.
Semaglutide is not contraindicated in ulcerative colitis, but patients with stable, well-controlled disease are better candidates than those with active inflammation. Close coordination between your gastroenterologist and prescribing physician is essential to monitor for symptom changes and distinguish medication side effects from disease flares.
The most common gastrointestinal side effects include nausea (15-44%), diarrhea (8-30%), vomiting (5-24%), and abdominal pain. These effects result from semaglutide's action on GLP-1 receptors throughout the digestive tract and typically improve after 4-8 weeks at a stable dose.
New-onset bloody diarrhea, fever, or severe abdominal pain should prompt evaluation for ulcerative colitis flare rather than being attributed to medication alone. Keeping a detailed symptom diary and using objective markers like fecal calprotectin testing helps distinguish between medication effects and disease activity.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.