LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management. Graves disease, an autoimmune thyroid disorder causing hyperthyroidism, affects approximately 0.5-1% of Americans and often leads to metabolic changes including weight fluctuations. Many patients with controlled Graves disease seek weight management solutions, raising questions about tirzepatide safety in this population. While tirzepatide is not contraindicated in Graves disease, careful consideration of thyroid status, medication interactions, and monitoring requirements is essential. This article examines the clinical considerations, safety profile, and management strategies for patients with Graves disease considering tirzepatide therapy.
Quick Answer: Tirzepatide is not contraindicated in Graves disease, but requires individualized assessment with careful thyroid monitoring and is generally deferred until patients achieve euthyroid status.
Tirzepatide is a novel dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). This medication works by enhancing insulin secretion in a glucose-dependent manner, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways. In the SURMOUNT-1 trial, adults with obesity or overweight without diabetes experienced dose-dependent weight loss, with higher doses achieving approximately 15-20% weight reduction over 72 weeks.
Graves disease is an autoimmune thyroid disorder characterized by excessive thyroid hormone production (hyperthyroidism) due to thyroid-stimulating immunoglobulins that activate the thyroid-stimulating hormone (TSH) receptor. This condition affects approximately 0.5-1% of the US population and is more common in women than men. Symptoms include unintentional weight loss, heat intolerance, tremor, palpitations, anxiety, and in some cases, thyroid eye disease (Graves ophthalmopathy).
The intersection of tirzepatide therapy and Graves disease presents important clinical considerations. Patients with Graves disease often experience metabolic changes including increased basal metabolic rate and weight loss during active hyperthyroidism. When thyroid function is controlled with antithyroid medications, radioactive iodine, or surgery, many patients experience weight gain. This metabolic shift has led some clinicians and patients to consider weight management medications like tirzepatide. While there is limited evidence regarding tirzepatide use specifically in patients with significant thyroid disease (as these patients were typically excluded from pivotal trials), there is no established direct pharmacological interaction between tirzepatide and Graves disease pathophysiology. It's important to note that tirzepatide delays gastric emptying, which may affect absorption of oral medications, including levothyroxine, potentially requiring monitoring and dose adjustments.
There is no absolute contraindication to using tirzepatide in patients with Graves disease according to the FDA prescribing information. The medication's labeled contraindications include personal or family history of medullary thyroid carcinoma (MTC), multiple endocrine neoplasia syndrome type 2 (MEN 2), and serious hypersensitivity to tirzepatide or any of its components. Graves disease is not specifically listed as a contraindication. However, this does not mean tirzepatide is automatically appropriate for all patients with Graves disease.
The decision to prescribe tirzepatide in patients with Graves disease requires careful individualized assessment. Key considerations include the current thyroid status (active hyperthyroidism versus controlled euthyroid state), stability of thyroid function on treatment, presence of complications such as thyroid eye disease or cardiac manifestations, and the patient's overall metabolic health. While not a formal contraindication, clinicians generally defer initiation of tirzepatide until patients with hyperthyroidism are euthyroid, as overlapping symptoms and cardiovascular effects could complicate assessment of medication tolerance and efficacy.
For patients with well-controlled Graves disease who are euthyroid on antithyroid medications or following definitive treatment (radioactive iodine or thyroidectomy), tirzepatide may be considered if there are appropriate indications such as type 2 diabetes or obesity (BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidities). The American Diabetes Association Standards of Care support individualized treatment approaches that consider patient comorbidities and preferences.
Importantly, tirzepatide should not be coadministered with other GLP-1 receptor agonists or other tirzepatide-containing products. Pregnancy and lactation are additional considerations, as tirzepatide has shown embryo-fetal risk in animal studies and is not recommended during pregnancy or breastfeeding. Women of reproductive potential should use effective contraception while taking tirzepatide. Clinicians should engage in shared decision-making discussions with patients, explaining that while there is no official link between tirzepatide and worsening Graves disease, limited specific data exists regarding this patient population.
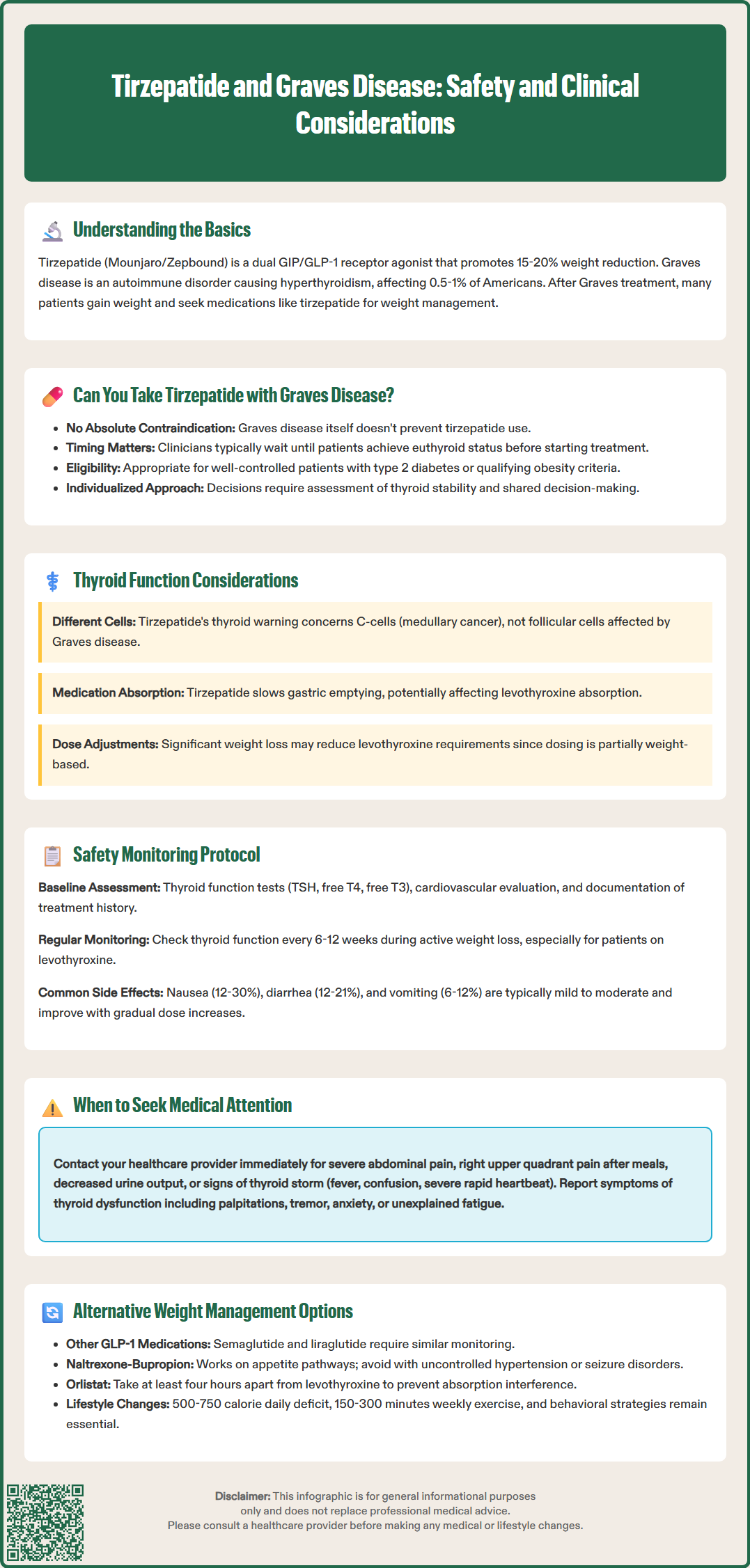
Tirzepatide's prescribing information includes a boxed warning regarding thyroid C-cell tumors, based on rodent studies showing dose-dependent and treatment-duration-dependent increases in thyroid C-cell tumors. However, it is important to note that this concern relates specifically to medullary thyroid carcinoma, which arises from parafollicular C-cells, not the follicular cells affected in Graves disease. The relevance of rodent C-cell tumor findings to humans remains uncertain, and no causal relationship has been established in human clinical trials. Patients should be counseled about symptoms of MTC, including neck mass, dysphagia, dyspnea, or persistent hoarseness, and to seek prompt medical evaluation if these occur. Routine calcitonin screening or thyroid ultrasound is not recommended in the absence of specific risk factors.
Graves disease involves the thyroid follicular cells and TSH receptor activation, representing a fundamentally different pathophysiological process than C-cell proliferation. There is no established mechanism by which GIP/GLP-1 receptor agonism would directly influence autoimmune thyroid disease activity or thyroid-stimulating immunoglobulin production. Clinical trial data for tirzepatide did not identify increased rates of thyroid dysfunction or autoimmune thyroid disease exacerbation, though patients with significant thyroid disease were typically excluded from pivotal trials.
Patients with Graves disease on antithyroid medications (methimazole or propylthiouracil) require regular thyroid function monitoring regardless of tirzepatide use. In accordance with American Thyroid Association guidelines, monitoring should focus on free T4 and T3 levels at 4-6 week intervals during dose titration, as TSH may remain suppressed for weeks to months despite clinical improvement. TSH becomes more useful once the patient is euthyroid and stable. For patients who have undergone radioactive iodine ablation or thyroidectomy and are on levothyroxine replacement, more frequent monitoring (every 6-12 weeks) is advisable during active weight loss, with annual testing once stable.
Clinicians should be aware that significant weight loss from tirzepatide may affect levothyroxine requirements in patients post-ablation or post-thyroidectomy, as thyroid hormone replacement dosing is partially weight-based. Additionally, tirzepatide's effect on gastric emptying may alter levothyroxine absorption. Dose adjustments may be necessary as patients lose weight, emphasizing the importance of continued thyroid function monitoring.
Comprehensive safety monitoring is essential when prescribing tirzepatide to patients with Graves disease. Baseline assessment should include current thyroid status with TSH, free T4, and free T3 levels, documentation of Graves disease treatment history and current management, assessment of thyroid eye disease or other complications, cardiovascular evaluation including heart rate and rhythm (as both hyperthyroidism and GLP-1 receptor agonists can affect heart rate), and standard metabolic parameters including HbA1c, lipid profile, and renal function.
Ongoing monitoring should incorporate thyroid function testing at regular intervals, particularly during the first six months of tirzepatide therapy and during dose escalation. For patients on antithyroid medications, maintain the established monitoring schedule with emphasis on free T4 and T3 levels early in treatment. For patients on levothyroxine replacement, check thyroid function every 6-12 weeks during active weight loss, as significant weight reduction may necessitate dose adjustments. Patients should be educated to report symptoms of thyroid dysfunction, including palpitations, tremor, heat intolerance, anxiety (suggesting hyperthyroidism), or fatigue, cold intolerance, and weight gain (suggesting hypothyroidism). Urgent medical attention is warranted for signs of thyroid storm, including fever, confusion, severe tachycardia, or altered mental status.
According to the FDA prescribing information, common adverse effects of tirzepatide vary by dose and population. In clinical trials, gastrointestinal symptoms were most common, including nausea (12-30%), diarrhea (12-21%), vomiting (6-12%), and constipation (5-17%), with higher rates generally seen at higher doses. These effects are typically mild to moderate and decrease over time. They can be minimized through gradual dose titration. Patients should be counseled about the risk of hypoglycemia, particularly if taking concomitant insulin or sulfonylureas, though tirzepatide's glucose-dependent mechanism reduces this risk compared to older diabetes medications.
Serious adverse effects requiring immediate medical attention include signs of pancreatitis (severe abdominal pain radiating to the back), gallbladder disease (right upper quadrant pain, particularly after meals), acute kidney injury (decreased urine output, swelling), or severe allergic reactions. Tirzepatide is not recommended in patients with a history of pancreatitis or severe gastrointestinal disease, including severe gastroparesis. Patients with diabetes should maintain routine eye care, as rapid glycemic improvement may transiently affect diabetic retinopathy. Patients with a history of thyroid eye disease should be monitored closely for any worsening of ocular symptoms, though there is no established link between tirzepatide and ophthalmopathy progression.
For patients with Graves disease who are not suitable candidates for tirzepatide or prefer alternative approaches, several evidence-based weight management options exist. Other GLP-1 receptor agonists include semaglutide (Wegovy for weight management, Ozempic for diabetes) and liraglutide (Saxenda for weight management, Victoza for diabetes), with semaglutide 2.4 mg demonstrating greater average weight loss than liraglutide 3.0 mg in clinical trials. These medications share the same contraindications regarding medullary thyroid carcinoma and MEN 2 and require similar monitoring.
Non-incretin-based pharmacological options include naltrexone-bupropion (Contrave), which acts on central nervous system pathways regulating appetite and reward. Key contraindications for naltrexone-bupropion include uncontrolled hypertension, seizure disorders, and use of monoamine oxidase inhibitors. Importantly, phentermine and phentermine-topiramate extended-release (Qsymia) are contraindicated in hyperthyroidism and should be avoided in patients with active Graves disease, as they may worsen tachycardia and other sympathomimetic effects. Orlistat (Xenical, Alli) reduces dietary fat absorption and may be considered, though it can interfere with levothyroxine absorption if taken concurrently; patients should separate administration by at least four hours and consider fat-soluble vitamin supplementation. Most weight management medications are contraindicated during pregnancy.
Comprehensive lifestyle modification remains the foundation of weight management for all patients, including those with Graves disease. Evidence-based approaches include structured dietary interventions such as calorie reduction (500-750 kcal/day deficit), Mediterranean or DASH dietary patterns, and portion control strategies. Physical activity recommendations include at least 150 minutes of moderate-intensity aerobic activity weekly, with progression to 200-300 minutes for weight loss maintenance, plus resistance training twice weekly. Behavioral interventions including cognitive behavioral therapy, self-monitoring of food intake and weight, and structured weight loss programs have demonstrated efficacy.
For patients with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) who have not achieved adequate weight loss with lifestyle and pharmacological interventions, bariatric surgery may be considered. Procedures such as sleeve gastrectomy or Roux-en-Y gastric bypass have shown substantial long-term weight loss and metabolic benefits. Patients with Graves disease should have stable, controlled thyroid function before undergoing elective bariatric surgery, and endocrinology consultation is recommended for perioperative management.
Tirzepatide is not contraindicated in Graves disease, but requires individualized assessment. Clinicians generally recommend achieving stable euthyroid status before initiating therapy, with regular thyroid function monitoring throughout treatment.
Tirzepatide does not directly affect Graves disease pathophysiology, but may alter levothyroxine absorption due to delayed gastric emptying. Significant weight loss may also necessitate levothyroxine dose adjustments in patients on thyroid hormone replacement.
Patients should have thyroid function tests (TSH, free T4, free T3) checked every 6-12 weeks during active weight loss, with continued monitoring per established schedules for antithyroid medication or levothyroxine replacement therapy.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.