LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management, but concerns about tirzepatide and thyroid nodules have emerged from animal studies showing thyroid C-cell tumors in rodents. While the FDA includes a boxed warning about potential thyroid cancer risk, clinical trials involving over 10,000 participants have not demonstrated increased thyroid nodule or cancer incidence in humans. Understanding the evidence, contraindications, and monitoring recommendations is essential for patients and clinicians considering this medication. This article examines the relationship between tirzepatide and thyroid health, clarifying when the medication should be avoided and what precautions are necessary.
Quick Answer: Tirzepatide carries an FDA boxed warning for thyroid C-cell tumors based on rodent studies, but clinical trials have not shown increased thyroid nodule or cancer risk in humans over two years of treatment.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management as an adjunct to reduced-calorie diet and increased physical activity), tirzepatide represents the first dual incretin receptor agonist available in clinical practice.
The medication works by simultaneously activating both GIP and GLP-1 receptors, which are naturally occurring hormones involved in glucose regulation and appetite control. When blood glucose levels rise after eating, tirzepatide stimulates insulin secretion from pancreatic beta cells while suppressing inappropriate glucagon release. This dual mechanism enhances glycemic control more effectively than single-receptor agonists. Additionally, tirzepatide slows gastric emptying and acts on central nervous system pathways to reduce appetite and food intake, contributing to significant weight loss in clinical trials.
Tirzepatide is administered as a once-weekly subcutaneous injection, with doses ranging from 2.5 mg to 15 mg depending on the indication and patient tolerance. The medication is metabolized by proteolytic cleavage with metabolites eliminated via urine and feces, and has a half-life of approximately five days. No dosage adjustment is required in renal impairment, including end-stage renal disease. Clinical trials have demonstrated substantial reductions in hemoglobin A1c (up to 2.5% reduction) and body weight (up to 20% reduction) compared to placebo and active comparators. Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, which typically diminish over time with continued use and gradual dose escalation.
Importantly, tirzepatide may reduce oral contraceptive absorption; patients should be advised to use nonoral or backup contraception for 4 weeks after initiation and after each dose escalation.
Thyroid nodules are discrete lesions within the thyroid gland that are distinct from surrounding thyroid tissue. These nodules are remarkably common in the general population, with prevalence estimates ranging from 20% to 76% depending on the detection method used. Palpable nodules occur in approximately 5% of women and 1% of men living in iodine-sufficient regions, while high-resolution ultrasound can detect nodules in up to half of adults over age 60.
The vast majority of thyroid nodules—approximately 90% to 95%—are benign. Common benign etiologies include colloid nodules, follicular adenomas, and hyperplastic nodules. Malignant nodules account for only 5% to 10% of all thyroid nodules, with papillary thyroid carcinoma being the most common histologic type. Most thyroid nodules are asymptomatic and discovered incidentally during physical examination or imaging studies performed for unrelated reasons. Larger nodules may occasionally cause compressive symptoms such as difficulty swallowing, a sensation of pressure in the neck, or hoarseness if they affect the recurrent laryngeal nerve.
Risk factors for thyroid nodules include female sex, increasing age, radiation exposure to the head and neck during childhood, and iodine deficiency (though this is less common in the United States). Family history of thyroid disease and certain genetic syndromes also increase risk. The clinical significance of a thyroid nodule depends on its size, ultrasound characteristics, and the patient's individual risk factors for malignancy.
Standard evaluation of thyroid nodules in the US includes thyroid-stimulating hormone (TSH) testing, high-quality thyroid ultrasound with risk stratification, and fine-needle aspiration (FNA) biopsy based on size and ultrasound risk features. If TSH is suppressed, a radionuclide uptake scan may be considered. Referral to an endocrinologist is typically warranted for suspicious ultrasound features, rapid nodule growth, compressive symptoms, or abnormal cervical lymph nodes. Most small, benign-appearing nodules require only periodic surveillance.
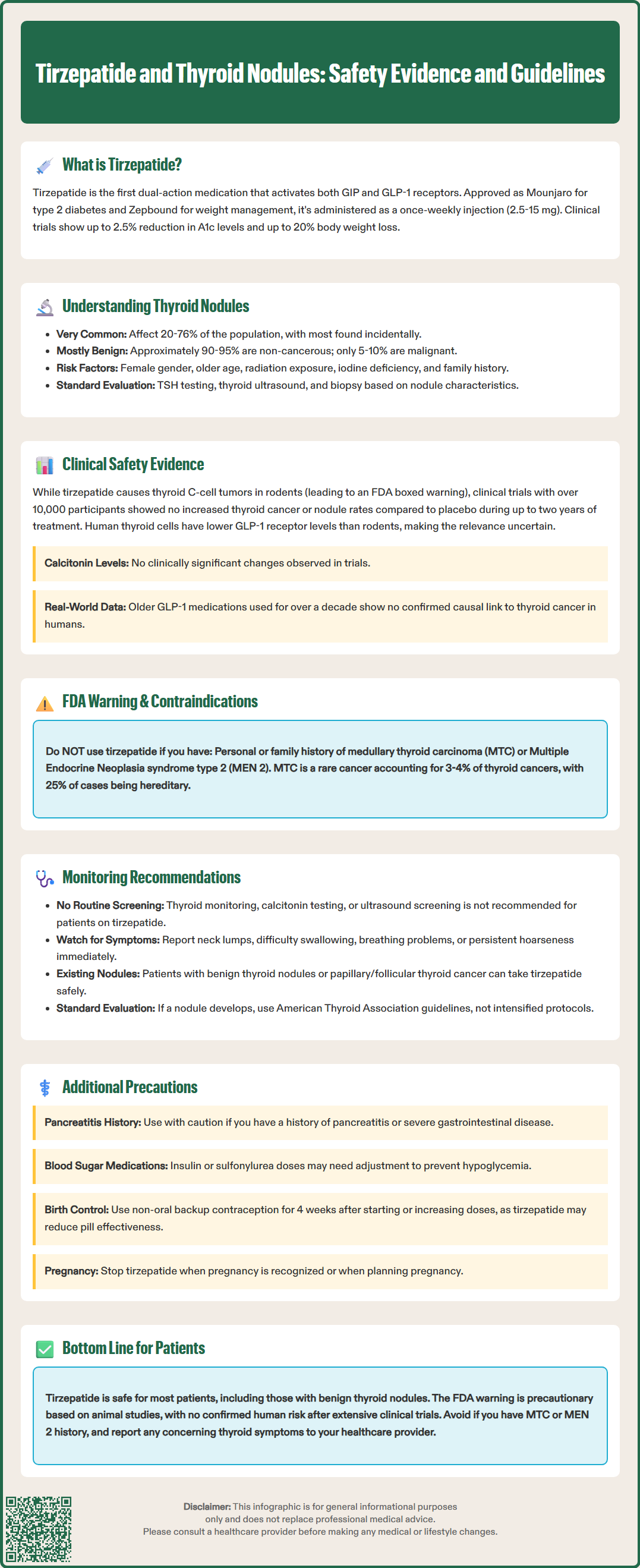
The relationship between tirzepatide and thyroid nodules has been a subject of careful scrutiny due to findings in preclinical animal studies. In rodent toxicology studies, tirzepatide and other GLP-1 receptor agonists have been associated with dose-dependent and treatment-duration-dependent thyroid C-cell tumors, including medullary thyroid carcinoma (MTC). These findings led to a boxed warning in the FDA prescribing information for tirzepatide and related medications. However, it is important to note that the relevance of these animal findings to human risk remains uncertain.
Human thyroid C-cells appear to express GLP-1 receptors at lower levels than rodent C-cells, suggesting that humans may be less susceptible to GLP-1-mediated thyroid proliferation, though evidence on receptor expression varies. Clinical trials of tirzepatide, including the SURPASS and SURMOUNT programs involving over 10,000 participants, have not demonstrated a signal for increased incidence of thyroid cancer or thyroid nodules compared to placebo or active comparators during treatment periods up to two years. However, these trials were not specifically powered to detect rare cancers and had limited follow-up duration. Serum calcitonin levels, a biomarker for C-cell activity, showed no clinically meaningful changes in these trials.
Postmarketing surveillance data and real-world evidence from GLP-1 receptor agonists that have been available for over a decade (such as liraglutide and exenatide) have yielded mixed results. While several observational studies have found no association between GLP-1 receptor agonist use and thyroid malignancy, others have reported potential signals. No causal relationship has been established in humans to date. The FDA boxed warning remains in place as a precautionary measure, reflecting the uncertainty about long-term human risk.
The FDA-approved prescribing information for tirzepatide contains a boxed warning—the most serious type of warning—regarding the risk of thyroid C-cell tumors. This warning states that tirzepatide causes thyroid C-cell tumors at clinically relevant exposures in rodents and that it is unknown whether tirzepatide causes thyroid C-cell tumors, including medullary thyroid carcinoma, in humans. The boxed warning specifically contraindicates tirzepatide use in patients with a personal or family history of medullary thyroid carcinoma or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
Medullary thyroid carcinoma is a rare form of thyroid cancer arising from parafollicular C-cells, accounting for approximately 3% to 4% of all thyroid cancers. Unlike the more common papillary and follicular thyroid cancers, MTC can be hereditary in about 25% of cases, often associated with MEN 2 syndrome. The theoretical concern with GLP-1 receptor agonists stems from the presence of GLP-1 receptors on thyroid C-cells, which could potentially stimulate proliferation and neoplastic transformation.
Healthcare providers are advised to inform patients about the potential risk of thyroid tumors when prescribing tirzepatide and to counsel them on symptoms that might suggest thyroid cancer, including a neck mass, dysphagia, dyspnea, or persistent hoarseness. Patients should be instructed to report these symptoms promptly. While routine calcitonin monitoring is not recommended, if serum calcitonin is measured and found to be markedly elevated (e.g., >50 ng/L), further evaluation is indicated. It is important to emphasize that there is no established causal link between tirzepatide and thyroid cancer in humans, and the warning is based primarily on animal data. The American Diabetes Association and other professional organizations acknowledge that the clinical significance of rodent C-cell findings for human risk remains unclear.
Current FDA labeling and clinical guidelines do not require routine thyroid monitoring or screening for patients taking tirzepatide who do not have specific risk factors. Routine measurement of serum calcitonin or thyroid ultrasound surveillance is not recommended for the general population of patients prescribed tirzepatide, as these screening approaches have poor positive predictive value and may lead to unnecessary interventions in patients with benign findings. This aligns with the US Preventive Services Task Force recommendation against thyroid cancer screening in asymptomatic adults.
Before initiating tirzepatide, clinicians should obtain a thorough personal and family history focusing on thyroid disease, particularly any history of medullary thyroid carcinoma or MEN 2 syndrome. Patients with a personal history of MTC or a family history of MTC or MEN 2 should not receive tirzepatide. For patients with a history of benign thyroid nodules or papillary/follicular thyroid cancer, tirzepatide is not contraindicated, though individualized risk-benefit assessment is appropriate.
Patients should be educated about symptoms that warrant medical evaluation, including the development of a neck lump or swelling, difficulty swallowing, shortness of breath, or persistent hoarseness. These symptoms should prompt clinical examination and appropriate diagnostic workup, which may include thyroid ultrasound and, if indicated, fine-needle aspiration biopsy. If a patient develops a thyroid nodule while taking tirzepatide, evaluation should follow standard American Thyroid Association guidelines, including TSH testing, ultrasound risk stratification, and FNA based on size and risk features.
If calcitonin is measured and found to be elevated (>50 ng/L), further evaluation is warranted. For patients already under surveillance for pre-existing benign thyroid nodules, continuation of their established monitoring schedule is appropriate. There is no evidence to suggest that more intensive surveillance is needed for patients taking tirzepatide. Healthcare providers should maintain open communication with patients about the theoretical thyroid risks while emphasizing the substantial metabolic benefits of tirzepatide and the absence of an established causal relationship to thyroid cancer in humans.
Tirzepatide is absolutely contraindicated in patients with a personal or family history of medullary thyroid carcinoma and in patients with Multiple Endocrine Neoplasia syndrome type 2. These contraindications are based on the theoretical risk suggested by animal studies and the known genetic predisposition to MTC in these populations. Clinicians should specifically inquire about family history of thyroid cancer and MEN 2 before prescribing tirzepatide.
Additional contraindications include a history of serious hypersensitivity reactions to tirzepatide or any of its components. Patients who have experienced anaphylaxis or angioedema with tirzepatide should not be rechallenged with the medication. Tirzepatide should be used with caution in patients with a history of pancreatitis, as GLP-1 receptor agonists have been associated with acute pancreatitis in postmarketing reports. While causality has not been definitively established, patients with a history of pancreatitis should be informed of this potential risk, and alternative therapies should be considered.
Tirzepatide is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis. Patients with diabetic retinopathy should be monitored closely, as rapid improvement in glycemic control has been associated with temporary worsening of diabetic retinopathy. There is also a risk of hypoglycemia when tirzepatide is used with insulin or sulfonylureas; consider dose reduction of these agents when initiating tirzepatide. Patients should be informed about the risk of gallbladder disease and advised to report symptoms suggestive of gallstones.
Regarding pregnancy, tirzepatide should be discontinued when pregnancy is recognized. Women planning pregnancy should consider stopping tirzepatide in advance according to the FDA-specified interval due to its long washout period. The medication is not recommended during pregnancy or breastfeeding. Tirzepatide may reduce oral contraceptive absorption; patients should use nonoral or backup contraception for 4 weeks after initiation and after each dose escalation.
No dosage adjustment is required for patients with renal impairment, including end-stage renal disease, though renal function should be monitored if severe gastrointestinal adverse effects occur. Healthcare providers should engage in shared decision-making with patients, discussing the substantial metabolic benefits of tirzepatide alongside the theoretical thyroid risks, to determine whether the medication is appropriate for each individual's clinical situation and risk profile.
Tirzepatide is not contraindicated for patients with benign thyroid nodules or common thyroid cancers (papillary or follicular). However, it should not be used if you have a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
No causal relationship between tirzepatide and thyroid cancer has been established in humans. While rodent studies showed thyroid C-cell tumors, clinical trials with over 10,000 participants found no increased thyroid cancer incidence during treatment periods up to two years.
Routine thyroid monitoring or calcitonin screening is not recommended for patients without specific risk factors. Patients should report symptoms such as neck lumps, difficulty swallowing, or persistent hoarseness, which warrant standard thyroid evaluation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.