LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) is a dual GIP/GLP-1 receptor agonist that has transformed metabolic disease treatment. While highly effective for glycemic control and weight reduction, some patients report hair thinning during treatment. Alopecia is listed as an adverse reaction in FDA prescribing information, with clinical trial data showing increased rates compared to placebo. However, distinguishing between medication effects and hair loss triggered by rapid weight loss itself remains challenging. Understanding the relationship between tirzepatide and hair loss helps patients and clinicians make informed treatment decisions and implement preventive strategies.
Quick Answer: Alopecia is listed as an adverse reaction to tirzepatide in FDA prescribing information, with clinical trials showing increased hair loss rates compared to placebo, though this may relate to rapid weight loss rather than direct drug effects.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus under the brand name Mounjaro, and for chronic weight management as Zepbound. For weight management, Zepbound is indicated for adults with a BMI ≥30 kg/m² (obesity) or ≥27 kg/m² (overweight) with at least one weight-related comorbidity. This dual-action mechanism distinguishes tirzepatide from other medications in its class.
The medication works by mimicking two naturally occurring incretin hormones that play crucial roles in glucose metabolism and appetite regulation. By activating both GIP and GLP-1 receptors, tirzepatide enhances insulin secretion in a glucose-dependent manner, meaning it stimulates insulin release only when blood glucose levels are elevated. This mechanism reduces the risk of hypoglycemia when used alone, though the risk increases significantly when combined with insulin or sulfonylureas. Additionally, tirzepatide suppresses glucagon secretion, slows gastric emptying, and reduces appetite through central nervous system pathways.
Clinical trials have demonstrated that tirzepatide produces substantial improvements in glycemic control, with HbA1c reductions of 1.9% to 2.4% depending on the dose in the SURPASS trials. The medication has also shown remarkable efficacy for weight loss in the SURMOUNT trials, with patients losing approximately 15% to 22% of their body weight at the highest doses. These significant metabolic effects have made tirzepatide an important therapeutic option for patients with type 2 diabetes, particularly those who are overweight or obese.
Tirzepatide is administered as a once-weekly subcutaneous injection, with doses typically starting at 2.5 mg for 4 weeks and gradually titrated upward in 2.5 mg increments to minimize gastrointestinal side effects. The maximum approved dose is 15 mg weekly for both diabetes management and weight loss indications.
Important safety information includes a boxed warning for thyroid C-cell tumors (contraindicated in patients with personal/family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2), and warnings for pancreatitis, gallbladder disease, acute kidney injury risk, diabetic retinopathy complications, and suicidal behavior/ideation (for the weight management indication).
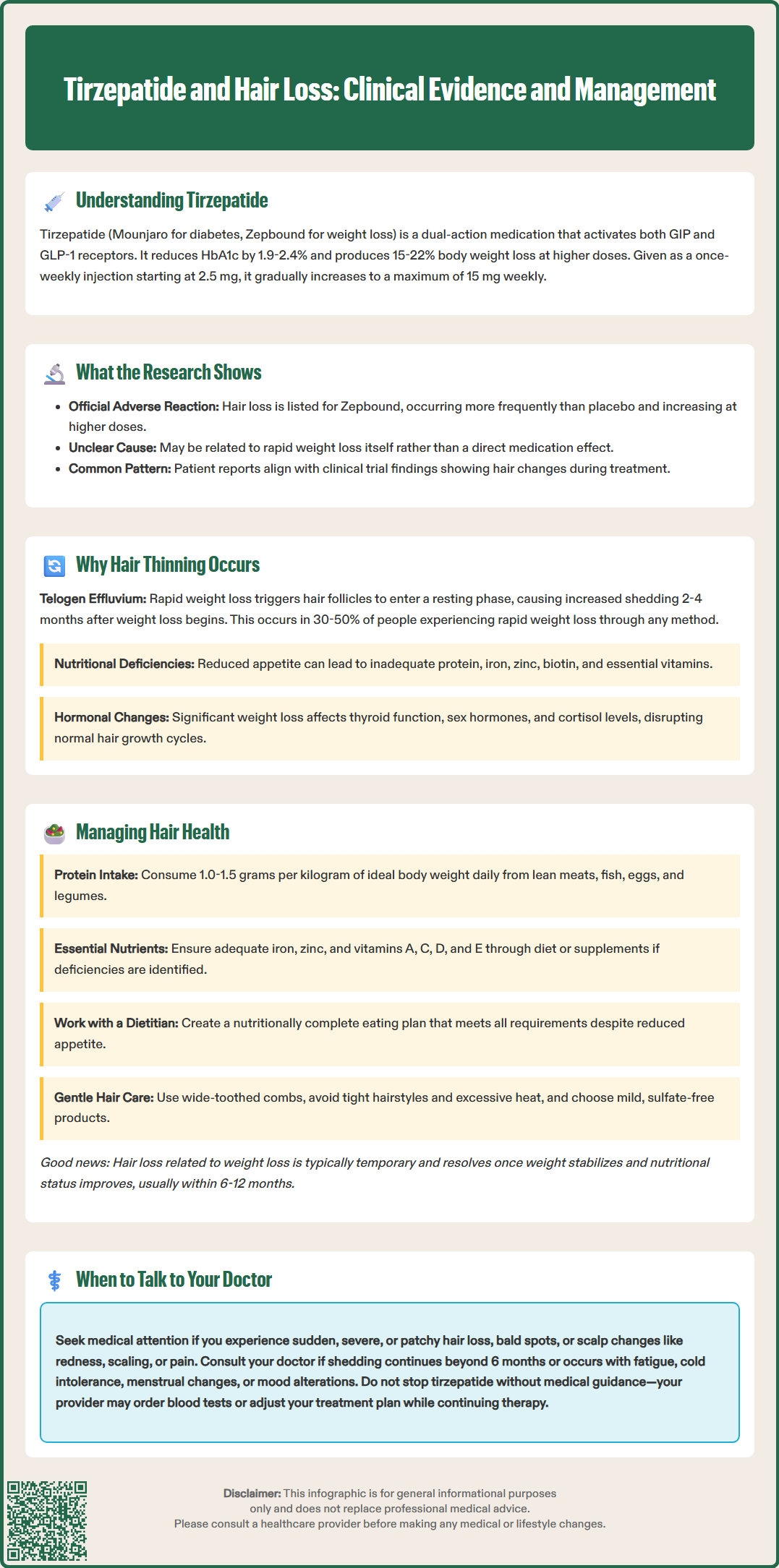
Alopecia (hair loss) is listed as an adverse reaction in the FDA-approved prescribing information for Zepbound (tirzepatide for chronic weight management). In clinical trials, hair loss was reported more frequently with tirzepatide than with placebo, with rates appearing to increase at higher doses. This finding suggests a possible association between tirzepatide treatment and hair loss, though the exact mechanism remains unclear and may be related to the rapid weight loss rather than a direct drug effect.
Anecdotal reports from patients taking tirzepatide have also emerged on social media platforms and patient forums describing experiences with hair thinning or increased shedding. While these reports align with clinical trial observations, it's important to distinguish between temporal association (events occurring around the same time) and true causality, which requires rigorous investigation.
The most common adverse effects documented in tirzepatide clinical trials are gastrointestinal in nature, including nausea, diarrhea, vomiting, constipation, and abdominal discomfort. These effects are generally mild to moderate and tend to diminish over time as the body adjusts to the medication. Other documented side effects include injection site reactions, fatigue, and potential increases in heart rate.
Researchers continue to monitor post-marketing surveillance data to identify any adverse effects that may not have been apparent during clinical trials. If you are experiencing hair changes while taking tirzepatide, it is essential to discuss this with your healthcare provider, who can help determine whether the medication, rapid weight loss, nutritional factors, or other underlying conditions may be contributing to the issue. Your doctor may also report such effects to the FDA's MedWatch program to contribute to ongoing safety monitoring.
While tirzepatide may be associated with hair loss as reported in clinical trials, the substantial weight loss it produces can trigger a well-recognized condition called telogen effluvium. This temporary form of hair shedding occurs when a significant proportion of hair follicles prematurely enter the resting (telogen) phase of the hair growth cycle, resulting in increased shedding approximately two to four months after the triggering event.
Rapid or significant weight loss is a known trigger for telogen effluvium, regardless of the method used to achieve that weight loss—whether through medication, bariatric surgery, or intensive dietary restriction. When the body experiences substantial metabolic changes or perceives physiological stress, it may temporarily redirect resources away from non-essential functions like hair growth. Studies of patients undergoing bariatric surgery have documented hair loss in 30% to 50% of cases, typically occurring several months post-procedure and resolving within six to twelve months.
Nutritional deficiencies commonly associated with rapid weight loss can also contribute to hair thinning. Inadequate intake of protein, iron, zinc, biotin, and essential vitamins can compromise hair follicle health and growth. Patients taking tirzepatide may experience reduced appetite and food intake, potentially leading to insufficient consumption of these critical nutrients if dietary choices are not carefully managed. Iron deficiency, in particular, is strongly associated with hair loss and is more common in individuals with restricted caloric intake.
Additionally, the physiological stress of significant metabolic changes, alterations in hormone levels associated with weight loss (including changes in thyroid function, sex hormones, and cortisol), and the body's adaptation to a new metabolic state can all influence hair growth cycles. Understanding these mechanisms helps contextualize why hair changes might occur during treatment with weight loss medications like tirzepatide, even if the medication itself is not directly affecting hair follicles.
If you are taking tirzepatide and concerned about hair health, several proactive strategies can help minimize the risk of hair thinning and support optimal hair growth. Nutritional optimization is paramount, particularly given the appetite-suppressing effects of the medication. Focus on consuming adequate protein—aim for 1.0 to 1.5 grams per kilogram of ideal body weight daily, which may be higher than standard recommendations during active weight loss. High-quality protein sources include lean meats, fish, eggs, dairy products, legumes, and plant-based proteins.
Ensure sufficient intake of micronutrients essential for hair health. Key nutrients include iron (found in red meat, spinach, and fortified cereals), zinc (present in shellfish, meat, and seeds), and vitamins A, C, D, and E. While biotin (in eggs, nuts, and whole grains) is often promoted for hair health, there is limited evidence supporting routine supplementation unless a deficiency is documented. Additionally, high-dose biotin supplements can interfere with certain laboratory tests, including thyroid and cardiac markers, so inform your healthcare provider if you're taking biotin supplements.
Consider working with a registered dietitian nutritionist (RDN) who specializes in weight management to develop a nutritionally complete eating plan that accommodates reduced appetite while meeting all nutritional requirements. Your healthcare provider may recommend laboratory testing to assess for deficiencies in iron (ferritin, serum iron, total iron-binding capacity), vitamin D, vitamin B12, and thyroid function.
Supplementation may be appropriate if dietary intake is insufficient or deficiencies are identified. A comprehensive multivitamin formulated for individuals undergoing weight loss can provide baseline nutritional insurance. However, avoid mega-dosing individual supplements without medical guidance, as excessive intake of certain nutrients (particularly fat-soluble vitamins like vitamin A) can paradoxically contribute to hair loss or other adverse effects.
Gentle hair care practices can minimize mechanical stress on hair follicles during periods of increased shedding. Use a wide-toothed comb, avoid tight hairstyles that create tension on the scalp, limit heat styling, and choose mild, sulfate-free hair care products. Adequate hydration, stress management techniques, and sufficient sleep also support overall physiological health and may help mitigate hair shedding. Remember that if hair loss is related to telogen effluvium from weight loss, it is typically temporary and self-resolving once weight stabilizes and nutritional status is optimized.
While some degree of hair shedding during significant weight loss may be expected and temporary, certain circumstances warrant prompt medical evaluation. Schedule an appointment with your healthcare provider if you experience sudden or severe hair loss, particularly if it occurs in patches (which may suggest alopecia areata or other dermatological conditions), if you notice bald spots, or if hair loss is accompanied by scalp changes such as redness, scaling, itching, or pain. Hair shedding that persists beyond 6 months or worsens despite stabilized weight also merits evaluation.
Additional concerning symptoms that should prompt medical consultation include hair loss associated with other systemic symptoms such as unexplained fatigue, cold intolerance, changes in menstrual patterns, unintended weight changes beyond expected medication effects, or mood alterations. These symptoms may indicate underlying conditions such as thyroid disorders, hormonal imbalances, or autoimmune diseases that require specific diagnosis and treatment. Your doctor can perform a comprehensive evaluation including detailed medical history, physical examination of the scalp and hair, and appropriate laboratory investigations.
Blood tests that may be ordered include complete blood count (to assess for anemia), comprehensive metabolic panel, thyroid function tests (TSH, free T4), ferritin and iron studies, vitamin D and B12 levels, and potentially hormone panels depending on clinical suspicion. In some cases, referral to a dermatologist may be appropriate for specialized evaluation, particularly if the pattern or characteristics of hair loss are atypical, scarring is present, or hair loss persists despite addressing nutritional and metabolic factors.
It is important to maintain open communication with your healthcare team about all side effects or concerns you experience while taking tirzepatide. Do not discontinue the medication without medical guidance, as abrupt cessation could adversely affect your diabetes control or weight management goals. Your doctor can help determine whether hair changes are related to the medication, the weight loss process, nutritional factors, or an unrelated condition, and can develop an appropriate management plan. If hair loss is determined to be related to rapid weight loss rather than a direct medication effect, your provider may recommend adjusting the pace of weight loss, optimizing nutrition, or implementing other supportive measures while continuing treatment.
Alopecia is listed in FDA prescribing information as an adverse reaction, with clinical trials showing increased rates compared to placebo. However, the mechanism remains unclear and may be related to rapid weight loss triggering telogen effluvium rather than direct drug effects on hair follicles.
If hair loss is related to weight-loss-induced telogen effluvium, shedding typically begins 2-4 months after starting treatment and resolves within 6-12 months once weight stabilizes and nutritional status is optimized. Persistent hair loss beyond 6 months warrants medical evaluation.
Optimize protein intake (1.0-1.5 g/kg ideal body weight daily), ensure adequate iron, zinc, and vitamin intake, consider working with a registered dietitian, and have your healthcare provider check for nutritional deficiencies through laboratory testing. Gentle hair care practices and avoiding tight hairstyles also help minimize mechanical stress.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.