LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist approved for type 2 diabetes and weight management, raising questions about its effects on eye health. Macular degeneration, the leading cause of vision loss in older adults, shares risk factors with metabolic conditions tirzepatide treats. While clinical trials have not identified a direct link between tirzepatide and macular degeneration, understanding potential ocular effects remains important for comprehensive patient care. This article examines current evidence on tirzepatide's relationship with macular degeneration, monitoring recommendations, and considerations for patients with existing eye conditions.
Quick Answer: Current clinical evidence does not show a direct link between tirzepatide use and macular degeneration development or progression.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight loss), tirzepatide represents a significant advancement in metabolic disease management due to its dual incretin receptor activity.
The medication works through multiple complementary mechanisms. By activating both GIP and GLP-1 receptors, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. These actions collectively improve glycemic control in patients with type 2 diabetes. Additionally, tirzepatide acts on central appetite regulation pathways, leading to reduced caloric intake and substantial weight loss—with clinical trials showing approximately 15-20% weight reduction in obesity (SURMOUNT-1) and somewhat smaller reductions in diabetes trials.
Tirzepatide is administered as a once-weekly subcutaneous injection, starting at 2.5 mg for 4 weeks as an initiation dose before titrating to maintenance doses of 5-15 mg depending on the indication and patient tolerance. In head-to-head trials, tirzepatide demonstrated greater efficacy in glycemic control and weight reduction compared to semaglutide 1 mg (SURPASS-2). Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, which typically diminish over time with dose titration.
Important safety considerations include a boxed warning for thyroid C-cell tumors (contraindicated in patients with personal/family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2), and warnings for pancreatitis, gallbladder disease, acute kidney injury, and severe gastrointestinal disease. Tirzepatide may also reduce the effectiveness of oral contraceptives due to delayed gastric emptying.
Given the growing prevalence of type 2 diabetes and obesity in the United States, tirzepatide has become an important therapeutic option for millions of patients. However, as with any medication affecting metabolic pathways, understanding its potential effects on various organ systems—including the eyes—remains an important consideration for comprehensive patient care.
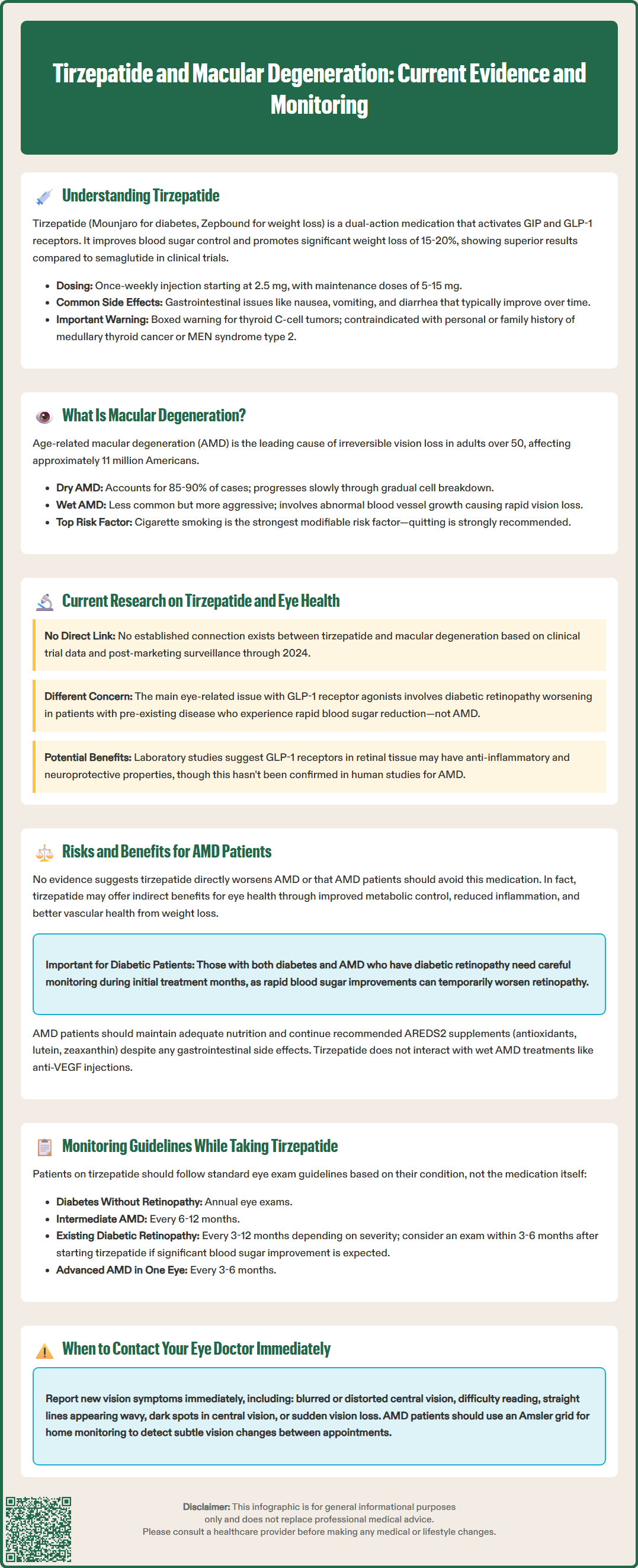
Macular degeneration, formally known as age-related macular degeneration (AMD), is a progressive eye condition affecting the macula—the central portion of the retina responsible for sharp, detailed central vision. AMD is the leading cause of irreversible vision loss in adults over 50 years of age in the United States, affecting approximately 11 million Americans according to the National Eye Institute (NEI), with prevalence expected to increase as the population ages.
There are two primary forms of AMD: dry (atrophic) and wet (neovascular or exudative). Dry AMD accounts for approximately 85-90% of cases and involves the gradual breakdown of light-sensitive cells in the macula, along with the accumulation of drusen (yellowish deposits beneath the retina). This form typically progresses slowly over years. Wet AMD, though less common, is more aggressive and involves abnormal blood vessel growth beneath the retina (choroidal neovascularization), which can leak fluid or blood, causing rapid and severe vision loss if untreated.
Several risk factors increase the likelihood of developing AMD. Non-modifiable risk factors include advancing age (particularly over 60 years), Caucasian ethnicity, family history of AMD, and genetic variants in complement pathway genes. Modifiable risk factors include cigarette smoking (the strongest modifiable risk factor, with smoking cessation strongly recommended), hypertension, cardiovascular disease, and potentially obesity. Dietary factors have been studied, with observational studies suggesting benefits from diets rich in antioxidants and green leafy vegetables. However, it's important to note that while the AREDS2 supplement formulation has been shown to reduce progression in intermediate to advanced AMD, omega-3 fatty acid supplementation did not demonstrate benefit in this randomized trial.
The relationship between diabetes and AMD is complex. While diabetes primarily causes diabetic retinopathy—a distinct microvascular complication—some epidemiological studies suggest diabetes may also influence AMD risk through shared pathophysiological mechanisms including chronic inflammation, oxidative stress, and endothelial dysfunction. This potential overlap makes understanding the ocular effects of diabetes medications particularly relevant for comprehensive patient management.
As of 2024, there is no established direct link between tirzepatide and macular degeneration based on available clinical trial data and post-marketing surveillance. The pivotal clinical trials for tirzepatide (SURPASS program for diabetes and SURMOUNT program for obesity) did not identify AMD as a specific adverse event of concern. However, research into the broader effects of incretin-based therapies on retinal health continues to evolve.
The primary ocular concern with GLP-1 receptor agonists has centered on diabetic retinopathy rather than macular degeneration. Clinical trials of semaglutide (another GLP-1 agonist) showed a temporary increase in diabetic retinopathy complications, particularly in patients with pre-existing retinopathy who experienced rapid glycemic improvement. This phenomenon, known as "early worsening," is thought to result from rapid reduction in blood glucose levels rather than a direct drug effect. The American Diabetes Association (ADA) Standards of Care notes this concern with rapid glycemic improvement generally, though the current US Prescribing Information for tirzepatide does not contain a specific warning about diabetic retinopathy complications.
Regarding potential protective effects, some preclinical research suggests GLP-1 receptors are expressed in retinal tissue, and GLP-1 agonists may have neuroprotective and anti-inflammatory properties in laboratory studies. Animal studies have shown that GLP-1 receptor activation may reduce retinal inflammation and oxidative stress. However, these findings from nonclinical research have not been translated into clinical evidence specifically addressing AMD prevention or progression in humans.
It is important to note that the weight loss and metabolic improvements achieved with tirzepatide could theoretically influence AMD risk by addressing modifiable risk factors such as obesity and cardiovascular disease. Currently, no dedicated clinical studies have examined tirzepatide's specific effects on AMD incidence or progression, representing an area where further research would be valuable as clinical experience with this medication expands.
For patients with pre-existing macular degeneration who are considering or currently taking tirzepatide for diabetes or weight management, the decision-making process requires careful individualized assessment. Currently, there is no evidence suggesting that tirzepatide directly worsens AMD or that patients with AMD should avoid this medication. However, several considerations merit attention.
Potential indirect benefits may include improved metabolic health, which could theoretically support overall vascular health. Some observational studies have suggested associations between obesity and AMD risk, though this relationship requires further research. Additionally, improved glycemic control in diabetic patients reduces overall microvascular complications, potentially creating a more favorable environment for retinal health. The anti-inflammatory effects associated with weight loss and metabolic improvement may also be beneficial, as chronic inflammation plays a role in AMD pathogenesis.
Potential considerations and risks primarily relate to the known effects on diabetic retinopathy rather than AMD specifically. Patients with concurrent diabetes and AMD who have pre-existing diabetic retinopathy should be monitored carefully, particularly during the initial months of therapy when glycemic changes are most pronounced. Rapid improvement in blood glucose levels, while generally beneficial, may temporarily worsen diabetic retinopathy in susceptible individuals. This "early worsening" phenomenon typically stabilizes with continued therapy but requires co-management with an ophthalmologist to determine appropriate individualized care.
The gastrointestinal side effects of tirzepatide—particularly nausea and vomiting—could theoretically affect nutritional intake. For patients with intermediate or advanced AMD, the American Academy of Ophthalmology and National Eye Institute recommend consideration of AREDS2 formula supplements, which contain specific antioxidants and carotenoids (lutein and zeaxanthin). Patients should be counseled on maintaining adequate nutrition despite appetite suppression.
For patients with wet AMD receiving anti-VEGF injections, there are no known interactions between tirzepatide and intravitreal therapies. Treatment for AMD should proceed according to standard ophthalmologic protocols regardless of tirzepatide use. The decision to initiate or continue tirzepatide should be based on the metabolic benefits and overall risk-benefit profile for each individual patient.
Patients taking tirzepatide should maintain appropriate ophthalmologic surveillance, with monitoring intensity determined by individual risk factors rather than tirzepatide use alone. The American Diabetes Association (ADA) and American Academy of Ophthalmology provide clear guidelines for eye examination frequency in diabetic patients, which should be followed regardless of the specific glucose-lowering medication used.
For patients with diabetes, comprehensive dilated eye examinations should be performed at the time of diabetes diagnosis (for type 2 diabetes) or within five years of diagnosis (for type 1 diabetes). According to the ADA Standards of Care, if no retinopathy is present and glycemic control is good, examinations should occur annually with the option to extend to every 1-2 years following one or more normal eye exams. Patients with any degree of diabetic retinopathy require more frequent monitoring as determined by their ophthalmologist, typically ranging from every 3-12 months depending on severity. When initiating tirzepatide in patients with pre-existing diabetic retinopathy, consideration should be given to ophthalmologic evaluation within 3-6 months if significant glycemic improvement is anticipated, though this represents expert opinion rather than specific guideline recommendations.
For patients with known AMD, monitoring should follow standard ophthalmologic recommendations based on AMD severity and type. According to the American Academy of Ophthalmology Preferred Practice Pattern, patients with intermediate AMD or high-risk features typically require examination every 6-12 months, while those with advanced AMD in one eye require more frequent monitoring (every 3-6 months). Patients with wet AMD receiving anti-VEGF therapy follow individualized treatment and monitoring schedules determined by their retinal specialist.
Patient education is essential for early detection of vision changes. Patients should be counseled to report immediately any new or worsening visual symptoms including:
Blurred or distorted central vision
Difficulty reading or recognizing faces
Straight lines appearing wavy (metamorphopsia)
Dark or empty areas in central vision
Sudden vision loss or floaters
Home monitoring with an Amsler grid can help patients with AMD detect subtle changes in central vision between appointments, as recommended by the NEI and AAO. Healthcare providers prescribing tirzepatide should document baseline eye examination status, ensure patients have established ophthalmologic care, and reinforce the importance of maintaining regular eye examinations as part of comprehensive diabetes and metabolic disease management.
No, current clinical trial data and post-marketing surveillance have not identified a direct link between tirzepatide and macular degeneration development or worsening.
Yes, there is no evidence suggesting patients with AMD should avoid tirzepatide. Treatment decisions should be based on metabolic benefits and overall risk-benefit assessment with your healthcare provider.
Eye exam frequency depends on your individual risk factors rather than tirzepatide use alone. Patients with diabetes should have annual comprehensive dilated eye exams, while those with AMD should follow their ophthalmologist's recommendations based on disease severity.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.