LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide and metformin together represent a powerful, evidence-based combination for managing type 2 diabetes when single-agent therapy fails to achieve glycemic targets. Metformin, a first-line biguanide, reduces hepatic glucose production, while tirzepatide—a dual GIP/GLP-1 receptor agonist approved by the FDA in 2022—enhances insulin secretion, suppresses glucagon, and promotes weight loss. This complementary pairing addresses multiple metabolic defects simultaneously, delivering superior HbA1c reductions and significant weight loss compared to monotherapy. Understanding how these medications work synergistically enables clinicians and patients to make informed treatment decisions aligned with American Diabetes Association guidelines and individual health goals.
Quick Answer: Tirzepatide and metformin together provide complementary diabetes control by targeting different metabolic pathways—metformin reduces hepatic glucose production while tirzepatide enhances insulin secretion and promotes weight loss.
The combination of tirzepatide and metformin represents an evidence-based approach to managing type 2 diabetes mellitus, leveraging complementary mechanisms of action to optimize glycemic control. Tirzepatide is available as Mounjaro® (indicated for type 2 diabetes) and Zepbound® (indicated for chronic weight management). It is a novel dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA in May 2022. Metformin, a biguanide, has been a cornerstone of type 2 diabetes pharmacotherapy for decades, with an established safety profile and extensive clinical experience.
Combination therapy with these agents is commonly employed in clinical practice when glycemic targets are not achieved with initial therapy. The American Diabetes Association (ADA) Standards of Care emphasizes patient-centered treatment selection, recommending consideration of combination therapy when monotherapy does not achieve or maintain glycemic goals (typically hemoglobin A1c [HbA1c] below 7% for most adults) within three months. For patients with HbA1c levels ≥1.5% above their individualized target, initial combination therapy may be appropriate.
This therapeutic approach addresses multiple pathophysiologic defects in type 2 diabetes simultaneously. Metformin primarily reduces hepatic glucose production and improves peripheral insulin sensitivity, while tirzepatide enhances glucose-dependent insulin secretion, suppresses glucagon release, slows gastric emptying, and promotes satiety. The complementary nature of these mechanisms provides additive glycemic benefits while potentially improving cardiovascular and renal risk factors associated with diabetes. Understanding the rationale for combination therapy enables clinicians to make informed treatment decisions aligned with current evidence-based guidelines and individual patient needs.
The pharmacologic synergy between tirzepatide and metformin stems from their distinct yet complementary mechanisms of action targeting different aspects of glucose homeostasis. Metformin's primary mechanism involves activation of AMP-activated protein kinase (AMPK) in hepatocytes, which suppresses gluconeogenesis and significantly reduces hepatic glucose output. Additionally, metformin enhances insulin sensitivity in peripheral tissues, particularly skeletal muscle, improving glucose uptake and utilization. These effects occur without stimulating insulin secretion, thereby minimizing hypoglycemia risk.
Tirzepatide functions as a dual incretin receptor agonist, binding both GIP and GLP-1 receptors with high affinity. Through GLP-1 receptor activation, tirzepatide stimulates glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon secretion from alpha cells, and delays gastric emptying to attenuate postprandial glucose excursions. The GIP receptor component enhances insulin secretion and may contribute to metabolic effects. Importantly, tirzepatide's glucose-dependent mechanism means insulin secretion occurs primarily when blood glucose is elevated, substantially reducing hypoglycemia risk compared to sulfonylureas or insulin.
When combined, these agents address multiple pathophysiologic defects simultaneously: metformin reduces basal hyperglycemia through hepatic mechanisms, while tirzepatide targets postprandial glucose elevations and promotes weight loss through central appetite regulation. The combination does not create significant pharmacokinetic interactions, as metformin is not metabolized hepatically and tirzepatide undergoes proteolytic degradation. This complementary action enables greater HbA1c reductions than either agent alone, with clinical trials demonstrating additive effects on glycemic control.
Clinically important, tirzepatide's effect on delaying gastric emptying may reduce the absorption of oral medications, including oral contraceptives. Patients using oral contraceptives should be advised to switch to a non-oral method or add a barrier method for 4 weeks after tirzepatide initiation and after each dose increase.
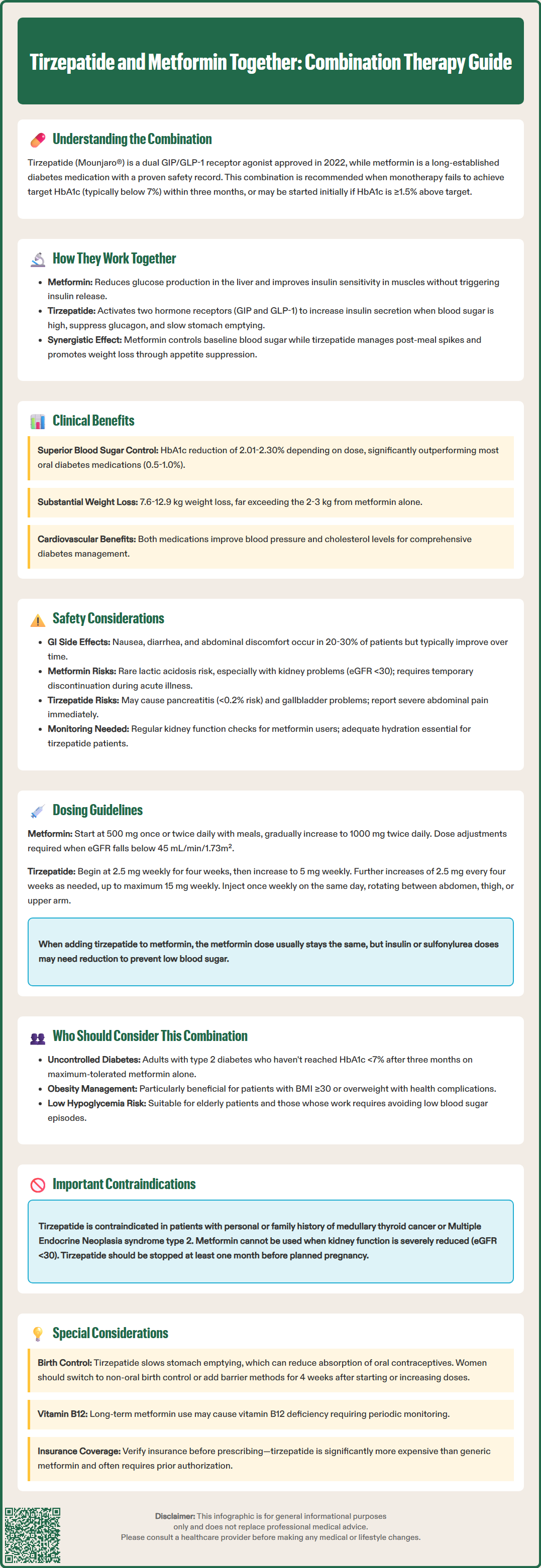
Clinical trial evidence demonstrates substantial benefits when tirzepatide is added to metformin therapy in patients with inadequate glycemic control. The pivotal SURPASS clinical trial program evaluated tirzepatide in various combinations, including with metformin. In SURPASS-2, which compared tirzepatide to semaglutide (a GLP-1 receptor agonist) in patients taking metformin, tirzepatide 5 mg, 10 mg, and 15 mg doses achieved mean HbA1c reductions of 2.01%, 2.24%, and 2.30% respectively from baseline, compared to 1.86% with semaglutide 1 mg. These reductions substantially exceeded the typical 0.5-1.0% decrease expected from adding most oral antidiabetic agents.
Beyond glycemic control, the combination offers significant weight reduction benefits. In SURPASS trials, patients receiving tirzepatide with metformin experienced mean weight loss ranging from 7.6 kg to 12.9 kg depending on tirzepatide dose, compared to baseline. This weight reduction addresses a critical component of type 2 diabetes pathophysiology, as obesity contributes to insulin resistance and beta-cell dysfunction. The weight loss observed with this combination exceeds that typically achieved with metformin alone (approximately 2-3 kg) or lifestyle modification.
Cardiovascular and metabolic benefits represent additional advantages of this combination. Both agents demonstrate favorable effects on cardiovascular risk factors, including blood pressure reduction and lipid profile improvement. Metformin has shown potential cardiovascular benefits in observational studies, while tirzepatide has demonstrated improvements in blood pressure and markers of cardiovascular risk in clinical trials. The SURPASS-CVOT trial, evaluating cardiovascular outcomes with tirzepatide, is ongoing. Until these results are available, GLP-1 receptor agonists with established cardiovascular benefits (liraglutide, semaglutide, dulaglutide) are preferred by ADA guidelines for patients with established atherosclerotic cardiovascular disease. Current evidence supports this combination as an effective strategy for comprehensive diabetes management, addressing glycemic control, weight, and cardiovascular risk factors simultaneously.
The safety profile of tirzepatide and metformin combination therapy reflects the individual adverse effect profiles of each agent, with gastrointestinal symptoms representing the most common tolerability concern. Metformin frequently causes gastrointestinal side effects including diarrhea, nausea, abdominal discomfort, and metallic taste, affecting approximately 20-30% of patients, particularly during initiation. These effects typically diminish with continued use and can be minimized through gradual dose titration and administration with meals. Extended-release metformin formulations may improve gastrointestinal tolerability.
Tirzepatide's most common adverse effects are also gastrointestinal, with nausea (12-22% depending on dose), diarrhea (12-16%), vomiting (6-10%), and constipation (5-7%) reported in clinical trials. These effects are generally mild to moderate, occur predominantly during dose escalation, and diminish over time. When combining these agents, patients may experience additive gastrointestinal effects, though clinical trial data suggest the combination is generally well-tolerated when appropriate dose titration strategies are employed.
Serious adverse effects requiring clinical vigilance include:
Lactic acidosis: A rare but potentially fatal complication of metformin, particularly in patients with renal impairment (eGFR <30 mL/min/1.73m²), acute illness, or conditions predisposing to hypoxia. Metformin should be temporarily discontinued during acute illness or procedures requiring iodinated contrast media. For intravenous contrast, metformin should be withheld at the time of or prior to the procedure in patients with eGFR 30-60 mL/min/1.73m² and for 48 hours afterward, with renal function reassessed before resuming.
Pancreatitis: Tirzepatide carries a warning for acute pancreatitis, observed in <0.2% of clinical trial participants. Patients should be counseled to report severe, persistent abdominal pain. Tirzepatide should be discontinued if pancreatitis is suspected.
Gallbladder disease: Tirzepatide may increase the risk of gallbladder-related disorders, including cholelithiasis and cholecystitis. Patients should report symptoms such as right upper quadrant pain, fever, or jaundice.
Acute kidney injury: Dehydration from tirzepatide-associated gastrointestinal side effects may increase the risk of acute kidney injury. Patients should maintain adequate fluid intake.
Hypoglycemia: While both agents have low intrinsic hypoglycemia risk, concurrent use with insulin or sulfonylureas increases risk, necessitating dose adjustments of these agents.
Thyroid C-cell tumors: Tirzepatide carries a boxed warning based on rodent studies showing thyroid C-cell tumors. It is contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
Vitamin B12 deficiency: Long-term metformin use may reduce vitamin B12 absorption. Periodic monitoring is recommended, especially in patients with anemia or peripheral neuropathy.
Neither tirzepatide nor metformin is indicated for the treatment of type 1 diabetes or diabetic ketoacidosis. Patients should be advised to seek immediate medical attention for symptoms of pancreatitis, lactic acidosis (unusual muscle pain, difficulty breathing, severe fatigue), or severe hypoglycemia. Regular monitoring of renal function is essential for patients on metformin, with dose adjustment or discontinuation required if eGFR falls below 45 mL/min/1.73m².
Appropriate dosing and titration strategies are essential for optimizing efficacy while minimizing adverse effects when combining tirzepatide and metformin. For patients already established on metformin with inadequate glycemic control, tirzepatide is typically added without adjusting the metformin dose, provided renal function is adequate and the patient tolerates metformin well.
Metformin dosing considerations:
Metformin immediate-release is typically initiated at 500 mg once or twice daily with meals, with gradual titration by 500 mg weekly to a target dose of 1000 mg twice daily (maximum 2550 mg daily, though 2000 mg daily is commonly used as the effective maximum). Extended-release formulations may be initiated at 500-1000 mg once daily with the evening meal, titrated weekly to a maximum of 2000 mg daily. Dose adjustment is required based on renal function: for patients with eGFR 30-45 mL/min/1.73m², metformin should not be newly initiated, but may be continued with close monitoring if already established; contraindicated if eGFR <30 mL/min/1.73m².
Tirzepatide dosing protocol:
Tirzepatide is administered as a once-weekly subcutaneous injection. The FDA-approved initiation dose is 2.5 mg weekly for four weeks, serving as a tolerability-building dose rather than a therapeutic dose. After four weeks, the dose is increased to 5 mg weekly. If additional glycemic control is needed after at least four weeks, the dose may be increased in 2.5 mg increments (to 7.5 mg, 10 mg, 12.5 mg, or maximum 15 mg weekly) at four-week intervals based on glycemic response and tolerability. Tirzepatide requires no dose adjustment for renal or hepatic impairment.
Practical administration guidance:
Tirzepatide can be administered any time of day, with or without meals, but should be given on the same day each week.
If a dose is missed, it should be administered within four days; if more than four days have passed, skip the dose and resume the regular schedule.
Injection sites include abdomen, thigh, or upper arm, with site rotation recommended.
When initiating tirzepatide in patients on insulin or sulfonylureas, consider reducing those doses based on individual glucose monitoring data to minimize hypoglycemia risk.
Clinicians should emphasize the importance of gradual titration to patients, explaining that the initial 2.5 mg dose helps the body adjust to the medication and reduces gastrointestinal side effects. Regular follow-up at 4-12 week intervals during titration enables assessment of glycemic response, tolerability, and need for dose adjustment. Periodic monitoring of vitamin B12 levels should be considered for patients on long-term metformin therapy, particularly those with anemia or neuropathy symptoms.
The combination of tirzepatide and metformin is appropriate for specific patient populations based on current evidence-based guidelines and clinical considerations. According to the American Diabetes Association and American College of Physicians guidelines, this combination should be considered for adults with type 2 diabetes who have not achieved glycemic targets (typically HbA1c <7% for most adults) on metformin monotherapy after three months of therapy at maximally tolerated doses.
Ideal candidates for this combination include:
Patients with HbA1c 1.5-2.5% above target on metformin monotherapy, where tirzepatide's robust glycemic efficacy can facilitate goal attainment
Individuals with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with weight-related comorbidities, given tirzepatide's substantial weight loss effects
Patients with cardiovascular risk factors who may benefit from improvements in blood pressure and lipid parameters (though for established atherosclerotic cardiovascular disease, GLP-1 receptor agonists with proven cardiovascular outcomes are preferred until tirzepatide CVOT results are available)
Those requiring avoidance of hypoglycemia (elderly, occupational considerations) due to the low hypoglycemia risk of both agents
Patients preferring once-weekly injectable therapy over multiple daily oral medications
Contraindications and precautions:
Tirzepatide is contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. It should be used with caution in patients with history of pancreatitis, though prior pancreatitis is not an absolute contraindication. Metformin is contraindicated with eGFR <30 mL/min/1.73m², severe hepatic impairment, or conditions predisposing to lactic acidosis. Neither medication is indicated for type 1 diabetes or diabetic ketoacidosis.
Special populations requiring individualized assessment:
Tirzepatide should generally be avoided during pregnancy and should be discontinued at least 1 month before planned conception. Metformin may be used during pregnancy in select cases, though insulin is typically preferred for glycemic control during pregnancy. In elderly patients (≥65 years), careful assessment of renal function is essential before initiating or continuing metformin. Patients with diabetic gastroparesis may experience symptom exacerbation with tirzepatide due to delayed gastric emptying.
Consider specialist referral for patients with severe hyperglycemia (HbA1c >10%), symptomatic hyperglycemia, diagnostic uncertainty, or recurrent hypoglycemia. Clinicians should engage in shared decision-making, discussing the benefits of improved glycemic control and weight loss against potential adverse effects, cost considerations (tirzepatide is significantly more expensive than generic metformin), and injection requirements. Insurance coverage and prior authorization requirements for tirzepatide vary and should be verified before prescribing. Patients should be counseled that this combination represents a long-term commitment requiring ongoing monitoring, lifestyle modification, and regular follow-up to optimize outcomes and ensure safety.
Yes, tirzepatide and metformin can be taken together safely as they work through different mechanisms without significant drug interactions. Tirzepatide is administered as a once-weekly injection while metformin is taken orally, typically twice daily with meals.
Clinical trials show patients combining tirzepatide with metformin experienced substantial weight reduction, with the magnitude depending on tirzepatide dose and individual factors. Weight loss with this combination exceeds that achieved with metformin alone or lifestyle modification.
The most common side effects are gastrointestinal, including nausea, diarrhea, and abdominal discomfort from both medications. Serious but rare risks include pancreatitis with tirzepatide and lactic acidosis with metformin, particularly in patients with kidney impairment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.