LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist used for type 2 diabetes and chronic weight management. Many patients taking tirzepatide wonder whether they can donate plasma while on this medication. While the FDA does not specifically prohibit plasma donation for tirzepatide users, eligibility depends on individual health status, disease control, medication side effects, and donation center policies. Understanding how tirzepatide affects donation eligibility helps patients make informed decisions about contributing to the plasma supply while maintaining their own health and safety.
Quick Answer: Patients taking tirzepatide may be eligible to donate plasma, as the medication is not specifically prohibited by the FDA, though eligibility depends on disease control, side effects, and individual donation center policies.
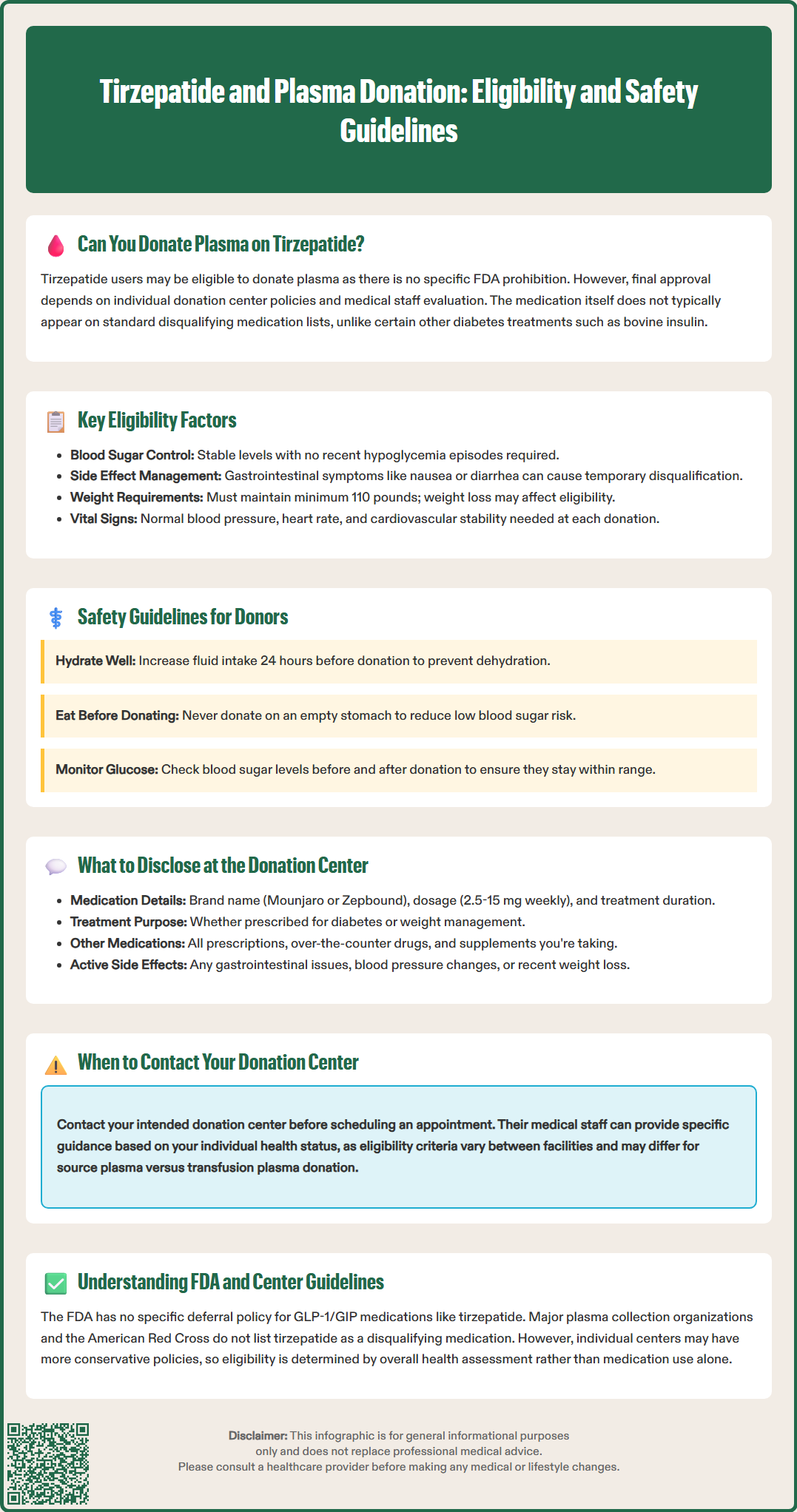
Individuals taking tirzepatide (Mounjaro, Zepbound) may be eligible to donate plasma, but eligibility depends on several factors including the reason for use, overall health status, and individual donation center policies. There is no specific FDA prohibition against plasma donation for patients using tirzepatide, though donation centers maintain discretion in accepting donors based on medication profiles and health conditions.
Tirzepatide is a glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved for type 2 diabetes management and chronic weight management. The medication works by enhancing insulin secretion, suppressing glucagon release, and slowing gastric emptying, as described in the FDA-approved prescribing information.
GLP-1/GIP agents such as tirzepatide are not currently listed as disqualifying by major US blood organizations; final eligibility is determined by the collection center's medical staff. Unlike bovine insulin (which results in indefinite deferral), tirzepatide and other GLP-1 receptor agonists do not typically appear on standard medication deferral lists. However, the underlying conditions for which tirzepatide is prescribed—particularly uncontrolled type 2 diabetes—may affect eligibility more than the medication itself.
Prospective donors should contact their intended donation center before scheduling an appointment, as policies vary between facilities. The American Red Cross, CSL Plasma, and other major organizations maintain medication databases and medical staff who can provide specific guidance based on individual circumstances and current health status. Eligibility criteria may also differ between source plasma donation (plasmapheresis) and transfusion plasma donation contexts.
Tirzepatide itself does not appear on most standard medication exclusion lists for plasma donation, but several medication-related factors influence eligibility decisions. The primary considerations include the indication for use, dosing stability, side effect profile, and overall disease management status rather than the pharmacological properties of tirzepatide alone.
For patients with type 2 diabetes, glycemic control is a critical eligibility factor. Donation centers typically require that diabetes be well-managed, with stable blood glucose levels and absence of recent hypoglycemic episodes. Centers generally assess current stability and absence of recent hypoglycemia rather than specific hemoglobin A1c numbers. Patients experiencing frequent hypoglycemia, recent dosage adjustments, or poor metabolic control may be temporarily deferred regardless of their specific medication regimen. This risk is higher in patients using tirzepatide in combination with insulin or sulfonylureas.
Common adverse effects of tirzepatide can impact donation eligibility if they cause dehydration or electrolyte imbalances. According to the FDA-approved prescribing information, gastrointestinal adverse reactions (nausea, vomiting, diarrhea) occur in up to 43% of patients taking Mounjaro and 37% of patients taking Zepbound, with higher rates during dose escalation phases. Plasma donation requires adequate hydration and stable fluid balance; donors experiencing active gastrointestinal symptoms should postpone donation until symptoms resolve.
Weight loss associated with tirzepatide may affect eligibility if it results in donors falling below minimum weight requirements (typically 110 pounds for most centers, as outlined in 21 CFR 640.65). Additionally, donation centers screen for heart rate, blood pressure, and cardiovascular stability before each donation session, as these parameters must be within normal ranges for safe donation.
Patient safety during and after plasma donation represents the paramount concern for individuals taking tirzepatide. The donation process removes approximately 600-800 mL of plasma (per FDA regulations in 21 CFR 640.65), which can temporarily affect fluid balance, blood pressure, and metabolic homeostasis—factors particularly relevant for patients managing diabetes or undergoing active weight loss.
Hypoglycemia risk requires careful consideration. While tirzepatide carries lower intrinsic hypoglycemia risk compared to insulin or sulfonylureas due to its glucose-dependent mechanism of action, the combination of fluid shifts during donation and potential meal timing disruptions may increase vulnerability to low blood glucose. This risk is significantly higher in patients who also take insulin or sulfonylureas. Patients should eat a healthy meal and hydrate before donation; do not donate on an empty stomach. Those with diabetes should monitor blood glucose levels before and after donation and maintain levels within their prescribed range throughout the donation process.
Dehydration represents another significant concern. Tirzepatide's gastrointestinal effects, combined with plasma volume removal, can compromise hydration status. Donors should increase fluid intake in the 24 hours before donation, avoid donation during periods of active nausea or diarrhea, and continue adequate hydration post-donation. If experiencing signs of dehydration—including dizziness, weakness, or decreased urine output—donors should notify staff immediately during donation or seek appropriate medical care for severe or persistent symptoms.
Cardiovascular stability is essential for safe donation. Donors should have stable blood pressure and heart rate. The donation process itself can cause vasovagal reactions, particularly in individuals with autonomic dysfunction or those experiencing rapid weight loss. Donors should report any history of fainting, dizziness upon standing, or cardiovascular symptoms to medical staff before proceeding with donation.
The FDA regulates plasma collection through Title 21 of the Code of Federal Regulations, particularly 21 CFR 630.10 (donor eligibility) and 21 CFR 640 Subpart L (Source Plasma requirements), which establish donor eligibility criteria and safety standards. While there is no specific FDA deferral for GLP-1/GIP agents, regulations require that donors be in good health and that medications do not pose risks to recipients or compromise donor safety during the collection process.
The FDA's guidance on donor eligibility focuses on excluding individuals with conditions that could transmit infectious diseases, compromise plasma quality, or endanger donor health. Medications are evaluated based on several criteria: whether they indicate an underlying disqualifying condition, whether they pose teratogenic risks to potential recipients, whether they affect donor safety during phlebotomy, and whether they compromise plasma product integrity.
Major plasma collection organizations—including CSL Plasma, BioLife Plasma Services, and Grifols—maintain internal medication policies that supplement FDA regulations. These organizations employ medical directors who review medication lists and make eligibility determinations based on current scientific evidence, safety data, and standards from organizations like the AABB (Association for the Advancement of Blood & Biotherapies) and the Plasma Protein Therapeutics Association (PPTA). Policies may vary between organizations, and some centers maintain more conservative approaches to newer medications with limited post-marketing experience.
The American Red Cross, which collects both whole blood and plasma, maintains a searchable medication database that provides guidance on eligibility. As of current guidelines, GLP-1 receptor agonists including tirzepatide are not listed as disqualifying medications, though donors are advised to discuss their complete medical history with collection staff. The organization emphasizes that medication evaluation occurs in the context of overall health assessment rather than as isolated criteria.
Complete and accurate medication disclosure is both a regulatory requirement and an ethical obligation for plasma donors. Donation centers rely on donor honesty to make appropriate eligibility determinations and ensure safety for both donors and plasma recipients. Individuals taking tirzepatide should provide comprehensive information about their medication regimen, underlying health conditions, and current symptom status.
When discussing tirzepatide with donation center staff, donors should specify: the brand name (Mounjaro or Zepbound), current dosage (ranging from 2.5 mg to 15 mg weekly), duration of therapy, indication for use (type 2 diabetes or chronic weight management), and any recent dosage changes. Donors should also report any recent dose escalations and current symptoms, as these may affect eligibility decisions at some centers.
Beyond tirzepatide itself, donors must disclose all concurrent medications, including over-the-counter drugs, supplements, and other prescription medications. Patients with type 2 diabetes often take multiple medications—such as metformin, SGLT2 inhibitors, or statins—that require separate evaluation. It is particularly important to disclose any concomitant insulin or sulfonylurea therapy due to increased hypoglycemia risk, and any history of bovine insulin use (which is an indefinite deferral criterion in the US). The combination of medications, rather than any single agent, may influence eligibility. Donors should bring a current medication list or prescription bottles to facilitate accurate documentation.
Donors should report any recent or ongoing side effects from tirzepatide, particularly gastrointestinal symptoms, changes in blood pressure, episodes of hypoglycemia, or significant weight changes. Active symptoms may warrant temporary deferral even if the medication itself is acceptable. Additionally, donors should inform staff about their diabetes management status if applicable, including stability of blood glucose levels, frequency of monitoring, and history of hypoglycemic episodes. This information enables medical staff to make individualized safety assessments and provide appropriate guidance for safe donation.
Tirzepatide does not automatically disqualify you from plasma donation, as it does not appear on FDA or major blood organization exclusion lists. However, eligibility depends on your overall health status, disease control (particularly diabetes stability), absence of active side effects, and individual donation center policies.
You should disclose the brand name (Mounjaro or Zepbound), current dosage, indication for use (diabetes or weight management), duration of therapy, any recent dose changes, and current side effects. Also report all other medications, particularly insulin or sulfonylureas, and your diabetes control status if applicable.
Yes, active gastrointestinal side effects such as nausea, vomiting, or diarrhea can cause dehydration and electrolyte imbalances that may temporarily defer donation. Donors should wait until symptoms resolve and ensure adequate hydration before attempting to donate plasma.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.