LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) is a dual GIP/GLP-1 receptor agonist that significantly reduces appetite and slows gastric emptying. While these effects support weight loss, they can make meeting daily protein requirements challenging. Many patients wonder whether protein shakes are safe and effective during tirzepatide treatment. This article examines the compatibility of tirzepatide and protein shakes, addresses timing considerations, discusses optimal shake selection, and provides practical strategies for maintaining adequate protein intake while managing common gastrointestinal side effects during treatment.
Quick Answer: Protein shakes are safe to consume with tirzepatide, with no contraindications or documented interactions between the medication and dietary protein supplements.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). This medication works by enhancing insulin secretion in response to meals, suppressing glucagon release, and slowing gastric emptying—an effect that is most pronounced after initial doses and typically diminishes over time. The delayed gastric emptying contributes to prolonged satiety and reduced appetite, which are central to its weight loss effects.
The pharmacological actions of tirzepatide have important nutritional implications. Patients commonly experience reduced hunger, early satiety, and decreased overall food intake. Many individuals taking tirzepatide report substantial reductions in caloric intake, which, while beneficial for weight loss, creates potential challenges for maintaining adequate protein consumption—a critical macronutrient for preserving lean muscle mass during weight reduction.
Gastrointestinal side effects occur frequently with tirzepatide. According to the FDA labels, nausea occurs in 17-25% of patients taking Zepbound and 12-24% taking Mounjaro, with vomiting and diarrhea also commonly reported. These symptoms typically peak within the first few weeks of treatment or after dose increases. The combination of reduced appetite and gastrointestinal discomfort can make consuming adequate protein through traditional whole foods challenging.
Importantly, tirzepatide's delayed gastric emptying can reduce the absorption of oral medications, including oral contraceptives. Patients using oral contraceptives should use an additional non-hormonal method of contraception for 4 weeks after initiating tirzepatide or increasing the dose. Additionally, patients taking insulin or sulfonylureas may have an increased risk of hypoglycemia when starting tirzepatide and should monitor blood glucose levels carefully.
There is no official contraindication to consuming protein shakes while taking tirzepatide. The FDA-approved prescribing information does not list protein supplements as incompatible with the medication, and no pharmacokinetic interactions between tirzepatide and dietary protein have been documented. Protein shakes can serve as a valuable tool for patients struggling to meet their protein requirements through solid foods alone, particularly when appetite suppression and early satiety limit meal sizes.
Maintaining adequate protein intake during tirzepatide treatment is clinically important for several reasons. During weight loss, the body loses both fat mass and lean muscle mass. Research suggests that without adequate protein intake and resistance exercise, a significant portion of weight lost may come from lean tissue, though the exact proportion varies based on individual factors and interventions. The Recommended Dietary Allowance (RDA) for protein is 0.8 grams per kilogram of actual body weight per day for adults. However, higher intakes of 1.0-1.6 g/kg/day may be beneficial during weight loss to help preserve muscle mass, support metabolic health, and promote better long-term weight maintenance outcomes.
Patients with chronic kidney disease (CKD) not on dialysis should discuss protein intake with their healthcare provider, as they may need to limit protein to 0.8 g/kg/day or less, depending on kidney function. Patients with diabetes who take insulin or sulfonylureas should monitor blood glucose levels when changing their protein and carbohydrate intake patterns, as these changes may affect medication requirements.
The decision to incorporate protein shakes should be individualized based on each patient's baseline protein intake, weight loss goals, tolerance of solid foods, and overall nutritional status. Patients should discuss their specific protein needs with their healthcare provider or a registered dietitian familiar with weight management medications.
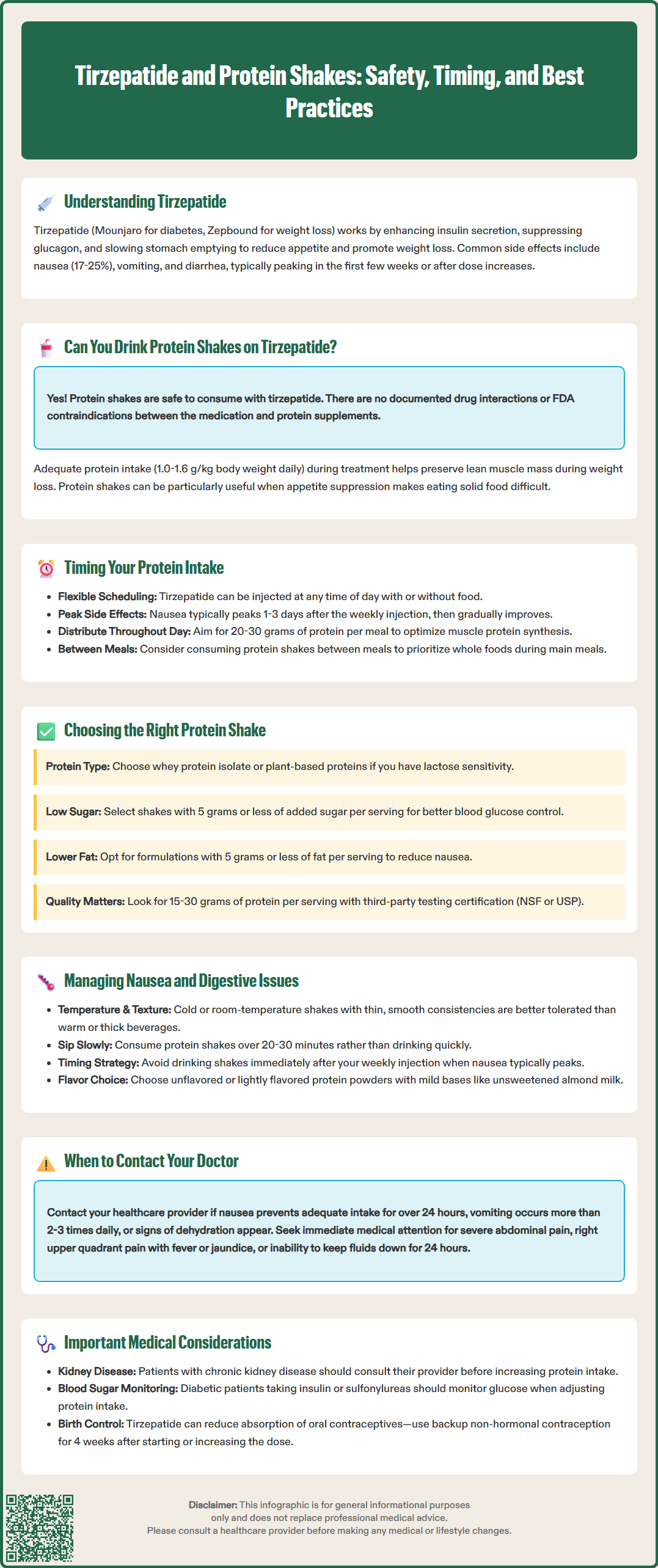
Tirzepatide is administered as a once-weekly subcutaneous injection, and unlike some oral medications, there are no specific timing restrictions regarding food or beverage consumption around the injection time. The medication can be given at any time of day, with or without meals, providing flexibility for patients. However, understanding the medication's pharmacodynamic effects can help optimize protein shake consumption throughout the week.
Gastrointestinal side effects, particularly nausea, often follow a predictable pattern related to the injection schedule. Many patients report that symptoms are most pronounced in the 1-3 days following their weekly injection, then gradually improve as the week progresses. This pattern reflects the medication's pharmacokinetics and effect on gastric emptying, which is most significant after the first dose and following dose increases. Patients may find it easier to consume protein shakes during the latter part of their dosing week when nausea has subsided and appetite begins to return slightly.
For daily protein distribution, spreading intake throughout the day appears more beneficial than consuming large amounts in a single sitting. Research on protein metabolism suggests that distributing protein across multiple meals (approximately 20-30 grams per meal) optimizes muscle protein synthesis more effectively than consuming the same total amount concentrated in one or two meals. Given the early satiety associated with tirzepatide, smaller, more frequent protein servings—whether from shakes or food—may be better tolerated than attempting to consume large protein loads at once.
Some patients find that consuming protein shakes between meals, rather than with meals, works better when appetite is suppressed. This approach allows them to prioritize nutrient-dense whole foods during main meals while using shakes as convenient protein supplements during times when solid food feels less appealing. There is no evidence that protein shakes interfere with tirzepatide's efficacy or absorption, so timing should be based primarily on individual tolerance and symptom patterns.
Selecting an appropriate protein shake while taking tirzepatide requires consideration of both nutritional composition and gastrointestinal tolerability. Not all protein supplements are equivalent, and certain formulations may be better suited for patients experiencing the appetite suppression and digestive side effects common with this medication.
Protein source considerations include whey, casein, soy, pea, and other plant-based proteins. Whey protein isolate is rapidly absorbed and generally well-tolerated, making it a popular choice. However, some patients with lactose sensitivity may experience increased gastrointestinal discomfort with whey concentrate formulations. In these cases, whey isolate (which contains minimal lactose), plant-based proteins, or lactose-free options may be preferable. There is no evidence that any particular protein source interferes with tirzepatide's mechanism of action.
Sugar and carbohydrate content warrant careful attention. Many commercial protein shakes contain added sugars, which can contribute unnecessary calories and potentially affect blood glucose control in patients with diabetes. As a practical starting point, products with minimal added sugars (around 5 grams or less per serving) may be preferable for most patients. Patients with diabetes should read Nutrition Facts labels carefully and account for total carbohydrates in their meal planning. Some individuals may experience gastrointestinal symptoms from sugar alcohols and certain artificial sweeteners, which could potentially compound digestive side effects from tirzepatide.
Fat content and additives also influence tolerability. Higher-fat protein shakes may worsen nausea and delay gastric emptying further, potentially intensifying the sensation of fullness or discomfort. Lower-fat formulations (around 5 grams or less per serving) are often better tolerated initially. Additionally, shakes with minimal additives, artificial ingredients, and thickening agents may cause fewer digestive issues.
Patients should aim for protein shakes providing 15-30 grams of protein per serving, allowing flexibility to meet individual needs without overwhelming the digestive system. When possible, choose supplements that have been third-party tested for quality and purity (look for NSF or USP certification). Consulting with a registered dietitian can help identify products that align with specific dietary requirements, taste preferences, and tolerance levels.
Nausea represents one of the most common and challenging side effects of tirzepatide, affecting patient adherence and nutritional intake. Strategic approaches to protein consumption can help patients maintain adequate nutrition while minimizing gastrointestinal discomfort during treatment.
Temperature and texture modifications can significantly impact tolerability. Many patients find that cold or room-temperature protein shakes are better tolerated than warm beverages when nausea is present. Thin, smooth consistencies generally cause less discomfort than thick, heavy shakes. Diluting protein powder with extra water or unsweetened almond milk creates a lighter beverage that may be easier to consume. Some patients prefer freezing protein shakes into ice pops, allowing for gradual consumption in small amounts throughout the day.
Consumption strategies should emphasize small volumes and slow intake. Rather than drinking an entire protein shake quickly, patients experiencing nausea should sip slowly over 20-30 minutes. Taking small sips every few minutes allows the stomach to accommodate the liquid gradually without triggering increased nausea or vomiting. Avoiding drinking protein shakes on a completely empty stomach may also help; consuming a few crackers or a small piece of fruit first can sometimes reduce nausea. Patients with diabetes should account for any carbohydrates in these foods and monitor blood glucose accordingly.
Flavor considerations matter more than many patients realize. Strong, sweet, or artificial flavors can trigger or worsen nausea. Unflavored or lightly flavored protein powders mixed with mild bases like unsweetened almond milk or water are often better tolerated. Avoiding protein shakes immediately after the weekly injection, when nausea typically peaks, and instead consuming them during the latter part of the dosing week may improve tolerance.
When to seek medical advice: Patients should contact their healthcare provider if nausea prevents adequate fluid or protein intake for more than 24 hours, if vomiting occurs more than 2-3 times daily, or if signs of dehydration develop (decreased urination, dizziness, extreme fatigue). Patients should seek immediate medical attention for severe, persistent abdominal pain (which could indicate pancreatitis), symptoms of gallbladder disease (right upper quadrant pain, fever, jaundice), or inability to keep any fluids down for 24 hours. Healthcare providers may prescribe antiemetics such as ondansetron or, for short-term use only, metoclopramide (which carries a boxed warning for tardive dyskinesia). Maintaining open communication with the prescribing provider ensures that nutritional challenges are addressed promptly, supporting both treatment adherence and optimal health outcomes during weight loss.
Yes, there are no contraindications to consuming protein shakes with tirzepatide. The FDA-approved prescribing information does not list protein supplements as incompatible, and no pharmacokinetic interactions have been documented between tirzepatide and dietary protein.
Protein shakes can be consumed at any time, as tirzepatide is a weekly injection with no food timing restrictions. Many patients find shakes easier to tolerate 3-7 days after their weekly injection when nausea subsides, and spreading protein intake across multiple small servings throughout the day optimizes tolerance and muscle protein synthesis.
Lower-fat protein shakes (5 grams or less per serving) with minimal added sugars, providing 15-30 grams of protein, are generally best tolerated. Cold or room-temperature shakes with thin consistency, consumed slowly over 20-30 minutes, help minimize nausea and gastrointestinal discomfort common with tirzepatide treatment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.