LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide and sermorelin together represent a combination therapy approach that some patients and clinicians consider for metabolic management, though this pairing lacks formal clinical study. Tirzepatide, an FDA-approved dual GIP/GLP-1 receptor agonist for type 2 diabetes and obesity, works through incretin-based glucose regulation and appetite suppression. Sermorelin, a growth hormone-releasing hormone analog, stimulates endogenous growth hormone production but lacks FDA approval for metabolic indications. While no direct contraindication exists for concurrent use, the absence of controlled trials means safety and efficacy remain inadequately characterized. Understanding the distinct mechanisms, potential interactions, and monitoring requirements is essential for informed clinical decision-making.
Quick Answer: Tirzepatide and sermorelin can be used together without known direct contraindications, but this combination lacks clinical trial evidence and requires careful medical supervision.
Tirzepatide and sermorelin operate through fundamentally different physiological pathways, making their mechanisms of action distinct yet potentially complementary in metabolic management.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). This medication works by enhancing insulin secretion in response to elevated glucose levels, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways. The dual agonist mechanism provides robust glycemic control and significant weight reduction, with clinical trials demonstrating A1C reductions of 1.9–2.4% and weight loss of approximately 15–22% of body weight in non-diabetic adults with obesity (SURMOUNT-1 trial), with more modest weight loss typically observed in patients with type 2 diabetes.
Sermorelin is a growth hormone-releasing hormone (GHRH) analog consisting of the first 29 amino acids of naturally occurring GHRH. It stimulates the anterior pituitary gland to produce and release endogenous growth hormone (GH) in a pulsatile manner that mimics physiological secretion patterns. Unlike synthetic growth hormone, sermorelin preserves the body's natural feedback mechanisms. It is sometimes used off-label for purported anti-aging purposes, body composition improvement, and metabolic enhancement, though it lacks FDA approval for these indications. Currently, no FDA-approved sermorelin products are marketed in the US, and it is typically accessed through compounding pharmacies. The proposed effects of sermorelin (increased lean muscle mass, improved sleep quality, enhanced recovery, and metabolic benefits) remain largely theoretical or anecdotal in adults without documented growth hormone deficiency.
These distinct mechanisms—tirzepatide's incretin-based glucose and appetite regulation versus sermorelin's growth hormone axis stimulation—theoretically address different aspects of metabolic health without direct pharmacological overlap.
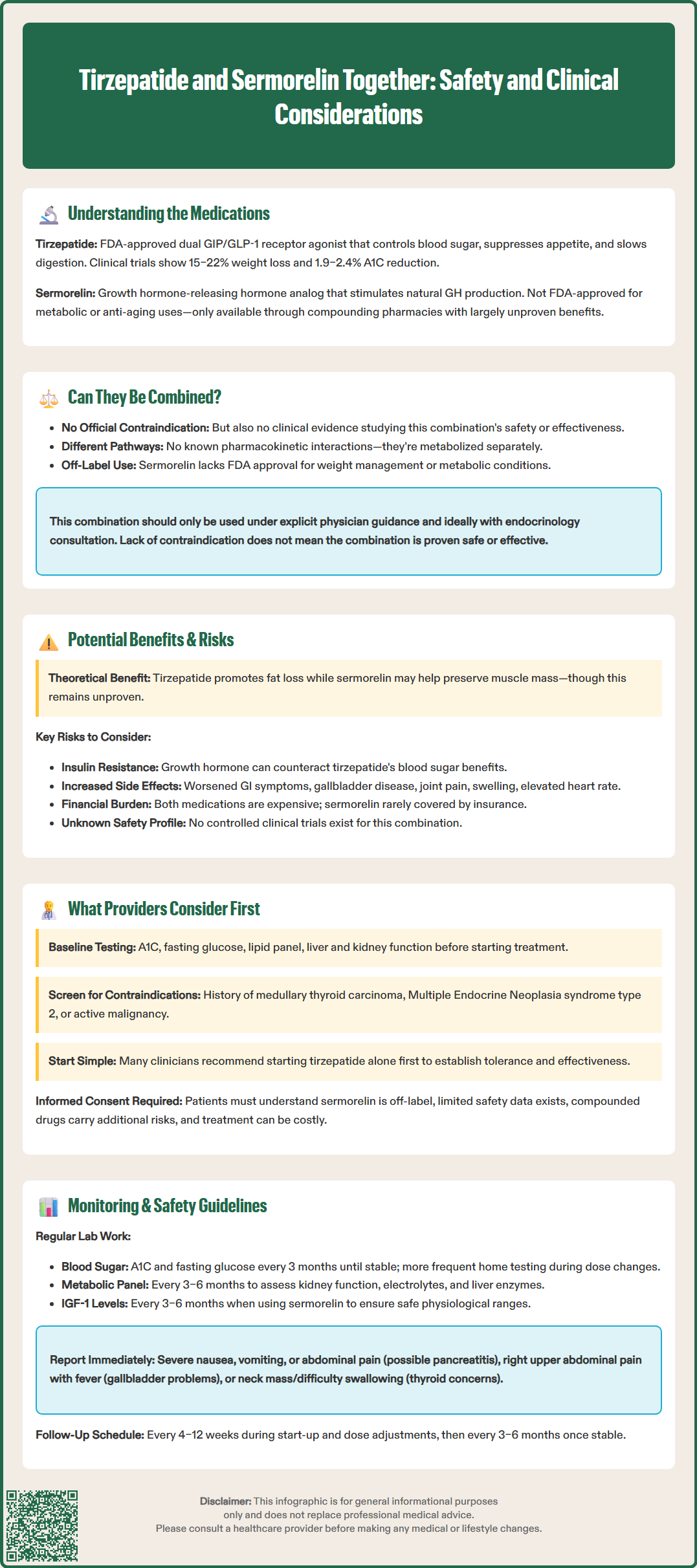
There is no official contraindication to using tirzepatide and sermorelin concurrently, but there is also limited clinical evidence specifically evaluating this combination. Neither the FDA-approved prescribing information for tirzepatide nor published clinical guidelines explicitly address sermorelin co-administration. The FDA labeling for tirzepatide notes that safety and efficacy with other medications for weight management have not been established.
From a pharmacological perspective, these medications have no known pharmacokinetic interactions. Tirzepatide is metabolized through proteolytic cleavage and does not rely on cytochrome P450 enzymes, while sermorelin undergoes rapid enzymatic degradation in plasma. However, the absence of evidence for interactions is not evidence of safety, as no controlled studies have evaluated this combination.
Several important considerations exist. First, sermorelin is not FDA-approved for metabolic or weight management indications, and its use in these contexts remains off-label with limited evidence quality. Second, both medications can influence metabolic parameters—tirzepatide through direct glucose regulation and weight loss, sermorelin through growth hormone-mediated effects on insulin sensitivity and body composition. Third, the combination lacks robust safety data from controlled trials, meaning potential synergistic effects or unexpected interactions remain inadequately characterized.
Patients should never initiate this combination without explicit physician guidance, as both medications require prescription authorization and medical supervision. Endocrinology consultation is advisable when considering off-label combination therapy. The absence of formal contraindication does not equate to established safety or efficacy for combined use.
The theoretical rationale for combining tirzepatide and sermorelin centers on addressing complementary aspects of metabolic health, though evidence supporting this approach remains largely theoretical rather than evidence-based.
Potential theoretical benefits include:
Body composition considerations: Tirzepatide promotes significant fat loss through appetite suppression and metabolic effects, while sermorelin might theoretically support lean muscle preservation through growth hormone stimulation—potentially mitigating the muscle loss sometimes observed with rapid weight reduction.
Metabolic effects: Tirzepatide addresses insulin resistance, glycemic control, and weight reduction, while sermorelin may influence metabolic processes through the GH-IGF-1 axis, though clinical significance remains unproven.
Subjective improvements: Some patients report enhanced energy with growth hormone-related therapies, which might support lifestyle modifications that complement tirzepatide's effects, though this remains anecdotal.
Potential risks and concerns include:
Glucose metabolism effects: Growth hormone exhibits counter-regulatory effects on insulin, potentially increasing insulin resistance. This could theoretically oppose tirzepatide's glucose-lowering effects. Patients with diabetes require careful glucose monitoring.
Additive gastrointestinal effects: Tirzepatide commonly causes nausea, vomiting, diarrhea, and constipation, particularly during dose escalation. While sermorelin's GI side effects are generally mild, combination therapy might increase symptom burden.
Growth hormone-related adverse effects: Sermorelin may cause edema, arthralgia, paresthesia (including carpal tunnel syndrome), and glucose intolerance through GH stimulation.
Gallbladder disease: Tirzepatide is associated with increased risk of gallbladder disease, including cholelithiasis and cholecystitis.
Cardiovascular considerations: Both medications can affect heart rate and cardiovascular parameters. Tirzepatide increases heart rate modestly (average 2–4 bpm in clinical trials), while growth hormone effects on cardiac function require monitoring in susceptible individuals.
Cost and access: Both medications are expensive, and sermorelin for metabolic purposes is rarely covered by insurance, creating significant financial burden without guaranteed benefit.
The absence of controlled trials means the true benefit-risk profile remains inadequately defined.
Clinicians evaluating potential tirzepatide and sermorelin combination therapy must conduct comprehensive assessment addressing multiple clinical domains before initiating treatment.
Patient selection criteria include:
Clear therapeutic indication: Tirzepatide should be prescribed for FDA-approved indications (type 2 diabetes or obesity with BMI ≥30 or ≥27 with weight-related comorbidity). Tirzepatide is not indicated for type 1 diabetes. Suspected growth hormone deficiency requires formal evaluation with stimulation testing per Endocrine Society guidelines and endocrinology referral; somatropin (not sermorelin) is the standard FDA-approved therapy for confirmed deficiency.
Baseline metabolic assessment: Complete evaluation including A1C, fasting glucose, lipid panel, liver function tests, renal function (eGFR), and appropriate cardiovascular assessment.
Contraindication screening: Tirzepatide is contraindicated in personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2, and in patients with severe hypersensitivity to tirzepatide. Caution is advised in patients with a history of pancreatitis or severe gastrointestinal disease. Growth hormone-related therapies should be avoided in active malignancy, as growth hormone may promote tumor growth.
Pregnancy planning: Tirzepatide for weight management should be discontinued if pregnancy occurs or is planned. Women of reproductive potential should use effective contraception during treatment.
Clinical decision-making factors include:
Treatment goals alignment: Providers must establish whether combination therapy addresses distinct, clinically meaningful objectives that justify added complexity, cost, and potential risk.
Sequential versus simultaneous initiation: Many clinicians prefer establishing tirzepatide tolerance and efficacy before adding other therapies, allowing clearer attribution of benefits and adverse effects.
Alternative approaches: Consideration of whether optimizing tirzepatide dosing, lifestyle interventions, or other evidence-based therapies might achieve goals without off-label combination therapy.
Informed consent: Patients must understand the off-label nature of sermorelin use, limited safety data for combination therapy, compounded medication risks, and financial implications.
Shared decision-making incorporating patient preferences, realistic expectations, and transparent discussion of evidence limitations is essential before proceeding with combination therapy.
Patients receiving tirzepatide and sermorelin together require enhanced monitoring protocols beyond standard care for either medication alone, given the absence of established safety data for this combination.
Baseline and ongoing laboratory monitoring should include:
Glucose parameters: A1C and fasting glucose at baseline, 3 months, and every 3 months thereafter until stable, then potentially less frequently per ADA guidelines. Patients with diabetes should perform home glucose monitoring as directed, with increased frequency during dose adjustments. Growth hormone's counter-regulatory effects necessitate vigilance for glycemic deterioration.
Metabolic panel: Comprehensive metabolic panel every 3–6 months to assess renal function, electrolytes, and liver enzymes. Tirzepatide can cause acute kidney injury, particularly with severe gastrointestinal symptoms causing dehydration.
Lipid profile: Assessment every 3–6 months, as both medications may influence lipid metabolism.
IGF-1 levels: Periodic monitoring (every 3–6 months) when using sermorelin to ensure physiological rather than supraphysiological growth hormone stimulation.
Clinical monitoring and patient safety advice includes:
Gastrointestinal symptoms: Patients should report severe or persistent nausea, vomiting, or abdominal pain, which may indicate pancreatitis (a warning in tirzepatide labeling) or require dose adjustment.
Gallbladder disease symptoms: Education on recognizing right upper quadrant pain, fever, or jaundice that may indicate cholelithiasis or cholecystitis.
Thyroid tumor symptoms: Patients should report symptoms such as neck mass, dysphagia, hoarseness, or dyspnea. Routine calcitonin monitoring or thyroid ultrasound is not recommended unless clinically indicated.
Hypoglycemia awareness: Education on recognition and management, particularly for patients on insulin or sulfonylureas with tirzepatide.
Injection site reactions: Monitoring for local reactions, proper injection technique education, and site rotation.
Growth hormone-related effects: Monitoring for edema, joint pain, carpal tunnel symptoms, and glucose changes.
Referral triggers include persistent hyperglycemia despite therapy, suspected pancreatitis, acute kidney injury, gallbladder disease, or concerning cardiovascular symptoms. Endocrinology consultation is appropriate for complex cases or inadequate response. Regular follow-up every 4–12 weeks during initiation and dose titration, then every 3–6 months once stable, ensures appropriate safety surveillance for this inadequately studied combination.
There is no known contraindication to using tirzepatide and sermorelin together, but no controlled clinical trials have evaluated this combination's safety or efficacy. Medical supervision with enhanced monitoring is essential if considering concurrent use.
Potential risks include growth hormone's counter-regulatory effects on glucose metabolism that may oppose tirzepatide's benefits, additive gastrointestinal symptoms, and growth hormone-related adverse effects such as edema and joint pain. Enhanced monitoring of glucose parameters and metabolic function is required.
Yes, enhanced monitoring is necessary including glucose parameters every 3 months, comprehensive metabolic panels every 3–6 months, periodic IGF-1 levels, and clinical surveillance for gastrointestinal symptoms, gallbladder disease, and growth hormone-related effects.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.