LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide and testosterone together represent a combination that men with obesity or type 2 diabetes and documented hypogonadism may consider under medical supervision. Tirzepatide, a dual GIP/GLP-1 receptor agonist approved for diabetes management and weight loss, works through distinct mechanisms from testosterone replacement therapy (TRT), which restores physiological hormone levels in men with confirmed low testosterone. While no formal contraindication exists for concurrent use, the interaction between significant weight loss and hormone levels creates important clinical considerations. Understanding the safety profile, monitoring requirements, and potential physiological interactions of these therapies is essential for anyone contemplating combined treatment.
Quick Answer: Tirzepatide and testosterone can be used together as no formal contraindication exists, but combined therapy requires medical supervision and individualized monitoring.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). It works by enhancing insulin secretion in response to meals, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways. Clinical trials have demonstrated substantial weight loss—with SURMOUNT obesity trials showing 15–22% of body weight reduction at higher doses, while more modest losses were observed in type 2 diabetes trials.
Testosterone replacement therapy (TRT) is prescribed for men with clinically confirmed hypogonadism due to specific pathology, characterized by low serum testosterone levels and associated symptoms such as reduced libido, fatigue, decreased muscle mass, and mood changes. TRT aims to restore physiological testosterone levels through various formulations including intramuscular injections, transdermal gels, patches, or subcutaneous pellets. The American Urological Association (AUA) guidelines recommend a diagnostic threshold of <300 ng/dL, while the Endocrine Society recommends using the laboratory-specific lower limit (approximately 264 ng/dL). Both require morning testosterone measurements on two separate occasions plus clinical symptoms. TRT is not indicated for age-related testosterone decline without clear pathologic hypogonadism.
Both therapies address distinct but sometimes overlapping health concerns. Obesity is associated with lower testosterone levels in men through multiple mechanisms, including increased aromatase activity in adipose tissue converting testosterone to estradiol, and inflammatory cytokines suppressing the hypothalamic-pituitary-gonadal axis. Conversely, low testosterone may contribute to increased fat mass and reduced lean body mass. Understanding how these medications work independently provides essential context for evaluating their combined use in clinical practice.
There is no official contraindication to using tirzepatide and testosterone therapy concurrently. Neither the FDA prescribing information for tirzepatide nor established endocrinology guidelines identify testosterone as an interacting medication that would preclude combined use. The two agents have different mechanisms of action and are metabolized through distinct pathways—tirzepatide is a peptide degraded by proteolytic enzymes, while testosterone undergoes hepatic metabolism primarily via cytochrome P450 enzymes.
Many patients may have legitimate clinical indications for both medications simultaneously. Men with type 2 diabetes or obesity who also have documented hypogonadism represent a common clinical scenario where dual therapy might be appropriate. The metabolic benefits of tirzepatide—including weight loss, improved insulin sensitivity, and improvements in cardiometabolic risk factors (definitive cardiovascular outcome benefits are not yet established)—do not inherently conflict with the physiological goals of testosterone replacement.
However, the absence of a formal contraindication does not mean these therapies should be combined without medical supervision. Each medication carries its own risk profile and monitoring requirements. Tirzepatide has a boxed warning contraindication for patients with personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). It may cause gastrointestinal adverse effects (nausea, vomiting, diarrhea), risk of hypoglycemia when combined with insulin or sulfonylureas, and is not recommended in severe gastrointestinal disease including gastroparesis. Tirzepatide can also reduce the exposure to oral contraceptives; non-oral or backup contraception is advised for 4 weeks after initiation and each dose escalation. Testosterone therapy requires monitoring for polycythemia, prostate health changes, blood pressure increases, and potential worsening of sleep apnea.
The decision to use both medications together should be individualized, based on documented clinical need for each therapy, careful assessment of the risk-benefit profile, and ongoing medical monitoring. Self-prescribing or obtaining either medication without proper medical evaluation is not advisable.
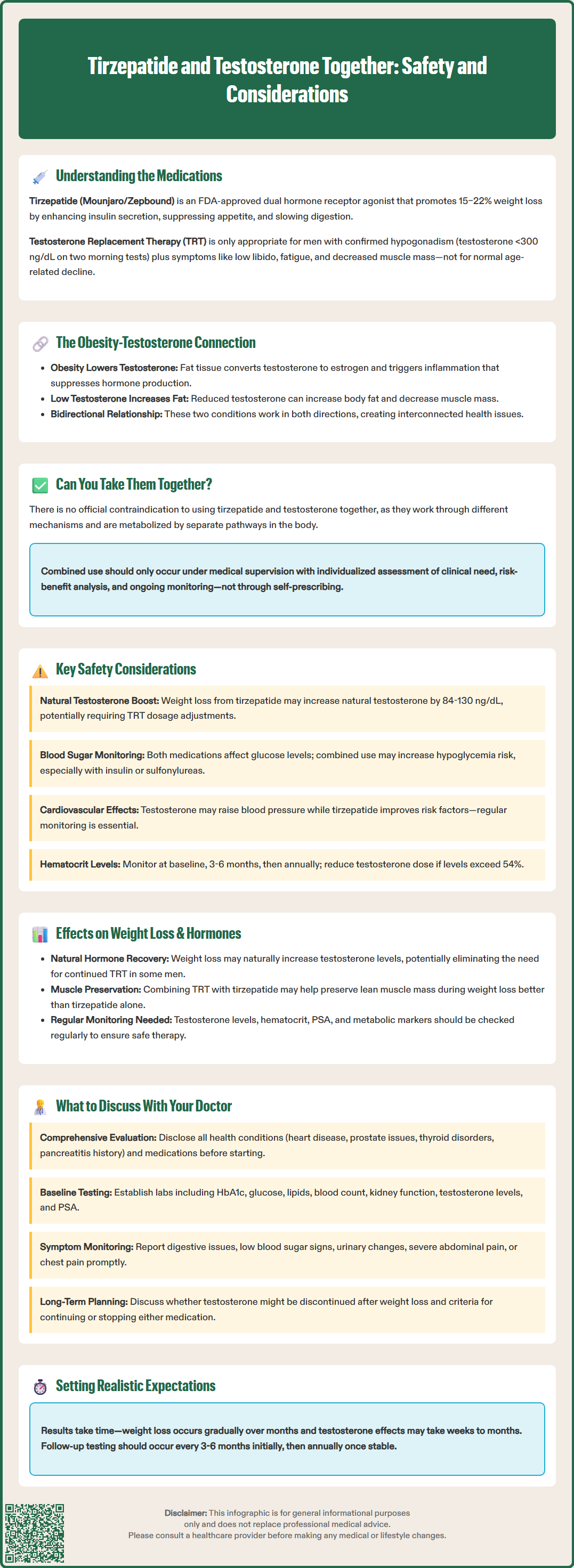
While direct pharmacokinetic interactions between tirzepatide and testosterone are not documented, several indirect physiological interactions warrant clinical attention. Significant weight loss induced by tirzepatide may influence endogenous testosterone production. Studies have shown that substantial weight reduction in obese men can increase endogenous testosterone levels by approximately 84–130 ng/dL (2.9–4.5 nmol/L), potentially reducing the need for exogenous testosterone or requiring dose adjustments in men already receiving TRT.
Testosterone therapy may influence glycemic control, though effects are variable. Some evidence suggests testosterone replacement in hypogonadal men with diabetes improves insulin sensitivity and may modestly reduce HbA1c levels. This could theoretically enhance tirzepatide's glucose-lowering effects, potentially increasing hypoglycemia risk in patients also taking insulin or sulfonylureas. Blood glucose monitoring may need intensification when initiating or adjusting either therapy.
Cardiovascular considerations require particular attention. Tirzepatide improves cardiovascular risk factors, though definitive outcome data are pending. Testosterone's cardiovascular safety profile has been studied in the TRAVERSE trial, which showed non-inferior major adverse cardiovascular events compared to placebo, though FDA labeling emphasizes the potential for increased blood pressure with testosterone products. Regular blood pressure monitoring is recommended for patients on testosterone therapy, particularly when combined with other medications.
Fluid retention represents another consideration. Testosterone can cause sodium and water retention, potentially exacerbating hypertension or heart failure. While tirzepatide is not typically associated with significant fluid retention, the combined effect on fluid balance should be monitored, particularly in patients with compromised cardiac function. Hematocrit should be monitored at baseline, 3–6 months after starting testosterone, and then annually, with dose reduction or interruption recommended if hematocrit exceeds 54%. Additionally, tirzepatide carries warnings for pancreatitis and gallbladder disease, requiring vigilance for symptoms such as severe abdominal pain.
The interplay between weight loss and testosterone levels creates a complex dynamic when these therapies are combined. Tirzepatide-induced weight loss may independently improve testosterone levels through multiple mechanisms: reduction in adipose tissue decreases aromatase activity (limiting testosterone conversion to estradiol), weight loss reduces inflammatory cytokines that suppress gonadal function, and improved insulin sensitivity may enhance hypothalamic-pituitary-gonadal axis function. Some men with obesity-related hypogonadism may experience normalization of testosterone levels with significant weight loss alone, potentially obviating the need for continued TRT.
Conversely, testosterone therapy may influence body composition changes during tirzepatide treatment. TRT promotes increased lean muscle mass and reduced fat mass independently. When combined with tirzepatide's effects, patients might experience more favorable body composition changes—greater preservation of lean muscle mass during weight loss—compared to tirzepatide alone. This could be clinically beneficial, as preserving muscle mass during significant weight reduction is important for maintaining metabolic rate and physical function.
However, these potential synergistic effects on body composition have not been systematically studied in controlled trials. The magnitude and clinical significance of any additive benefits remain uncertain. Monitoring hormone levels becomes particularly important when combining these therapies. Men receiving TRT should have testosterone levels checked periodically, with timing dependent on the formulation (e.g., trough levels for injections). The goal is to maintain testosterone in the mid-normal range. If endogenous production increases substantially due to weight loss, testosterone doses may require reduction to avoid supraphysiological levels.
Additionally, other laboratory parameters warrant monitoring based on clinical indications. Comprehensive metabolic assessment helps optimize both therapies and identify any adverse changes requiring intervention. Regular monitoring of hematocrit, PSA (when appropriate), and metabolic parameters provides the foundation for safe, effective combined therapy.
Before combining tirzepatide and testosterone therapy, comprehensive medical evaluation is essential. Discuss your complete medical history, including cardiovascular disease, prostate conditions, sleep apnea, polycythemia, liver disease, and any history of pancreatitis, gallbladder disease, or thyroid disorders. Specifically, disclose any personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2, as these are contraindications to tirzepatide. Provide a full medication list, as other drugs may interact with either therapy. Your provider should confirm appropriate indications for each medication—documented type 2 diabetes or obesity for tirzepatide, and biochemically confirmed hypogonadism with symptoms for testosterone.
Key monitoring parameters to establish with your provider include:
Baseline laboratory testing: HbA1c, fasting glucose, lipid panel, complete blood count (including hematocrit), comprehensive metabolic panel (including renal function), testosterone levels (morning sample), prostate-specific antigen (PSA) based on age and risk factors (following shared decision-making guidelines), and other tests as clinically indicated
Follow-up schedule: For diabetes management, HbA1c every 3 months until stable; more frequent visits during tirzepatide dose titration; testosterone levels at 3–6 months after starting therapy or dose adjustment, then annually; hematocrit at 3–6 months, then annually
Symptom monitoring: Report gastrointestinal symptoms, signs of hypoglycemia, changes in urinary function, mood changes, or cardiovascular symptoms promptly; be alert for gallbladder symptoms (right upper quadrant pain) or signs of pancreatitis
Dose adjustment protocols: Understand when and how doses might be modified based on response and tolerability; know that testosterone should be reduced or paused if hematocrit exceeds 54% or if PSA rises >1.4 ng/mL in 12 months or exceeds 4.0 ng/mL
Discuss realistic expectations regarding outcomes. While both therapies can provide significant benefits, individual responses vary. Weight loss with tirzepatide typically occurs gradually over months, and testosterone's effects on symptoms may take several weeks to months to manifest fully. Ask about potential adverse effects of each medication and when to seek urgent medical attention—for example, severe abdominal pain (possible pancreatitis), chest pain, or sudden vision changes.
If applicable, discuss contraception, as tirzepatide can reduce the exposure to oral contraceptives; non-oral contraception or backup methods are recommended for 4 weeks after starting tirzepatide or increasing the dose.
Finally, clarify the long-term plan. Will testosterone therapy be continued indefinitely, or might it be discontinued if weight loss normalizes endogenous production? How will success be measured? What are the criteria for continuing, adjusting, or discontinuing either therapy? Establishing clear treatment goals and monitoring plans ensures safe, effective use of both medications and helps optimize your overall metabolic and hormonal health.
There is no formal contraindication to using tirzepatide and testosterone together, as they work through different mechanisms and metabolic pathways. However, combined use requires medical supervision, individualized monitoring of hormone levels, blood counts, and cardiovascular parameters, and careful assessment of each medication's risk-benefit profile.
Yes, significant weight loss from tirzepatide may increase endogenous testosterone production by reducing adipose tissue aromatase activity and improving hypothalamic-pituitary-gonadal axis function. Men on testosterone replacement therapy may require dose adjustments as weight loss progresses to avoid supraphysiological testosterone levels.
Combined therapy requires baseline and periodic monitoring of testosterone levels, hematocrit, blood glucose, HbA1c, blood pressure, and metabolic parameters. Hematocrit should be checked at 3–6 months then annually, with testosterone dose reduction if levels exceed 54%, while testosterone levels should be monitored at 3–6 months after initiation or dose changes.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.