LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Hashimoto's disease, an autoimmune thyroid condition affecting approximately 5% of Americans, often leads to hypothyroidism and challenging weight gain despite standard levothyroxine therapy. Tirzepatide, a dual GIP/GLP-1 receptor agonist FDA-approved for type 2 diabetes and chronic weight management, has generated interest for addressing metabolic complications in thyroid patients. While tirzepatide is not approved to treat Hashimoto's disease itself and does not modify the autoimmune process, it may benefit patients who meet criteria for obesity treatment. This article examines the current evidence, safety considerations, and appropriate clinical context for tirzepatide use in patients with Hashimoto's disease.
Quick Answer: Tirzepatide is not FDA-approved to treat Hashimoto's disease itself but may be used on-label for weight management in patients with Hashimoto's who meet obesity treatment criteria (BMI ≥30 or BMI ≥27 with comorbidities).
Hashimoto's disease, also known as Hashimoto's thyroiditis or chronic lymphocytic thyroiditis, is an autoimmune condition in which the immune system attacks the thyroid gland. This progressive destruction of thyroid tissue typically leads to hypothyroidism, a state of insufficient thyroid hormone production. The condition affects approximately 5% of the US population and is significantly more common in women than men, with peak incidence occurring between ages 30 and 50.
Diagnosis typically involves measuring thyroid stimulating hormone (TSH) as the first-line test, with elevated TSH and low free T4 confirming hypothyroidism. Anti-thyroid peroxidase (TPO) antibodies support the autoimmune etiology of Hashimoto's disease, though thyroid ultrasound is not routinely indicated unless nodules or goiter are present.
The thyroid gland produces hormones that regulate metabolism, energy expenditure, and numerous physiological processes throughout the body. When Hashimoto's disease causes hypothyroidism, patients commonly experience fatigue, cold intolerance, constipation, dry skin, and unintentional weight gain. This weight gain results from decreased metabolic rate and may be challenging to address with lifestyle interventions alone, even with thyroid hormone replacement therapy.
Many patients with Hashimoto's disease develop metabolic complications beyond weight gain. Studies indicate that hypothyroidism is associated with dyslipidemia (elevated LDL cholesterol and triglycerides), insulin resistance, and increased cardiovascular risk. The prevalence of metabolic syndrome—a cluster of conditions including abdominal obesity, hypertension, dyslipidemia, and impaired glucose metabolism—appears higher in individuals with hypothyroidism compared to the general population.
The intersection of autoimmune thyroid disease and metabolic dysfunction creates complex management challenges. Standard treatment with levothyroxine addresses thyroid hormone deficiency but does not directly resolve metabolic complications or facilitate weight loss in many patients. This clinical reality has prompted interest in adjunctive therapies that might address both thyroid-related and metabolic aspects of the condition, though such approaches require careful evaluation and medical supervision.
Referral to an endocrinologist is recommended for patients who are pregnant or planning pregnancy, pediatric patients, those with nodules or goiter, discordant laboratory results, persistent symptoms despite normal TSH, or suspected myxedema coma (requiring urgent care).
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for two distinct indications: type 2 diabetes mellitus (marketed as Mounjaro) and chronic weight management (marketed as Zepbound). As the first dual GIP/GLP-1 receptor agonist, tirzepatide represents a significant advancement in metabolic therapeutics, offering enhanced efficacy compared to single-pathway agents.
The medication's mechanism of action involves simultaneous activation of two incretin hormone pathways. GLP-1 receptor activation enhances glucose-dependent insulin secretion, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through central nervous system effects. GIP receptor activation complements these effects by promoting insulin secretion, while potentially improving insulin sensitivity in peripheral tissues and influencing lipid metabolism and energy expenditure, though these additional effects have more limited human data.
Tirzepatide is administered as a once-weekly subcutaneous injection, with dosing typically initiated at 2.5 mg and gradually titrated upward (5 mg, 7.5 mg, 10 mg, 12.5 mg, to a maximum of 15 mg) based on therapeutic response and tolerability. Each dose should be maintained for at least 4 weeks before considering escalation. The gradual dose escalation minimizes gastrointestinal adverse effects, which represent the most common side effects of the medication.
Clinical trials have demonstrated substantial efficacy for tirzepatide in both glycemic control and weight reduction. In the SURMOUNT clinical trial program for obesity, participants achieved average weight loss of 15-21% of body weight depending on dose, significantly exceeding results with diet and exercise alone or other available pharmacotherapies. For type 2 diabetes, the SURPASS trials demonstrated robust HbA1c reductions of 1.9-2.4 percentage points. Zepbound is specifically indicated as an adjunct to reduced-calorie diet and increased physical activity for chronic weight management in adults with BMI ≥30 kg/m² or BMI ≥27 kg/m² with at least one weight-related comorbid condition. These impressive outcomes have generated interest in potential applications beyond the approved indications, though such use requires careful consideration of evidence and safety.
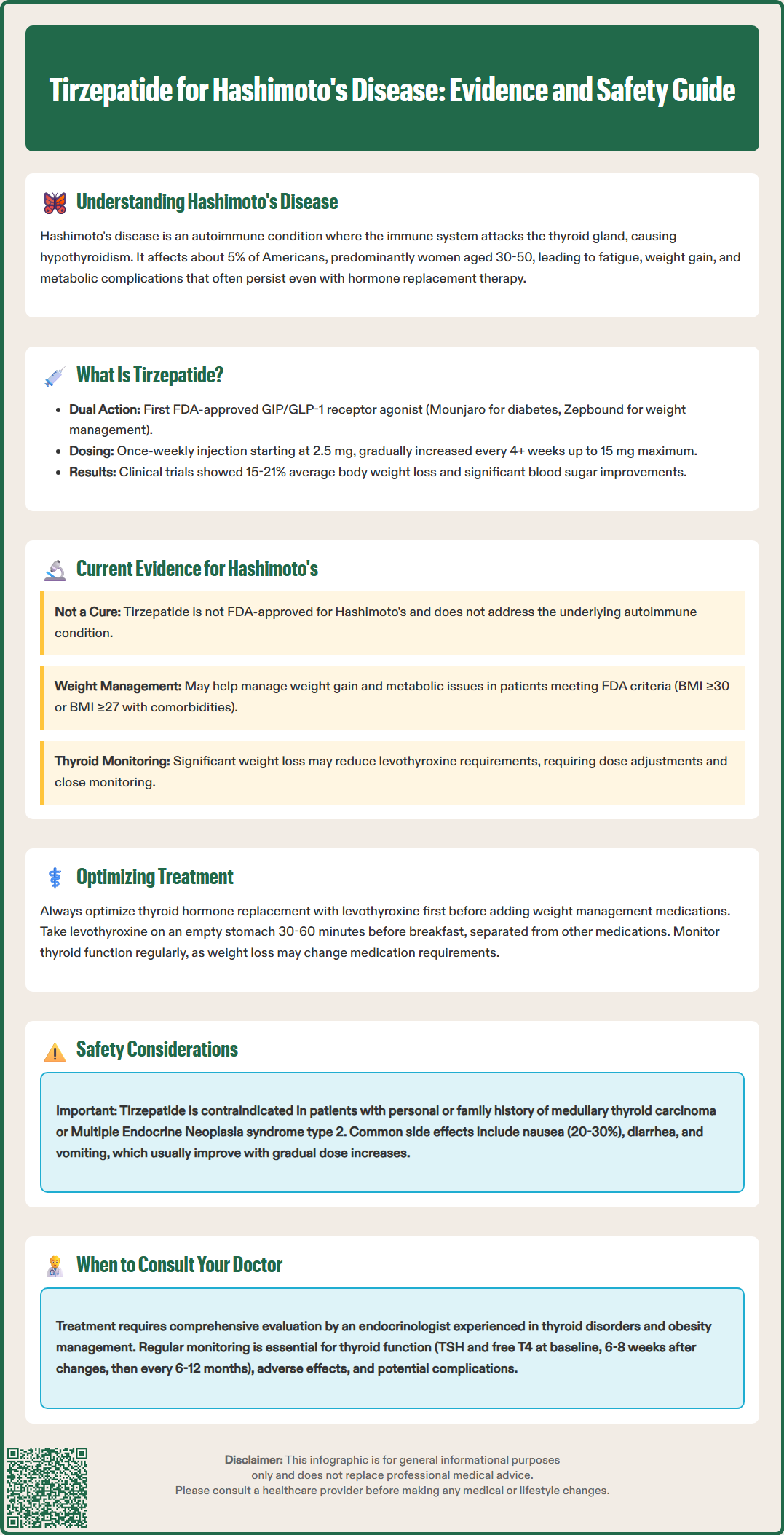
There is currently no FDA-approved indication for tirzepatide specifically for Hashimoto's disease, and no large-scale randomized controlled trials have evaluated tirzepatide as a treatment for this autoimmune thyroid condition. The existing evidence base does not establish tirzepatide as a disease-modifying therapy for Hashimoto's thyroiditis or as a treatment that directly addresses the autoimmune pathophysiology underlying the condition.
However, clinical interest exists regarding tirzepatide's potential role in managing metabolic complications that frequently accompany Hashimoto's disease. Patients with hypothyroidism secondary to Hashimoto's often struggle with weight gain and metabolic dysfunction despite adequate thyroid hormone replacement. In this context, tirzepatide may address weight management challenges in patients who meet FDA-approved criteria for obesity treatment (BMI ≥30 kg/m² or BMI ≥27 kg/m² with weight-related comorbidities), which would be an on-label use of Zepbound. Using tirzepatide solely to treat Hashimoto's disease itself would be considered off-label and requires individualized assessment.
Limited observational data and case reports suggest that GLP-1 receptor agonists do not adversely affect thyroid function in patients with pre-existing hypothyroidism who are maintained on stable levothyroxine therapy. Some preliminary evidence indicates that significant weight loss achieved through any mechanism, including pharmacotherapy, may reduce levothyroxine requirements in some patients, necessitating monitoring of thyroid function and potential dose adjustment. However, these observations do not constitute evidence that tirzepatide treats Hashimoto's disease itself.
It is essential to emphasize that tirzepatide does not replace thyroid hormone replacement therapy, does not reduce thyroid antibody levels, and does not modify the autoimmune process in Hashimoto's disease. Any consideration of tirzepatide in patients with Hashimoto's disease would be based on comorbid conditions (type 2 diabetes or obesity meeting specific criteria) rather than the thyroid condition itself. Patients should not discontinue or alter thyroid hormone replacement when using tirzepatide, and close endocrinologic supervision remains essential.
The relationship between thyroid function and weight management medications requires careful clinical consideration. Thyroid hormones profoundly influence basal metabolic rate, thermogenesis, and energy expenditure, making thyroid status a critical factor when evaluating any weight management intervention. In patients with Hashimoto's disease, optimization of thyroid hormone replacement with levothyroxine represents the foundational therapeutic step before considering additional weight management strategies.
Adequate thyroid hormone replacement should normalize TSH levels, typically targeting the laboratory reference range for most nonpregnant adults. Individualized targets may be appropriate for older adults and those with cardiovascular disease, while trimester-specific ranges should be used during pregnancy. However, even with biochemically optimized thyroid function, many patients continue to experience difficulty with weight management. This persistent challenge likely reflects multiple factors including prior metabolic adaptations, changes in body composition, lifestyle factors, and possibly residual metabolic effects not fully corrected by thyroid hormone replacement alone.
When considering adjunctive pharmacotherapy for weight management in patients with Hashimoto's disease, several principles apply. First, thyroid function must be stable and adequately treated. Second, the patient should meet established criteria for pharmacologic weight management intervention, such as BMI ≥30 kg/m² or BMI ≥27 kg/m² with weight-related comorbidities, consistent with FDA indications. Third, lifestyle modifications including nutrition counseling and physical activity should be implemented concurrently. Fourth, regular monitoring of thyroid function is necessary, as significant weight loss may alter levothyroxine requirements.
Tirzepatide and other incretin-based therapies do not directly interact with thyroid hormone replacement at a pharmacokinetic level. However, gastrointestinal effects of these medications—particularly delayed gastric emptying—could theoretically affect levothyroxine absorption if medications are taken simultaneously. Standard practice recommends taking levothyroxine on an empty stomach, 30-60 minutes before breakfast or at bedtime (at least 3-4 hours after the last meal), and separated from calcium and iron supplements by at least 4 hours. Patients should maintain consistent timing of levothyroxine administration and report any symptoms suggesting altered thyroid status, prompting laboratory reassessment.
The use of tirzepatide in patients with Hashimoto's disease requires comprehensive safety evaluation and ongoing medical supervision. While tirzepatide has demonstrated a generally favorable safety profile in clinical trials, specific considerations apply when treating patients with autoimmune thyroid disease and hypothyroidism.
The most common adverse effects of tirzepatide are gastrointestinal, including nausea (occurring in 20-30% of patients), diarrhea, vomiting, constipation, and abdominal discomfort. These effects are typically mild to moderate, dose-dependent, and tend to diminish over time. Gradual dose titration significantly reduces the incidence and severity of gastrointestinal symptoms. Patients should be counseled on strategies to minimize these effects, including eating smaller meals, avoiding high-fat foods, and maintaining adequate hydration.
Important safety considerations include:
Thyroid monitoring: Check TSH and free T4 at baseline, then 6-8 weeks after any levothyroxine dose change or substantial weight loss; once stable, recheck every 6-12 months
Hypoglycemia risk: While tirzepatide's glucose-lowering effect is glucose-dependent, patients with type 2 diabetes taking concurrent sulfonylureas or insulin require dose adjustments of these medications to prevent hypoglycemia
Pancreatitis: Acute pancreatitis has been reported with GLP-1 receptor agonists; patients should be instructed to seek immediate medical attention for severe, persistent abdominal pain; tirzepatide has not been studied in patients with a history of pancreatitis, and alternative therapy should be considered in these individuals
Gallbladder disease: Rapid weight loss increases cholelithiasis risk; patients with gallbladder disease history require careful consideration
Thyroid C-cell tumors: Tirzepatide carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies, though human relevance remains uncertain; the medication is contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2
Oral contraceptives: Tirzepatide can reduce exposure to oral contraceptives; patients should use alternative contraception for 4 weeks after initiation and each dose escalation
Pregnancy/lactation: Tirzepatide for weight management should be discontinued when pregnancy is recognized due to potential fetal risk; preconception planning is important for patients with Hashimoto's disease
Severe GI disease: Use caution or avoid in patients with severe gastrointestinal disease, including gastroparesis
Renal function: Monitor for dehydration and renal impairment if significant gastrointestinal adverse events occur
Medication interactions: Do not use concurrently with other GLP-1 receptor agonists
Patients with Hashimoto's disease considering tirzepatide should undergo comprehensive evaluation by an endocrinologist or physician experienced in managing both thyroid disorders and obesity pharmacotherapy. This evaluation should include assessment of thyroid function optimization, screening for contraindications, review of potential drug interactions, and establishment of a monitoring plan. Shared decision-making should address realistic expectations, as tirzepatide addresses metabolic and weight management aspects but does not treat the underlying autoimmune thyroid condition. Regular follow-up enables timely identification of adverse effects, adjustment of thyroid hormone replacement as needed, and assessment of therapeutic response to ensure safe, effective care.
No, tirzepatide does not treat the underlying autoimmune process of Hashimoto's disease, reduce thyroid antibodies, or replace thyroid hormone therapy. It may only address metabolic complications like obesity in patients who meet specific FDA-approved criteria for weight management.
Possibly. Significant weight loss from tirzepatide may reduce levothyroxine requirements in some patients, necessitating TSH monitoring at baseline, after substantial weight loss, and every 6-12 months once stable. Never adjust thyroid medication without physician guidance.
Tirzepatide can be used safely in patients with Hashimoto's who meet obesity treatment criteria, provided thyroid function is optimized and contraindications are excluded (personal or family history of medullary thyroid carcinoma or MEN2). Endocrinologist supervision and regular monitoring are essential.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.