LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide, marketed as Mounjaro for type 2 diabetes and Zepbound for weight management, is a dual GIP/GLP-1 receptor agonist that has transformed metabolic disease treatment. While no direct pharmacokinetic interaction exists between tirzepatide and alcohol, understanding the potential risks of combining these substances is crucial for safe diabetes management. Both can affect blood glucose regulation and gastrointestinal function through different mechanisms, creating indirect concerns that warrant careful consideration. This article examines the evidence on tirzepatide interaction with alcohol, potential side effects, and practical guidelines for patients.
Quick Answer: Tirzepatide has no direct pharmacokinetic interaction with alcohol, but combining them increases risks of hypoglycemia and gastrointestinal side effects.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide represents a significant advancement in metabolic disease therapy due to its dual incretin receptor activity.
The medication works through multiple complementary mechanisms to improve glycemic control and promote weight loss. As a GLP-1 receptor agonist, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. The additional GIP receptor agonism may potentially further enhance insulin secretion and contribute to improved metabolic effects, though the exact mechanisms remain under investigation. These combined actions result in improved postprandial and fasting glucose levels without significantly increasing hypoglycemia risk when used as monotherapy.
Tirzepatide is administered once weekly via subcutaneous injection, with doses typically starting at 2.5 mg and gradually titrating up to a maximum of 15 mg depending on therapeutic indication and patient tolerance. The medication demonstrates dose-dependent efficacy for both glycemic control and weight reduction. Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and decreased appetite, which typically diminish over time.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Tirzepatide is not indicated for use in type 1 diabetes. When used with insulin or sulfonylureas, the risk of hypoglycemia increases significantly. Understanding these mechanisms and safety considerations is essential when considering potential interactions with other substances, including alcohol.
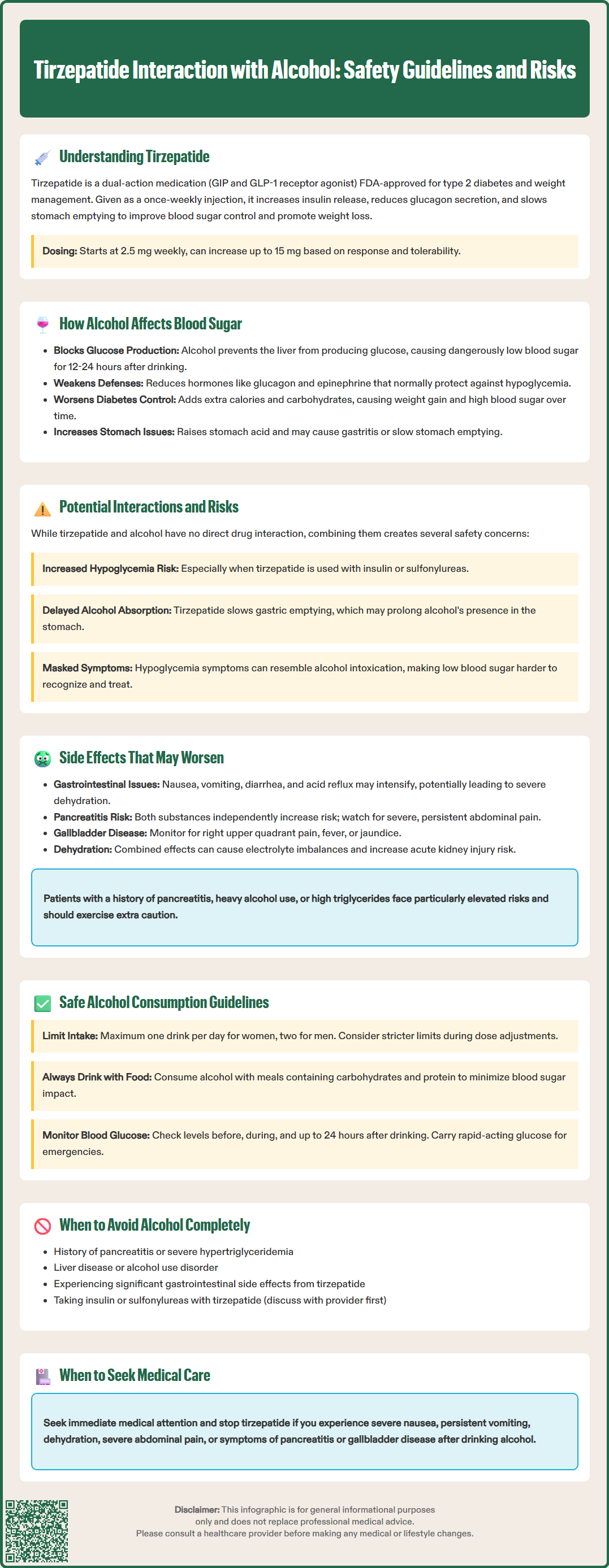
Alcohol consumption has complex and sometimes contradictory effects on glucose metabolism that are particularly relevant for individuals with diabetes. Ethanol metabolism occurs primarily in the liver, where it interferes with gluconeogenesis—the process by which the liver produces glucose from non-carbohydrate sources. This inhibition can lead to delayed hypoglycemia, particularly in individuals taking glucose-lowering medications or those with depleted glycogen stores from fasting or exercise.
The timing and pattern of alcohol's effects on blood glucose are dose-dependent and influenced by nutritional status. Moderate alcohol consumption with food may have minimal immediate impact on blood glucose levels, while drinking on an empty stomach or consuming larger quantities significantly increases hypoglycemia risk. This risk can persist for up to 12-24 hours after alcohol consumption as hepatic glucose production remains suppressed. Additionally, alcohol impairs the body's counter-regulatory response to hypoglycemia, blunting the release of hormones like glucagon and epinephrine that normally raise blood glucose during hypoglycemic episodes. Importantly, alcohol-induced depletion of liver glycogen can reduce the effectiveness of glucagon as an emergency treatment for severe hypoglycemia.
Beyond acute glucose effects, chronic alcohol use can worsen diabetes management through multiple pathways. Alcoholic beverages often contain significant calories and carbohydrates that can contribute to weight gain and hyperglycemia. Alcohol may reduce medication adherence, impair judgment regarding dietary choices, and interfere with self-monitoring behaviors. The American Diabetes Association (ADA) recognizes these risks and provides specific guidance for alcohol consumption in diabetes management.
Alcohol also affects gastrointestinal function, increasing gastric acid secretion and potentially causing gastritis or delayed gastric emptying. These effects may overlap with the gastrointestinal side effects of diabetes medications, creating additive discomfort. Understanding these multifaceted interactions is crucial when considering alcohol use alongside any diabetes therapy, including tirzepatide.
There is no official direct pharmacokinetic interaction between tirzepatide and alcohol documented in the FDA prescribing information or clinical trial data. Tirzepatide is a peptide medication that is not metabolized by hepatic cytochrome P450 enzymes, and alcohol does not directly alter tirzepatide's pharmacokinetics or its binding to GIP and GLP-1 receptors. However, the absence of a direct drug-drug interaction does not mean that combining tirzepatide with alcohol is without risk—several indirect pharmacodynamic concerns warrant careful consideration.
The primary concern involves the combined effects of both substances on blood glucose regulation. While tirzepatide has a low intrinsic risk of hypoglycemia when used alone due to its glucose-dependent mechanism, this risk increases when combined with other factors that lower blood glucose, including alcohol. According to the FDA prescribing information, patients taking tirzepatide alongside insulin or sulfonylureas face particularly elevated hypoglycemia risk when consuming alcohol, as these medications do not have glucose-dependent action. The delayed gastric emptying caused by tirzepatide may theoretically alter alcohol absorption patterns, potentially slowing the rate of alcohol absorption, though the clinical significance of this effect remains unclear and unstudied.
Gastrointestinal tolerability represents another important consideration. Both tirzepatide and alcohol can cause nausea, vomiting, and gastrointestinal distress. The delayed gastric emptying induced by tirzepatide may prolong alcohol's presence in the stomach, potentially intensifying gastrointestinal symptoms or increasing alcohol's local irritant effects on the gastric mucosa. Some patients report that alcohol consumption while taking GLP-1 receptor agonists results in more pronounced or prolonged nausea compared to their experience before starting the medication.
Additionally, alcohol's effects on judgment and symptom recognition may be particularly problematic for patients on tirzepatide. Hypoglycemia symptoms can mimic alcohol intoxication, potentially leading to delayed recognition and treatment of low blood glucose. This overlap in symptoms creates a safety concern, especially in social situations where others might attribute concerning symptoms to alcohol consumption rather than recognizing a medical emergency.
Several adverse effects associated with tirzepatide therapy may be exacerbated by concurrent alcohol consumption, creating additive or synergistic discomfort and potential health risks. The most commonly reported and clinically significant overlapping effects involve the gastrointestinal system, metabolic disturbances, and central nervous system symptoms.
Gastrointestinal effects represent the most frequent concern when combining tirzepatide with alcohol:
Nausea and vomiting: Both substances independently cause nausea through different mechanisms—tirzepatide through delayed gastric emptying and central GLP-1 receptor activation, and alcohol through direct gastric irritation and central effects. Combined use may result in severe nausea that interferes with adequate nutrition and hydration.
Diarrhea and abdominal discomfort: Alcohol can accelerate intestinal transit and cause osmotic diarrhea, while tirzepatide commonly causes diarrhea (rates vary by dose, ranging from approximately 7-17% in clinical trials). The combination may lead to more frequent or severe diarrhea with associated dehydration risk.
Gastritis and gastroesophageal reflux: Alcohol increases gastric acid secretion and can damage the gastric mucosa, while delayed gastric emptying from tirzepatide may worsen reflux symptoms.
Gallbladder disease is another important consideration. Tirzepatide has been associated with an increased risk of gallbladder adverse events, including cholelithiasis and cholecystitis. Patients should be alert to symptoms such as right upper quadrant pain, fever, or jaundice, which warrant prompt medical evaluation.
Metabolic complications include hypoglycemia as previously discussed, but also extend to dehydration and electrolyte disturbances. Both alcohol and tirzepatide-induced gastrointestinal symptoms can lead to reduced fluid intake and increased losses, creating compounded dehydration risk. This is particularly concerning given that dehydration may increase the risk of acute kidney injury, a rare but serious adverse effect associated with severe gastrointestinal reactions to GLP-1 receptor agonists.
Pancreatitis risk deserves special mention. The FDA label includes pancreatitis as a potential risk with tirzepatide. Alcohol is a well-established independent risk factor for both acute and chronic pancreatitis. Patients with a history of pancreatitis, heavy alcohol use, or hypertriglyceridemia may face elevated risk when combining these exposures, though definitive evidence of synergistic risk is lacking. Patients should be counseled to discontinue tirzepatide and seek immediate medical attention for severe, persistent abdominal pain that may indicate pancreatitis.
For patients taking tirzepatide who choose to consume alcohol, following evidence-based guidelines can help minimize risks while maintaining diabetes management goals. The American Diabetes Association provides general recommendations for alcohol consumption in diabetes that apply to patients on tirzepatide, with some additional considerations specific to GLP-1 receptor agonist therapy.
General alcohol limits for adults with diabetes include no more than one drink per day for women and up to two drinks per day for men, where one drink equals 12 oz beer, 5 oz wine, or 1.5 oz distilled spirits (per CDC and NIAAA definitions). However, patients taking tirzepatide, particularly those new to the medication or experiencing gastrointestinal side effects, may benefit from more conservative limits or temporary abstinence during dose titration periods when side effects are typically most pronounced.
Practical safety strategies include:
Never drink on an empty stomach: Always consume alcohol with food containing carbohydrates and protein to help stabilize blood glucose and reduce gastrointestinal irritation.
Monitor blood glucose carefully: Check blood glucose before drinking, periodically during alcohol consumption, before bed, and the following morning, as hypoglycemia risk persists for up to 24 hours.
Carry rapid-acting glucose: Always have glucose tablets or gel available to treat hypoglycemia, and remember that glucagon emergency kits may be less effective after alcohol consumption due to depleted liver glycogen.
Wear medical identification: Ensure medical alert jewelry or identification clearly indicates diabetes and current medications, as hypoglycemia symptoms can be mistaken for intoxication.
Avoid binge drinking: Large quantities of alcohol significantly increase hypoglycemia risk and gastrointestinal distress.
Stay hydrated: Alternate alcoholic beverages with water to maintain hydration and potentially reduce gastrointestinal symptoms.
Consider a bedtime snack: If consuming alcohol in the evening, a protein and carbohydrate-containing snack before sleep may help prevent nocturnal hypoglycemia.
When to avoid alcohol completely: Certain situations warrant complete alcohol abstinence, including history of pancreatitis, severe hypertriglyceridemia (triglycerides >500 mg/dL), active liver disease, history of alcohol use disorder, pregnancy, or when experiencing significant gastrointestinal side effects from tirzepatide. Tirzepatide is not recommended during pregnancy, and alcohol should be avoided completely during pregnancy. Patients taking insulin or sulfonylureas alongside tirzepatide face substantially elevated hypoglycemia risk and should discuss alcohol use extensively with their healthcare provider.
Clinical follow-up: Patients should discuss their alcohol consumption patterns openly with their healthcare team. Providers can assess individual risk factors, adjust diabetes management strategies accordingly, and provide personalized guidance. Any concerning symptoms following alcohol consumption—including severe nausea, persistent vomiting, signs of dehydration, or symptoms suggestive of pancreatitis or gallbladder disease—warrant prompt medical evaluation and discontinuation of tirzepatide until assessed by a healthcare provider. While moderate alcohol consumption may be compatible with tirzepatide therapy for many patients, individualized assessment and ongoing monitoring remain essential for safe use.
Moderate alcohol consumption may be acceptable for some patients taking tirzepatide, following ADA guidelines of no more than one drink per day for women and two for men. However, alcohol increases risks of hypoglycemia and gastrointestinal side effects, so it should always be consumed with food and with careful blood glucose monitoring.
There is no direct pharmacokinetic interaction between tirzepatide and alcohol documented in FDA prescribing information. However, indirect pharmacodynamic concerns exist, including increased hypoglycemia risk and worsened gastrointestinal symptoms when the two substances are combined.
The primary risks include delayed hypoglycemia (low blood sugar) lasting up to 24 hours, intensified gastrointestinal symptoms such as nausea and vomiting, dehydration, and potentially increased risk of pancreatitis. Patients taking insulin or sulfonylureas alongside tirzepatide face particularly elevated hypoglycemia risk.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.