LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is an FDA-approved dual GIP and GLP-1 receptor agonist used for type 2 diabetes and chronic weight management. While gastrointestinal side effects like nausea and dyspepsia are well-documented, many patients wonder: does tirzepatide cause GERD? The relationship between this medication and gastroesophageal reflux disease remains incompletely understood. Although GERD is not prominently featured in FDA labeling, some patients report new or worsening reflux symptoms during treatment. Understanding this potential connection, along with effective management strategies, helps patients and healthcare providers make informed treatment decisions.
Quick Answer: Tirzepatide may cause or worsen GERD in some patients, though the relationship is not fully established and GERD is not prominently featured in FDA labeling.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. This medication works by enhancing insulin secretion, suppressing glucagon release, and slowing gastric emptying—mechanisms that contribute to improved glycemic control and significant weight loss. Notably, the gastric emptying effect tends to attenuate over time with continued dosing.
Gastrointestinal side effects are among the most commonly reported adverse reactions with tirzepatide therapy. Clinical trials have documented that nausea, diarrhea, vomiting, constipation, dyspepsia, eructation (belching), and abdominal discomfort occur frequently, particularly during dose initiation and escalation. These effects are generally mild to moderate in severity and tend to diminish over time as patients develop tolerance to the medication.
Understanding the full spectrum of potential digestive effects is essential for both healthcare providers and patients, as it allows for appropriate counseling, expectation management, and timely intervention when symptoms become problematic. While many gastrointestinal effects are well-characterized, questions remain about tirzepatide's relationship with gastroesophageal reflux disease (GERD), a condition affecting millions of Americans and characterized by the backward flow of stomach acid into the esophagus.
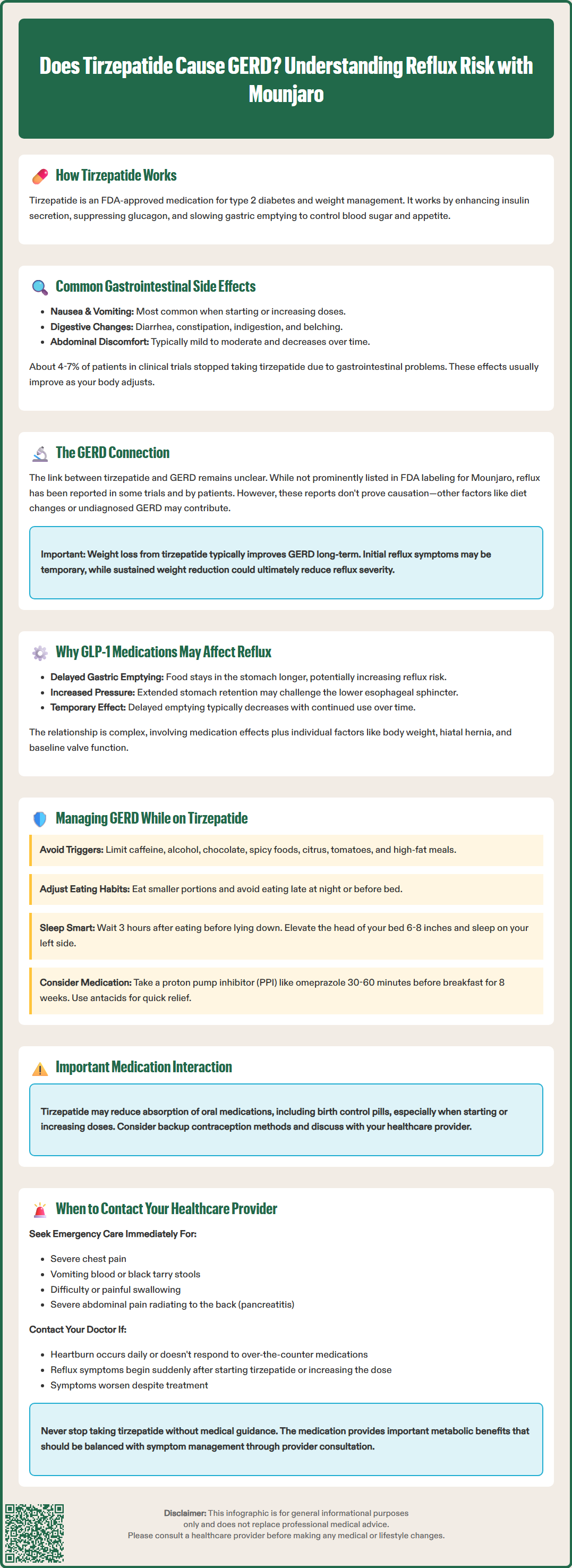
The relationship between tirzepatide and GERD is not fully established. While gastroesophageal reflux disease is not prominently featured in the FDA-approved prescribing information for Mounjaro, it has been reported as an adverse reaction in some clinical trials for Zepbound. Dyspepsia (indigestion), which can include reflux-like symptoms, is listed among the common adverse reactions in the product labeling.
Some patients and healthcare providers have reported experiences of new-onset or worsening reflux symptoms during tirzepatide therapy. These reports warrant attention, though they must be interpreted cautiously as postmarketing experiences with unknown incidence and potential confounding factors. It is important to recognize that correlation does not equal causation, and multiple factors may contribute to reflux symptoms in patients taking tirzepatide, including dietary changes, concurrent medications, or pre-existing but undiagnosed GERD.
Interestingly, weight loss generally reduces GERD severity over time, so while early GI effects of tirzepatide may transiently worsen symptoms, long-term weight reduction might ultimately improve reflux for many patients.
The American Diabetes Association (ADA) Standards of Care and American College of Physicians (ACP) guidelines do not specifically address GERD as a contraindication for GLP-1 or dual agonist therapy, though the ADA does caution about use in patients with severe gastrointestinal disease. Patients with pre-existing GERD are not automatically excluded from tirzepatide treatment, though individualized assessment is always appropriate. Healthcare providers should maintain awareness that while tirzepatide does not carry a formal GERD warning, gastrointestinal effects are common with this medication class, and reflux symptoms may emerge or change during treatment.
The pharmacological mechanism of tirzepatide and other GLP-1 receptor agonists provides a theoretical basis for understanding potential effects on gastroesophageal reflux. These medications significantly delay gastric emptying—the rate at which food moves from the stomach into the small intestine. This delayed emptying is therapeutically beneficial for glucose control and satiety, but it also means that stomach contents remain present for longer periods, potentially increasing the opportunity for reflux to occur.
When the stomach retains food and digestive fluids for extended periods, intragastric pressure may hypothetically increase, particularly after meals. This increased pressure could potentially challenge the lower esophageal sphincter (LES)—the muscular valve that normally prevents stomach contents from flowing backward into the esophagus. It's important to note that this mechanism is theoretical in the context of tirzepatide, as direct studies examining its effect on LES function are limited.
Additionally, the delayed gastric emptying effect of tirzepatide typically attenuates over time with continued dosing, which may explain why some patients experience improvement in initial reflux symptoms with ongoing treatment.
The relationship between GLP-1 medications and reflux is likely multifactorial, involving direct pharmacological effects on gastric motility and individual patient susceptibility factors including body weight, hiatal hernia presence, and baseline LES function. Changes in meal patterns and food choices that often accompany tirzepatide therapy may also influence reflux symptoms. The net impact on GERD may vary considerably between patients, and the current evidence base remains limited.
Patients experiencing reflux symptoms while taking tirzepatide can implement several evidence-based lifestyle modifications to reduce discomfort. Dietary adjustments are often the first line of management and include avoiding known reflux triggers such as caffeine, alcohol, chocolate, spicy foods, citrus, tomato-based products, and high-fat meals. Eating smaller portions rather than large meals can help minimize gastric distension and reduce reflux risk. Avoiding late meals and nighttime snacking is particularly important.
Timing and positioning strategies are equally important. Patients should avoid lying down for at least three hours after eating, allowing adequate time for partial gastric emptying even with medication-induced delay. Elevating the head of the bed by 6-8 inches (using bed risers, not just pillows) can help prevent nighttime reflux by using gravity to keep stomach contents in place. Sleeping on the left side may also reduce reflux episodes compared to right-side sleeping.
Pharmacological management follows a stepwise approach aligned with American College of Gastroenterology guidelines. For typical GERD symptoms without alarm features, an 8-week trial of a once-daily proton pump inhibitor (PPI) such as omeprazole or esomeprazole is recommended, taken 30-60 minutes before breakfast. If symptoms are only partially controlled, twice-daily PPI dosing or switching to an alternative PPI may be considered. Over-the-counter antacids (calcium carbonate, magnesium hydroxide) can provide rapid but short-term relief for breakthrough symptoms. H2-receptor antagonists (famotidine, cimetidine) offer intermediate acid suppression and can be used as needed or regularly.
Patients should be aware that tirzepatide may temporarily reduce the absorption of oral medications, including oral contraceptives, particularly during dose initiation and escalation. Alternative contraception methods should be considered during this period.
Patients should discuss any new or worsening reflux symptoms with their healthcare provider rather than self-managing indefinitely. The provider can assess whether symptoms represent true GERD requiring investigation, whether tirzepatide dose adjustment might be beneficial, or whether the medication should be continued given the overall risk-benefit profile for the individual patient.
While mild, occasional reflux symptoms may be manageable with lifestyle modifications, certain warning signs require prompt medical evaluation. Patients should contact their healthcare provider if they experience severe or persistent heartburn that does not respond to over-the-counter medications, occurs daily, or significantly impacts quality of life. Reflux symptoms that worsen progressively despite treatment warrant reassessment of the diagnosis and management approach.
Alarm symptoms that require urgent evaluation include difficulty swallowing (dysphagia), painful swallowing (odynophagia), unintentional weight loss beyond expected therapeutic weight reduction, persistent vomiting, evidence of gastrointestinal bleeding (black tarry stools, vomiting blood or coffee-ground material), or severe chest pain. For severe chest pain or significant GI bleeding, patients should seek emergency care or call 911 immediately. These symptoms may indicate complications such as esophagitis, stricture, Barrett's esophagus, or other serious conditions that require endoscopic evaluation and specialized management.
Patients should also be aware of warning signs related to other potential tirzepatide side effects. Severe, persistent abdominal pain that may radiate to the back could indicate pancreatitis, while right upper quadrant pain, fever, or yellowing of the skin/eyes may suggest gallbladder disease—both are noted in the FDA warnings for tirzepatide. Signs of dehydration (dizziness, reduced urination) with persistent vomiting or diarrhea also warrant prompt medical attention.
Patients should inform their provider if reflux symptoms develop suddenly after starting tirzepatide or following dose escalation, as this temporal relationship may inform treatment decisions. Healthcare providers may consider dose adjustment, temporary dose reduction, or additional investigation including upper endoscopy if clinically indicated. In some cases, switching to an alternative diabetes or weight management medication may be appropriate if GERD symptoms are severe and refractory to standard management.
It is essential that patients do not discontinue tirzepatide abruptly without medical guidance, as this medication provides important metabolic benefits for diabetes control and weight management. A collaborative discussion between patient and provider can identify the optimal balance between managing reflux symptoms and maintaining the therapeutic benefits of tirzepatide therapy.
Patients with pre-existing GERD are not automatically excluded from tirzepatide treatment, though individualized assessment is appropriate. The FDA does not list GERD as a contraindication, but cautions against use in patients with severe gastrointestinal disease.
Many gastrointestinal side effects of tirzepatide, including reflux symptoms, tend to diminish over time as patients develop tolerance. Additionally, the delayed gastric emptying effect attenuates with continued dosing, and long-term weight loss may ultimately improve GERD severity.
Proton pump inhibitors (omeprazole, esomeprazole) taken 30-60 minutes before breakfast are first-line treatment for GERD symptoms. H2-receptor antagonists (famotidine) and over-the-counter antacids can provide additional or breakthrough relief as needed.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.