LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
When does tirzepatide kick in? Most patients notice initial effects within the first few weeks of treatment, though the timeline varies between blood sugar control and weight loss. Tirzepatide, a dual GIP and GLP-1 receptor agonist approved by the FDA as Mounjaro for type 2 diabetes and Zepbound for chronic weight management, typically improves fasting blood glucose within 1-2 weeks. Substantial weight loss generally becomes apparent after 3-6 months of consistent use. Understanding this timeline helps set realistic expectations as you begin therapy with this once-weekly injectable medication.
Quick Answer: Tirzepatide typically improves blood glucose within 1-2 weeks, while noticeable weight loss generally occurs after 3-6 months of treatment.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound) in adults. This medication represents a novel approach to metabolic regulation by targeting two incretin hormone pathways simultaneously.
The drug's mechanism of action involves binding to GIP and GLP-1 receptors throughout the body, including pancreatic beta cells, which stimulates insulin secretion in a glucose-dependent manner. This means insulin release occurs primarily when blood glucose levels are elevated, reducing the risk of hypoglycemia compared to some other diabetes medications. Tirzepatide also suppresses glucagon secretion from pancreatic alpha cells, further contributing to improved glycemic control.
Beyond glucose regulation, tirzepatide significantly affects appetite and gastric emptying. The medication acts on receptors in the brain to reduce hunger signals and increase satiety, while simultaneously slowing the rate at which food leaves the stomach. These combined effects lead to reduced caloric intake and subsequent weight loss. The drug is administered once weekly via subcutaneous injection, with dosing typically starting at 2.5 mg and gradually increasing every 4 weeks as tolerated through 5 mg, 7.5 mg, 10 mg, 12.5 mg, to a maximum of 15 mg based on individual response and tolerability.
Tirzepatide's dual receptor activity distinguishes it from single GLP-1 receptor agonists. In clinical trials, tirzepatide demonstrated greater A1c reduction and weight loss compared to semaglutide 1 mg, though individual responses vary considerably. Tirzepatide is not indicated for type 1 diabetes or for use in pediatric patients.
Understanding when tirzepatide begins to produce measurable effects requires distinguishing between its impact on blood glucose levels and weight loss, as these outcomes follow different timelines.
Blood Sugar Improvements: Glycemic effects typically emerge within the first few weeks of treatment. Most patients notice improved fasting blood glucose readings within 1-2 weeks of starting tirzepatide, though optimal glycemic control generally develops over 8-12 weeks. According to the FDA label, steady-state plasma concentrations are achieved after approximately 4 weeks at a given dose. Hemoglobin A1c reductions—the standard measure of long-term glucose control—become clinically significant after 12 weeks of therapy, with continued improvement through 24 weeks. In the SURPASS clinical trials for type 2 diabetes, patients achieved A1c reductions ranging from 1.9% to 2.4% at the highest doses by week 40.
Weight Loss Progression: Weight reduction follows a more gradual trajectory. Initial weight loss may be noticeable within 4-8 weeks, but substantial changes typically require 3-6 months of treatment. In the SURMOUNT-1 trial for weight management, participants lost an average of 5% of their body weight by approximately 12 weeks, with continued weight loss occurring through 72 weeks. At the maximum 15 mg dose, participants achieved average weight reductions of 20-22% of baseline body weight.
It is important to recognize that these timelines represent population averages. Individual responses vary based on baseline metabolic status, adherence to lifestyle modifications, concurrent medications, and other factors. The gastric-emptying effect of tirzepatide may attenuate somewhat with chronic use, which can influence early versus later glycemic effects. Healthcare providers typically reassess A1c every 3 months per American Diabetes Association guidelines.
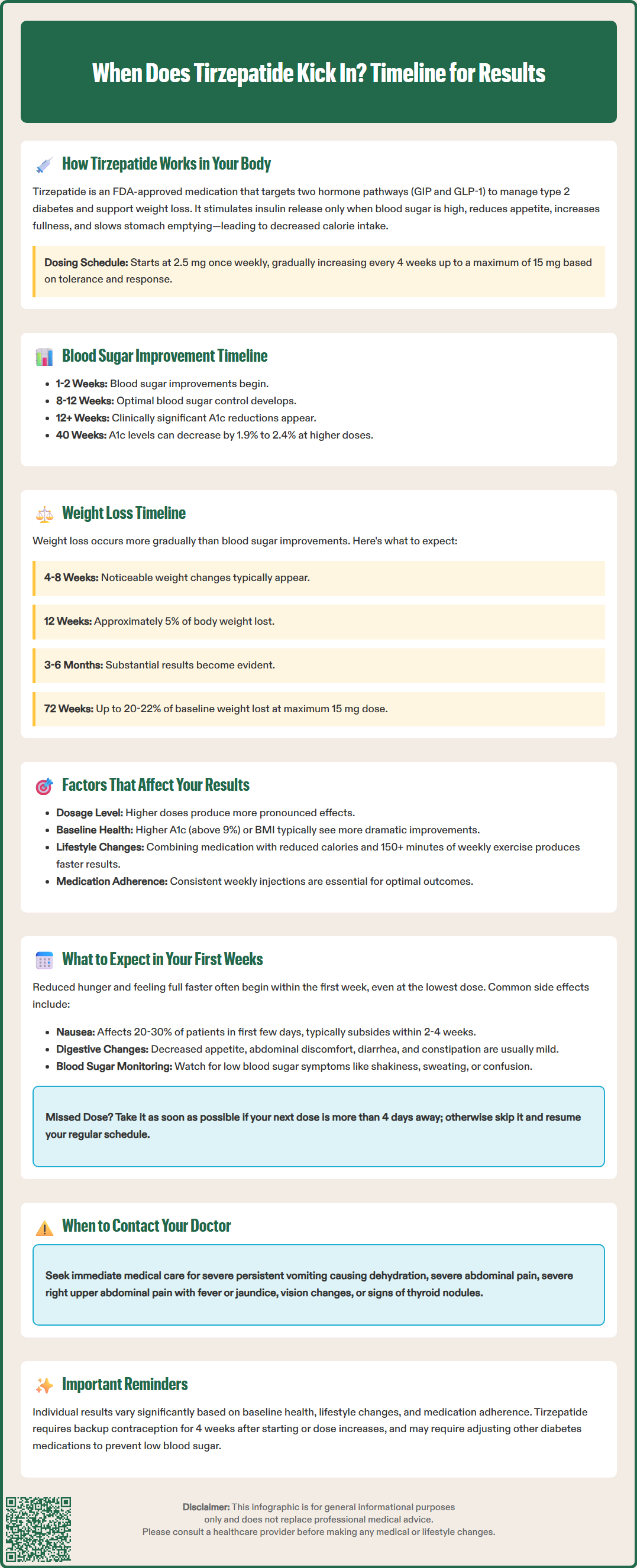
Multiple variables influence the speed and magnitude of tirzepatide's therapeutic effects, making individual responses highly variable.
Dosing Schedule: Tirzepatide follows a gradual dose-escalation protocol to minimize gastrointestinal adverse effects. Treatment begins at 2.5 mg weekly for four weeks, then increases to 5 mg. Further increases to 7.5 mg, 10 mg, 12.5 mg, and 15 mg typically occur at four-week intervals if additional glycemic control or weight loss is needed and if tolerated. This stepwise approach means patients on lower maintenance doses may experience slower or less pronounced effects than those reaching higher therapeutic doses.
Baseline Metabolic Status: Patients with higher baseline A1c levels (above 9%) often demonstrate more dramatic absolute reductions in blood glucose, though percentage improvements may be similar across groups. Similarly, individuals with higher starting body mass index (BMI) may lose more absolute weight, though percentage weight loss tends to be comparable. Insulin resistance severity and beta-cell function also influence glycemic response rates.
Lifestyle Modifications: Diet quality and physical activity significantly impact outcomes. Patients who combine tirzepatide with reduced caloric intake and regular exercise typically achieve faster and more substantial results than those relying on medication alone. The American Diabetes Association recommends at least 150 minutes of moderate-intensity aerobic activity weekly alongside medical therapy.
Medication Interactions: Tirzepatide delays gastric emptying, which can affect the absorption of oral medications. Patients taking oral contraceptives should use a backup method for 4 weeks after starting tirzepatide and after each dose increase, or consider using a non-oral contraceptive method. Other diabetes medications, particularly insulin or sulfonylureas, may require dose reductions when initiating tirzepatide to prevent hypoglycemia.
Individual Physiological Factors: Age, sex, and renal function may contribute to response variability. No dose adjustment is required for any degree of renal impairment, including end-stage renal disease, though patients should be monitored for dehydration and acute kidney injury. Similarly, no dose adjustment is needed for hepatic impairment.
The initial weeks of tirzepatide therapy represent an adjustment period during which patients should anticipate both therapeutic effects and potential adverse reactions.
Common Early Experiences: Gastrointestinal symptoms are the most frequently reported adverse effects during treatment initiation. Nausea affects approximately 20-30% of patients, typically emerging within days of the first injection and often diminishing over 2-4 weeks as tolerance develops. Other common symptoms include decreased appetite, mild abdominal discomfort, occasional diarrhea, and constipation. These effects are generally mild to moderate in severity and rarely require treatment discontinuation.
Many patients notice reduced hunger and earlier satiety within the first week, even at the 2.5 mg starter dose. This appetite suppression often becomes more pronounced as the dose increases. Some individuals report feeling fuller after smaller meals and experiencing fewer cravings for high-calorie foods.
Monitoring and Safety Considerations: Patients should monitor blood glucose levels as directed by their healthcare provider, particularly if taking other diabetes medications. Signs of hypoglycemia—including shakiness, sweating, confusion, or rapid heartbeat—warrant immediate glucose intake and medical consultation. Regular weight tracking and blood pressure monitoring are advisable, as weight loss may necessitate adjustments to antihypertensive medications.
People with diabetes and pre-existing diabetic retinopathy should be monitored closely, as rapid improvement in blood glucose can temporarily worsen retinopathy. If you miss a dose and the next scheduled dose is more than 4 days away, take the missed dose as soon as possible. If less than 4 days remain, skip the missed dose and take the next dose on the regular schedule.
When to Seek Medical Advice: Patients should contact their healthcare provider immediately for severe or persistent nausea and vomiting leading to dehydration, severe abdominal pain (which may indicate pancreatitis), or severe right upper abdominal pain with or without fever, yellowing of skin/eyes (possible gallbladder disease). Visual changes or signs of thyroid nodules also warrant prompt medical attention. While tirzepatide carries a boxed warning regarding thyroid C-cell tumors based on rodent studies, there is no established link to medullary thyroid carcinoma in humans. Nevertheless, the medication is contraindicated in patients with a personal or family history of this condition or Multiple Endocrine Neoplasia syndrome type 2.
Tirzepatide is not recommended during pregnancy or breastfeeding. Patience and consistent adherence are essential during the initial treatment phase. Most patients find that side effects diminish significantly after the first month, while therapeutic benefits continue to accumulate over subsequent months.
Most patients notice improved fasting blood glucose within 1-2 weeks of starting tirzepatide, with optimal glycemic control developing over 8-12 weeks. Clinically significant A1c reductions typically occur after 12 weeks of therapy.
Initial weight loss may be noticeable within 4-8 weeks, but substantial changes typically require 3-6 months of treatment. Clinical trials showed patients lost an average of 5% body weight by approximately 12 weeks, with continued weight loss through 72 weeks.
Gastrointestinal symptoms are most common, with nausea affecting 20-30% of patients within days of the first injection. These effects, along with decreased appetite and mild abdominal discomfort, typically diminish over 2-4 weeks as tolerance develops.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.