LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide, a dual GIP and GLP-1 receptor agonist approved by the FDA for type 2 diabetes (Mounjaro) and chronic weight management (Zepbound), may indirectly affect menstrual cycles in some women. While tirzepatide does not directly target reproductive hormones, the significant weight loss and metabolic changes it produces can influence the hypothalamic-pituitary-ovarian axis that regulates menstruation. Women taking tirzepatide have reported changes in cycle timing, flow intensity, and menstrual regularity. Understanding this connection helps women anticipate potential reproductive health changes during treatment and recognize when medical evaluation is needed.
Quick Answer: Tirzepatide may indirectly affect menstrual cycles through significant weight loss and metabolic changes that influence reproductive hormone balance, though it does not directly target menstrual function.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). While the medication does not directly target reproductive hormones, some women have reported menstrual cycle changes after starting treatment.
The relationship between tirzepatide and menstrual irregularities is primarily indirect, mediated through significant weight loss and metabolic improvements. As tirzepatide promotes substantial weight reduction—clinical trials such as SURMOUNT-1 demonstrated average weight loss of approximately 20.9% of body weight at the 15 mg dose in adults without diabetes—this metabolic shift can influence the hypothalamic-pituitary-ovarian axis that regulates menstruation. Women may experience changes in cycle length, flow intensity, or timing of periods.
Menstrual changes that have been anecdotally reported include:
Irregular cycle timing or missed periods
Heavier or lighter menstrual flow
Changes in premenstrual symptoms
Breakthrough bleeding between periods
It is important to note that there is no official direct link established between tirzepatide's pharmacological mechanism and menstrual function. The FDA prescribing information does not list menstrual irregularities as a specific adverse effect. However, the metabolic and hormonal shifts accompanying rapid weight loss can affect reproductive function in women of childbearing age. Women with underlying conditions such as polycystic ovary syndrome (PCOS) may experience different patterns of menstrual changes, sometimes including cycle normalization as insulin resistance improves.
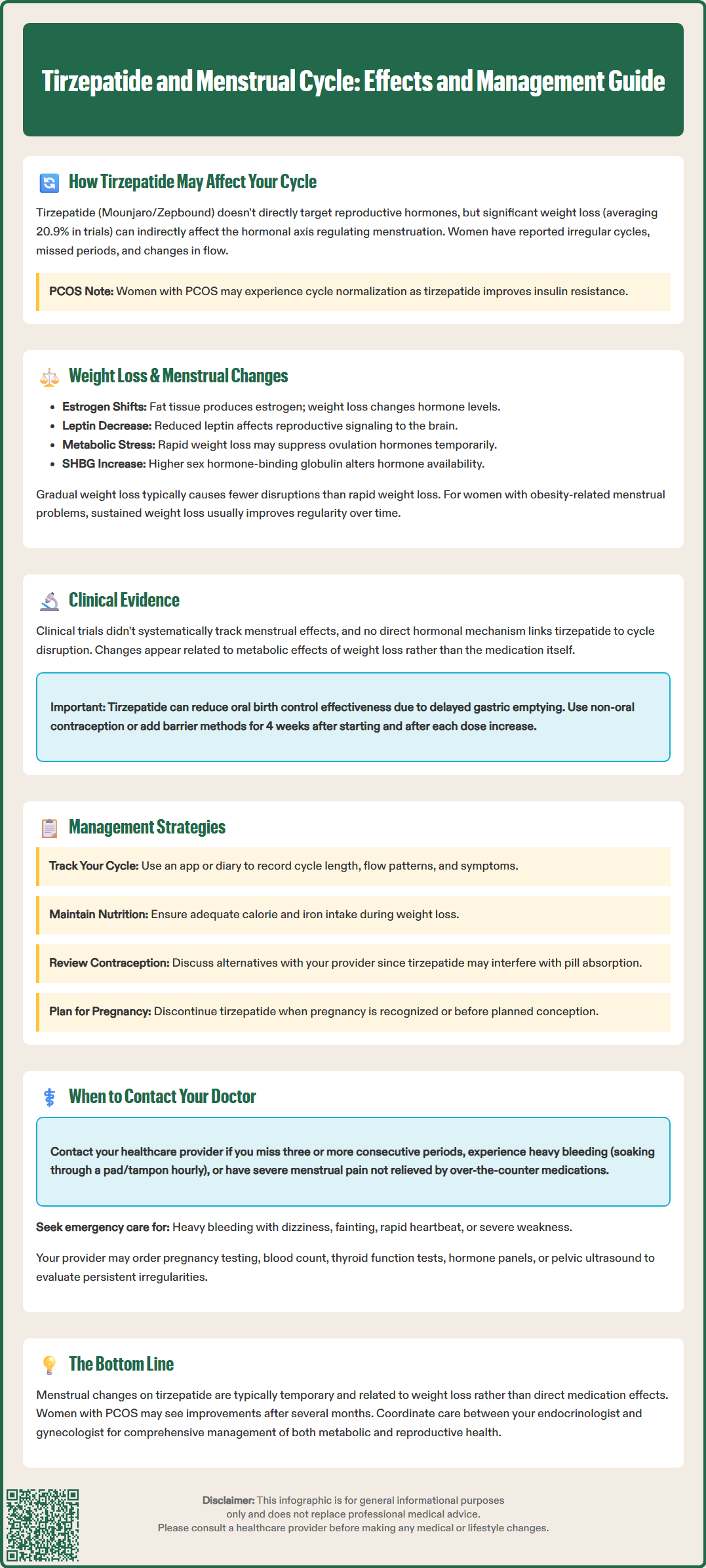
Weight loss, regardless of the method achieved, can significantly impact menstrual regularity through multiple physiological pathways. Adipose tissue functions as an endocrine organ, producing estrogen through the aromatization of androgens. When substantial fat loss occurs, circulating estrogen levels may fluctuate, temporarily disrupting the delicate hormonal balance required for regular ovulation and menstruation.
The hypothalamic-pituitary-ovarian axis is particularly sensitive to energy availability and metabolic status. Rapid weight reduction can signal energy deficit to the hypothalamus, potentially suppressing gonadotropin-releasing hormone (GnRH) pulsatility. This suppression may lead to reduced luteinizing hormone (LH) and follicle-stimulating hormone (FSH) secretion, affecting ovulation timing and menstrual predictability. These changes represent the body's adaptive response to perceived metabolic stress.
Metabolic factors influencing menstrual function during weight loss:
Leptin levels: This adipocyte-derived hormone decreases with fat loss and plays a crucial role in reproductive function signaling
Insulin sensitivity: Improved insulin sensitivity can normalize androgen levels, particularly beneficial in PCOS
Inflammatory markers: Reduction in chronic low-grade inflammation associated with obesity
Sex hormone-binding globulin (SHBG): Levels typically increase with weight loss, affecting free hormone availability
For women with obesity-related reproductive dysfunction, particularly those with PCOS, moderate and sustained weight loss often improves menstrual regularity over time. However, the transition period may involve temporary irregularities as the body adjusts to new metabolic parameters. The rate of weight loss matters—more gradual reduction may cause fewer menstrual disruptions than rapid weight loss, though tirzepatide-induced weight loss occurs relatively quickly compared to lifestyle modification alone. Severe energy deficits from extreme caloric restriction can potentially suppress reproductive function.
Clinical trial data specifically examining tirzepatide's effects on menstrual cycles and reproductive hormones remain limited. The pivotal SURMOUNT and SURPASS trial programs primarily focused on weight loss and glycemic outcomes, with reproductive health not designated as a primary endpoint. Post-marketing reports provide some insights into menstrual pattern changes among women taking tirzepatide, though these have not been systematically analyzed.
In the SURMOUNT-1 trial, which evaluated tirzepatide for chronic weight management in adults without diabetes, approximately 67% of participants were women. While menstrual irregularities were not systematically reported as adverse events in published results, the substantial weight loss achieved (approximately 20.9% with the 15 mg dose) would be expected to influence reproductive hormone dynamics in premenopausal women based on established weight loss physiology.
Studies of other GLP-1 receptor agonists provide relevant context. Research on semaglutide and liraglutide has documented menstrual cycle changes associated with significant weight reduction. Studies examining women with PCOS treated with liraglutide have shown improvements in menstrual regularity alongside metabolic benefits, suggesting that GLP-1-based therapies may positively influence reproductive function in this population through insulin sensitization and weight loss.
Key considerations from available evidence:
No direct hormonal mechanism linking tirzepatide to menstrual disruption has been identified
Metabolic improvements (reduced insulin resistance, decreased androgens) may benefit women with PCOS
The magnitude and rapidity of weight loss correlate with likelihood of temporary menstrual changes
Long-term data on reproductive outcomes remain limited
Healthcare providers should counsel women of reproductive age about potential menstrual changes when initiating tirzepatide. The FDA label includes a warning that tirzepatide may reduce the effectiveness of oral hormonal contraceptives due to delayed gastric emptying. The prescribing information recommends using a non-oral contraceptive method or adding a barrier method for 4 weeks after treatment initiation and for 4 weeks after each dose escalation.
Women experiencing menstrual changes while taking tirzepatide can implement several strategies to monitor and manage these alterations effectively. Maintaining detailed menstrual cycle records provides valuable information for healthcare providers to distinguish between benign adaptive changes and patterns requiring further evaluation.
Practical management strategies include:
Cycle tracking: Use a menstrual diary or smartphone application to document cycle length, flow characteristics, and associated symptoms
Nutritional adequacy: Ensure sufficient caloric intake to support metabolic health despite weight loss goals; extreme caloric restriction may exacerbate menstrual irregularities
Micronutrient optimization: Maintain adequate iron intake, particularly if experiencing heavier menstrual bleeding
Contraceptive considerations: Discuss alternative contraceptive methods with your provider, as tirzepatide may affect oral contraceptive absorption
For women with pre-existing menstrual irregularities or PCOS, tirzepatide treatment may ultimately improve cycle regularity as metabolic parameters normalize. However, this improvement may take several months to manifest. Patience during the adjustment period is important, though persistent or concerning changes warrant medical evaluation.
If menstrual irregularities cause significant distress or interfere with quality of life, healthcare providers may consider several approaches. Any medication adjustments, including changes to the tirzepatide dose or titration schedule, should be made under healthcare provider guidance based on overall tolerability and treatment goals.
Women planning pregnancy should discuss tirzepatide use with their healthcare provider. The medication should be discontinued when pregnancy is recognized or before planned conception. Tirzepatide has a half-life of approximately 5 days, with elimination occurring over several weeks. The FDA prescribing information does not specify a required washout period before conception, so women should consult with their healthcare provider about appropriate timing. The return of regular ovulation following significant weight loss may actually improve fertility in women with obesity-related reproductive dysfunction.
Regarding lactation, limited data are available on tirzepatide use during breastfeeding. Women should discuss the potential benefits and risks with their healthcare provider.
While many menstrual changes during tirzepatide treatment represent benign adaptive responses to weight loss, certain patterns warrant prompt medical evaluation to exclude other underlying conditions. Women should maintain open communication with their healthcare providers about reproductive health changes throughout treatment.
Contact your healthcare provider if you experience:
Absent periods (amenorrhea): Missing three or more consecutive menstrual cycles if previously regular, or six or more months if previously irregular
Heavy bleeding (menorrhagia): Soaking through a pad or tampon every hour for several consecutive hours, or periods lasting longer than seven days
Severe pain: New or worsening menstrual cramping not relieved by over-the-counter medications
Intermenstrual bleeding: Bleeding or spotting between periods that persists beyond initial treatment months
Pregnancy possibility: Any missed period when pregnancy is possible, as tirzepatide is not recommended during pregnancy
Urgent warning signs: Heavy bleeding with dizziness, fainting, rapid heartbeat, or severe weakness requires emergency evaluation
Your healthcare provider may recommend specific investigations to evaluate persistent menstrual irregularities. These may include pregnancy testing, complete blood count to assess for anemia, thyroid function tests (as thyroid disorders commonly affect menstrual cycles), and reproductive hormone panels measuring FSH, LH, estradiol, and prolactin levels. Pelvic ultrasound may be indicated if structural abnormalities are suspected.
For women with known PCOS or other reproductive endocrine conditions, baseline and follow-up assessments of metabolic and reproductive parameters can help distinguish medication effects from underlying disease progression. Collaboration between your primary care provider or endocrinologist and a gynecologist may optimize management of both metabolic and reproductive health.
Additional reasons to seek medical advice:
Symptoms suggesting pregnancy (nausea beyond typical tirzepatide side effects, breast tenderness, fatigue)
Signs of infection (fever, unusual vaginal discharge, pelvic pain)
Significant mood changes or depression related to menstrual irregularities
Concerns about fertility or family planning while taking tirzepatide
Proactive communication with your healthcare team ensures that menstrual changes are appropriately evaluated and managed, optimizing both the metabolic benefits of tirzepatide treatment and your overall reproductive health.
Yes, tirzepatide can indirectly cause menstrual irregularities through significant weight loss and metabolic changes that affect reproductive hormone balance. Women may experience changes in cycle timing, flow intensity, missed periods, or breakthrough bleeding as the body adjusts to new metabolic parameters.
Yes, tirzepatide may reduce the effectiveness of oral hormonal contraceptives due to delayed gastric emptying. The FDA recommends using a non-oral contraceptive method or adding a barrier method for 4 weeks after starting treatment and for 4 weeks after each dose increase.
Yes, tirzepatide should be discontinued when pregnancy is recognized or before planned conception. Women should consult their healthcare provider about appropriate timing for discontinuation, as the medication has a half-life of approximately 5 days with elimination occurring over several weeks.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.