LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Weight loss injections like semaglutide (Wegovy) and tirzepatide (Zepbound) have transformed obesity treatment, but they aren't appropriate for everyone. Certain medical conditions, family histories, and life circumstances create absolute contraindications or require careful medical evaluation before starting treatment. Understanding who shouldn't take weight loss injections is essential for patient safety, as these medications carry specific risks including potential thyroid tumors, pancreatitis, and complications during pregnancy. This guide outlines key contraindications, medical conditions requiring caution, and situations demanding thorough consultation with your healthcare provider before initiating GLP-1 or dual GIP/GLP-1 receptor agonist therapy.
Quick Answer: Individuals with personal or family history of medullary thyroid carcinoma or MEN 2 syndrome, known hypersensitivity to these medications, pregnant or breastfeeding women, and those with certain medical conditions should not take weight loss injections without careful medical evaluation.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections represent a class of medications that include glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 receptor agonists such as tirzepatide (Zepbound). While semaglutide (Ozempic) and tirzepatide (Mounjaro) are FDA-approved for type 2 diabetes management, only Wegovy and Zepbound have received FDA approval specifically for chronic weight management in adults with obesity (BMI ≥30) or overweight (BMI ≥27) with at least one weight-related comorbidity.
These medications work by mimicking naturally occurring hormones released after eating. They slow gastric emptying, which prolongs the feeling of fullness after meals. They also act on appetite centers in the brain, particularly the hypothalamus, to reduce hunger signals and food cravings. Additionally, these medications enhance insulin secretion in a glucose-dependent manner while suppressing inappropriate glucagon release.
Clinical trials have demonstrated substantial weight loss outcomes. In the STEP 1 trial, semaglutide 2.4 mg produced approximately 15% weight loss at 68 weeks, while the SURMOUNT-1 trial showed tirzepatide achieved 15-21% weight loss at 72 weeks when combined with lifestyle modifications. These medications are administered via subcutaneous injection, typically once weekly, using pre-filled pens designed for self-administration. Treatment typically begins with a lower dose that gradually increases over several weeks to minimize gastrointestinal side effects.
While these medications offer significant benefits for appropriate candidates, they are not suitable for everyone. Understanding contraindications and safety considerations is essential before initiating treatment, as certain medical conditions, medications, and life circumstances may preclude their use or require careful medical supervision.
Several absolute contraindications exist for weight loss injections, meaning these medications should not be used under specific circumstances. The most critical contraindication is a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Animal studies demonstrated thyroid C-cell tumors at clinically relevant exposures, and while the human risk remains uncertain, the FDA requires a boxed warning about this potential thyroid cancer risk.
Patients with a known hypersensitivity to semaglutide, tirzepatide, or any component of these formulations should avoid these medications. Serious hypersensitivity reactions, including anaphylaxis and angioedema, have been reported in post-marketing surveillance. Symptoms may include difficulty breathing, swelling of the face or throat, severe rash, or rapid heartbeat requiring immediate medical attention.
Individuals with a history of pancreatitis should use these medications with caution, if at all. The FDA labels advise that these medications have not been studied in patients with a history of pancreatitis and other treatment options should be considered. While causality has not been definitively established, acute pancreatitis has been observed in clinical trials and post-marketing reports. If pancreatitis is suspected during treatment, the medication should be discontinued immediately.
Regarding pediatric use, Wegovy is approved for chronic weight management in patients aged 12 years and older with obesity, while Zepbound is approved only for adults 18 years and older. These medications should not be used in patients with type 1 diabetes. The safety and efficacy in these populations have not been established. Patients should not use multiple GLP-1 or GIP/GLP-1 medications simultaneously due to overlapping mechanisms and increased risk of adverse effects.
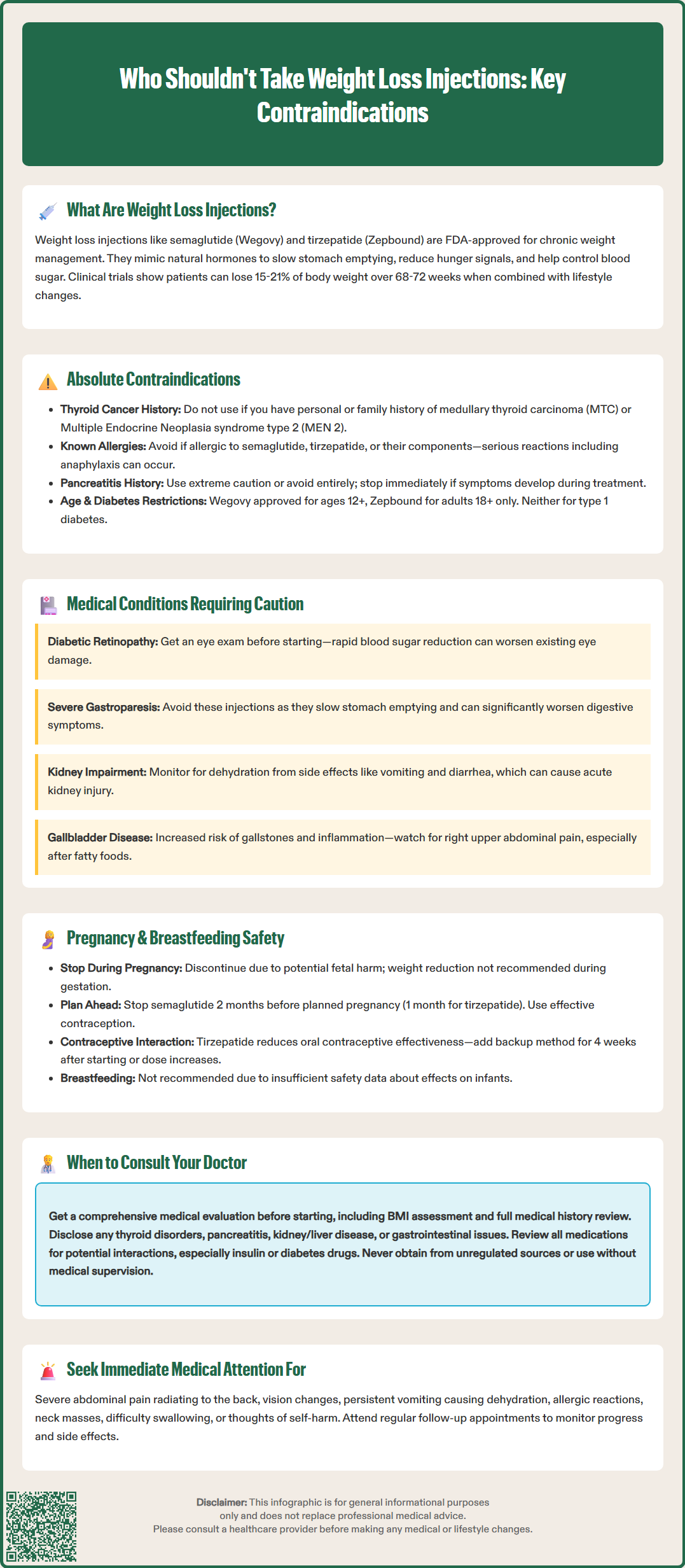
Several medical conditions require careful evaluation before initiating weight loss injections, as they may increase the risk of complications. Diabetic retinopathy warrants particular attention, especially in patients with type 2 diabetes. Rapid glucose reduction associated with GLP-1 therapy has been linked to worsening of diabetic retinopathy in some studies, particularly the SUSTAIN-6 trial with semaglutide. Patients with pre-existing retinopathy should undergo ophthalmologic evaluation and close monitoring if treatment is initiated.
Severe gastrointestinal disease, particularly severe gastroparesis, may preclude the use of these medications. The delayed gastric emptying effect of these medications may worsen symptoms in patients with severe gastroparesis. Other gastrointestinal conditions such as inflammatory bowel disease or gastroesophageal reflux disease should be evaluated on an individual basis, as these medications may potentially exacerbate symptoms including nausea, vomiting, abdominal pain, and bloating in some patients.
Regarding renal function, no dose adjustment is required for patients with renal impairment for either semaglutide or tirzepatide. However, gastrointestinal side effects such as severe vomiting and diarrhea can lead to dehydration and acute kidney injury. Patients with any degree of renal impairment should be monitored for dehydration and worsening kidney function if severe gastrointestinal adverse events occur.
Gallbladder disease represents another concern, as substantial weight loss itself increases the risk of cholelithiasis. Clinical trials have shown increased rates of gallbladder-related adverse events, including cholecystitis and cholelithiasis, in patients taking these medications. Patients with active gallbladder disease or a history of gallstones should be counseled about this risk and monitored for symptoms such as right upper quadrant pain, particularly after fatty meals.
Weight loss injections are not recommended during pregnancy and should be discontinued when pregnancy is recognized. Animal reproduction studies have shown fetal harm, including structural abnormalities and growth alterations, though human data remain limited. The potential risks to fetal development outweigh any benefits of weight loss during pregnancy, as weight reduction is not recommended during gestation.
Women of childbearing potential should use effective contraception while taking these medications. Due to the long half-life, semaglutide should be discontinued at least 2 months before a planned pregnancy, while tirzepatide should be stopped at least 1 month prior. Importantly, tirzepatide may decrease the exposure of oral contraceptives when co-administered. Women using oral contraceptives should consider using a non-oral method or adding a barrier method for 4 weeks after initiating tirzepatide and for 4 weeks after each dose escalation.
Breastfeeding considerations are complex, as there is insufficient data regarding the presence of these medications in human milk or their effects on the breastfed infant. The developmental and health benefits of breastfeeding should be weighed against the mother's clinical need for the medication and any potential adverse effects on the infant. Given the lack of safety data, most clinicians recommend considering alternative weight management approaches during lactation.
For postpartum women seeking weight management, alternative approaches should be prioritized during the breastfeeding period. These include evidence-based lifestyle modifications, dietary counseling, and gradual increases in physical activity as medically appropriate. Women should discuss their individual circumstances with their healthcare provider to develop a safe, effective weight management plan that considers both maternal health goals and infant nutrition needs. Weight loss injections may be considered after weaning, provided no other contraindications exist.
Comprehensive medical evaluation is essential before initiating weight loss injections. All patients should schedule a thorough consultation with their healthcare provider to review their complete medical history, current medications, and weight loss goals. This evaluation should include assessment of body mass index (BMI) to confirm eligibility (BMI ≥30, or ≥27 with at least one weight-related comorbidity such as hypertension, dyslipidemia, type 2 diabetes, or obstructive sleep apnea), previous weight loss attempts, and realistic expectations for treatment outcomes.
Patients should specifically inform their doctor if they have a history of the following conditions: thyroid disorders or thyroid nodules, pancreatitis or elevated pancreatic enzymes, kidney disease, liver disease, diabetic retinopathy, depression or suicidal ideation, gastroparesis or severe gastrointestinal disorders, or gallbladder disease. Additionally, any family history of medullary thyroid carcinoma or MEN 2 syndrome must be disclosed, as this represents an absolute contraindication to treatment.
Medication interactions require careful review. Patients taking insulin or insulin secretagogues (such as sulfonylureas) may require dose adjustments to prevent hypoglycemia. Oral medications with narrow therapeutic indices may have altered absorption due to delayed gastric emptying. Women using oral contraceptives who start tirzepatide should consider using a non-oral contraceptive method or adding a barrier method for 4 weeks after initiation and after each dose increase. Patients should provide a complete list of prescription medications, over-the-counter drugs, and supplements to their healthcare provider.
Immediate medical consultation is warranted if patients experience warning signs during treatment, including: severe abdominal pain that may radiate to the back (potential pancreatitis), visual changes, persistent nausea and vomiting leading to dehydration, signs of allergic reaction, symptoms of thyroid tumors (neck mass, difficulty swallowing, persistent hoarseness), or thoughts of self-harm. Regular follow-up appointments are essential for monitoring weight loss progress, managing side effects, and adjusting treatment as needed. Patients should never obtain these medications from unregulated sources or use them without proper medical supervision, as this significantly increases safety risks.
No, a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2) is an absolute contraindication to GLP-1 and dual GIP/GLP-1 receptor agonists. These medications carry an FDA boxed warning about potential thyroid C-cell tumor risk based on animal studies.
No, weight loss injections are not recommended during pregnancy and should be discontinued when pregnancy is recognized. Semaglutide should be stopped at least 2 months before planned pregnancy, while tirzepatide should be discontinued at least 1 month prior, as animal studies have shown potential fetal harm.
Yes, individuals with a history of pancreatitis should use these medications with extreme caution, if at all. The FDA labels advise that these medications have not been studied in patients with prior pancreatitis, and acute pancreatitis has been observed in clinical trials and post-marketing reports.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.