LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Burping is a common digestive side effect experienced by patients taking tirzepatide (Mounjaro, Zepbound), a dual GIP and GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management. This symptom occurs primarily because tirzepatide slows gastric emptying—a key mechanism that helps control blood sugar and reduce appetite. When food remains in the stomach longer, it can lead to increased gas accumulation and burping (eructation). Understanding why this happens and how to manage it can help patients continue their treatment comfortably while achieving their therapeutic goals.
Quick Answer: Tirzepatide causes burping because it slows gastric emptying, leading to delayed food movement from the stomach and increased gas accumulation.
Tirzepatide is a once-weekly injectable medication approved by the FDA for the treatment of type 2 diabetes mellitus (marketed as Mounjaro) and chronic weight management (marketed as Zepbound). It represents a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. This dual mechanism distinguishes tirzepatide from single-target GLP-1 receptor agonists such as semaglutide.
The medication works through multiple complementary pathways to improve glycemic control and promote weight loss. By activating GLP-1 receptors, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon release, and slows gastric emptying. The additional GIP receptor activation further enhances insulin secretion. These combined effects result in improved blood glucose regulation and reduced appetite.
The slowing of gastric emptying is particularly relevant to understanding digestive side effects, including burping. When tirzepatide delays the movement of food from the stomach into the small intestine, it can contribute to symptoms like burping (eructation). Burping primarily occurs due to swallowed air and transient relaxations of the lower esophageal sphincter, which can be exacerbated when gastric emptying is delayed. This mechanism helps explain why burping and other upper gastrointestinal symptoms are among the most frequently reported adverse effects during tirzepatide therapy.
It's important to note that tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis, as its effects on gastric emptying may worsen these conditions. Gastrointestinal adverse events are generally dose-dependent, with higher doses typically associated with more pronounced effects.
Burping, medically termed eructation, is a recognized gastrointestinal side effect of tirzepatide, though it is not always explicitly listed as a separate adverse event in clinical trial data. According to FDA prescribing information and pivotal clinical trials, gastrointestinal adverse effects are the most common side effects associated with tirzepatide therapy.
In the SURPASS clinical trial program evaluating tirzepatide for type 2 diabetes, gastrointestinal adverse events were dose-dependent. According to the Mounjaro prescribing information, nausea occurred in 17.9%, 19.8%, and 22.2% of patients receiving 5 mg, 10 mg, and 15 mg doses respectively. Diarrhea occurred in 13.3-16.4% of patients, vomiting in 6.2-9.8%, and dyspepsia (indigestion) in 6.1-9.6% of participants. Eructation (burping) is not specifically listed as a separate adverse event in the prescribing information tables.
The SURMOUNT trials examining tirzepatide for weight management showed similar patterns, with gastrointestinal side effects being dose-related and most prominent during the initial titration period. Most patients experience these symptoms during the first 4-8 weeks of treatment or following dose increases, with symptoms typically diminishing over time as the body adapts to the medication.
It is important to note that individual experiences vary considerably. Some patients report minimal or no burping, while others find it bothersome enough to discuss management strategies with their healthcare provider. The symptom does not necessarily indicate treatment failure or a serious underlying problem, but rather reflects the medication's expected pharmacological effect on gastrointestinal motility. While some patients may report burping as a symptom in clinical practice, formal documentation of its specific frequency is limited in the published clinical trial data.
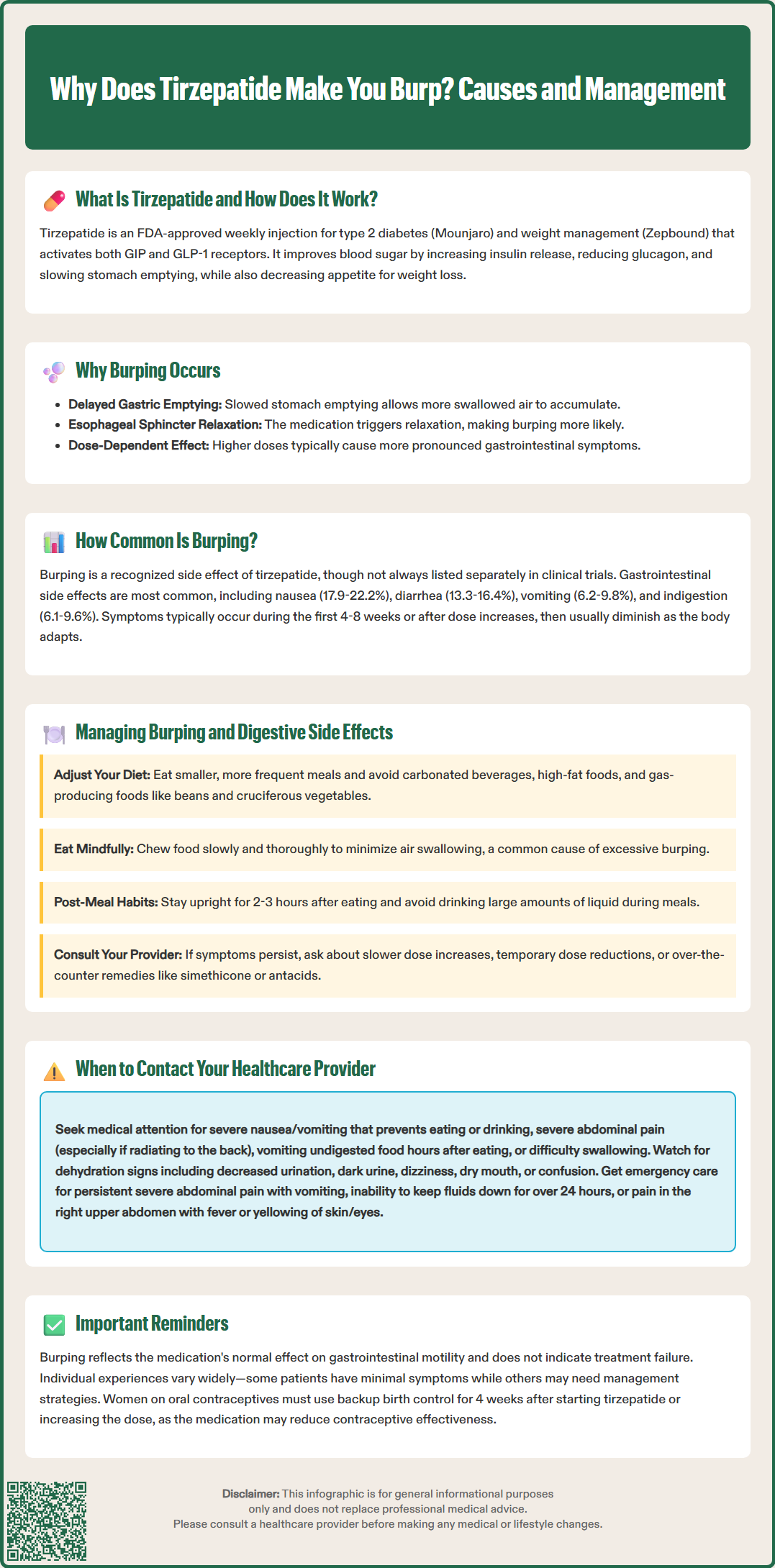
Most patients can successfully manage burping and related digestive symptoms with practical dietary and lifestyle modifications. These strategies work by reducing gastric distension, minimizing gas production, and accommodating the medication's effect on delayed gastric emptying.
Dietary modifications form the cornerstone of symptom management:
Eat smaller, more frequent meals rather than large portions. Since tirzepatide slows gastric emptying, smaller meal volumes reduce the likelihood of gastric distension and reflux of air.
Avoid carbonated beverages, which introduce additional gas into the digestive system and can exacerbate burping.
Limit high-fat foods, as fats further delay gastric emptying and may worsen symptoms when combined with tirzepatide's effects.
Reduce intake of gas-producing foods such as beans, cruciferous vegetables (broccoli, cabbage, Brussels sprouts), onions, and certain artificial sweeteners.
Eat slowly and chew thoroughly to minimize air swallowing (aerophagia), a common contributor to burping.
Behavioral strategies can also provide relief:
Avoid lying down immediately after eating; remain upright for at least 2-3 hours after meals to facilitate digestion.
Stay well-hydrated throughout the day, but avoid drinking large volumes of liquid with meals.
Identify and avoid personal trigger foods through systematic observation.
If changing your weekly injection day, ensure at least 72 hours have passed since your last dose, per FDA guidance.
For persistent symptoms, over-the-counter remedies such as simethicone may help break up gas bubbles, though evidence for its effectiveness specifically for burping is limited. For reflux-type symptoms, antacids, H2 blockers, or proton pump inhibitors may be appropriate under healthcare provider guidance.
If gastrointestinal symptoms are significant, your healthcare provider may recommend slower dose titration, temporary dose reduction, or delaying dose escalation. Importantly, women taking oral contraceptives should use a backup method for 4 weeks after starting tirzepatide or increasing the dose, as the medication may reduce contraceptive effectiveness. Never discontinue or adjust your tirzepatide dose without medical guidance.
While burping alone is generally a benign and manageable side effect, certain symptoms warrant prompt medical evaluation to rule out more serious complications or conditions requiring intervention.
Contact your healthcare provider if you experience:
Severe or persistent nausea and vomiting that prevents adequate fluid or food intake, as this may lead to dehydration and electrolyte imbalances.
Severe abdominal pain, particularly if persistent, radiating to the back, or accompanied by vomiting, which could indicate pancreatitis—a rare but serious adverse effect of GLP-1 receptor agonists.
Persistent vomiting of undigested food consumed many hours earlier, which may suggest gastroparesis or severe delayed gastric emptying.
Signs of dehydration including decreased urination, dark urine, dizziness, dry mouth, or confusion.
Difficulty swallowing or sensation of food getting stuck, which requires evaluation for esophageal complications.
Unintended weight loss beyond expected therapeutic effects, or inability to maintain adequate nutrition.
New or worsening heartburn that does not respond to over-the-counter antacids, as this may indicate gastroesophageal reflux disease requiring treatment.
Pain in the right upper abdomen, fever, or yellowing of the skin/eyes, which could indicate gallbladder disease, a known risk with tirzepatide therapy.
Seek emergency care immediately if you experience severe, persistent abdominal pain with vomiting, inability to keep fluids down for more than 24 hours, or signs of significant dehydration such as dizziness when standing, confusion, or very low urine output.
Your healthcare provider may recommend dose adjustment, temporary treatment interruption, or additional evaluation depending on symptom severity. In some cases, diagnostic testing such as upper gastrointestinal imaging or gastric emptying studies may be appropriate to assess gastric function.
It is also important to discuss any side effects at your regular follow-up appointments, even if not severe. Your provider can assess whether symptoms are within the expected range, optimize your treatment regimen, and ensure you are achieving therapeutic goals while maintaining acceptable tolerability.
Most patients experience burping and other gastrointestinal symptoms during the first 4-8 weeks of treatment or following dose increases, with symptoms typically diminishing over time as the body adapts to the medication.
Over-the-counter remedies such as simethicone may help break up gas bubbles, though evidence for its effectiveness specifically for burping is limited. Dietary modifications including smaller meals and avoiding carbonated beverages are typically the most effective first-line strategies.
Burping reflects tirzepatide's pharmacological effect on slowing gastric emptying, which is part of its mechanism of action. However, the absence of burping does not mean the medication is not working, as individual experiences with side effects vary considerably.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.