LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide cause birth defects? Tirzepatide (Mounjaro, Zepbound) is a dual GIP and GLP-1 receptor agonist used for type 2 diabetes and weight management. Limited human data exist regarding its safety during pregnancy. Animal studies have shown fetal growth abnormalities and skeletal malformations at clinically relevant doses, though these findings don't always predict human outcomes. The FDA has not established a definitive link between tirzepatide and human birth defects due to insufficient clinical data. Healthcare providers recommend discontinuing tirzepatide when pregnancy is recognized and using effective contraception during treatment. Understanding the evidence and timing of discontinuation is essential for women of reproductive potential.
Quick Answer: There is insufficient human data to confirm whether tirzepatide causes birth defects, though animal studies show fetal abnormalities at clinically relevant doses.
Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for chronic weight management) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. Currently, there is limited human data regarding tirzepatide use during pregnancy and its potential effects on fetal development. The FDA-approved prescribing information for tirzepatide products includes a pregnancy risk summary that emphasizes the absence of adequate well-controlled studies in pregnant women.
Animal reproduction studies have been conducted with tirzepatide in rats and rabbits. These studies revealed adverse developmental outcomes, including fetal growth abnormalities and skeletal malformations, when administered during organogenesis at clinically relevant exposures. However, animal findings do not always predict human outcomes, and the clinical significance of these observations remains uncertain.
The mechanism by which tirzepatide might affect fetal development is not fully understood. Some research with GLP-1 receptor agonists has suggested potential metabolic effects that could theoretically influence pregnancy, though specific impacts on human pregnancy are unknown. Additionally, the significant weight loss associated with tirzepatide therapy could influence pregnancy outcomes through nutritional pathways.
Given the lack of controlled human studies and the presence of adverse findings in animal models, healthcare providers generally advise against tirzepatide use during pregnancy. Weight loss medications like Zepbound are not recommended during pregnancy and should be discontinued when pregnancy is recognized. Women of reproductive potential should discuss contraception and pregnancy planning with their healthcare team before initiating tirzepatide therapy. The potential benefits of glycemic control must be weighed against unknown fetal risks, with alternative diabetes management strategies typically preferred during pregnancy.
The FDA has not established a definitive causal link between tirzepatide and birth defects in humans due to insufficient clinical data. The prescribing information for tirzepatide states that available data are inadequate to determine a drug-associated risk of major birth defects, miscarriage, or other adverse maternal or fetal outcomes. This uncertainty reflects the ethical and practical challenges of conducting pregnancy studies with investigational medications.
Animal studies provide the primary safety signal for concern. In developmental toxicity studies, tirzepatide administration during organogenesis resulted in decreased fetal growth and increased incidences of skeletal malformations in both rats and rabbits. These effects occurred at systemic exposures that were below those achieved at the maximum recommended human dose. Specific findings included delayed ossification and skeletal variations, which may indicate disrupted fetal development during critical growth periods.
The background risk of major birth defects in the general US population is approximately 2-4%, while the risk of miscarriage in clinically recognized pregnancies ranges from 15-20%, according to CDC data. For women with diabetes, baseline risks may be elevated due to hyperglycemia itself, with poorly controlled diabetes associated with increased rates of congenital malformations, particularly cardiac and neural tube defects. This complicates risk assessment, as it becomes difficult to separate medication effects from underlying disease contributions.
The FDA guidance emphasizes that healthcare providers should discontinue tirzepatide in women who become pregnant. Weight loss medications like Zepbound are not recommended during pregnancy. The American Diabetes Association (ADA) recommends insulin as the preferred agent for glycemic control during pregnancy due to its established safety profile and inability to cross the placental barrier in significant amounts. Until more human data become available, a precautionary approach remains the standard of care.
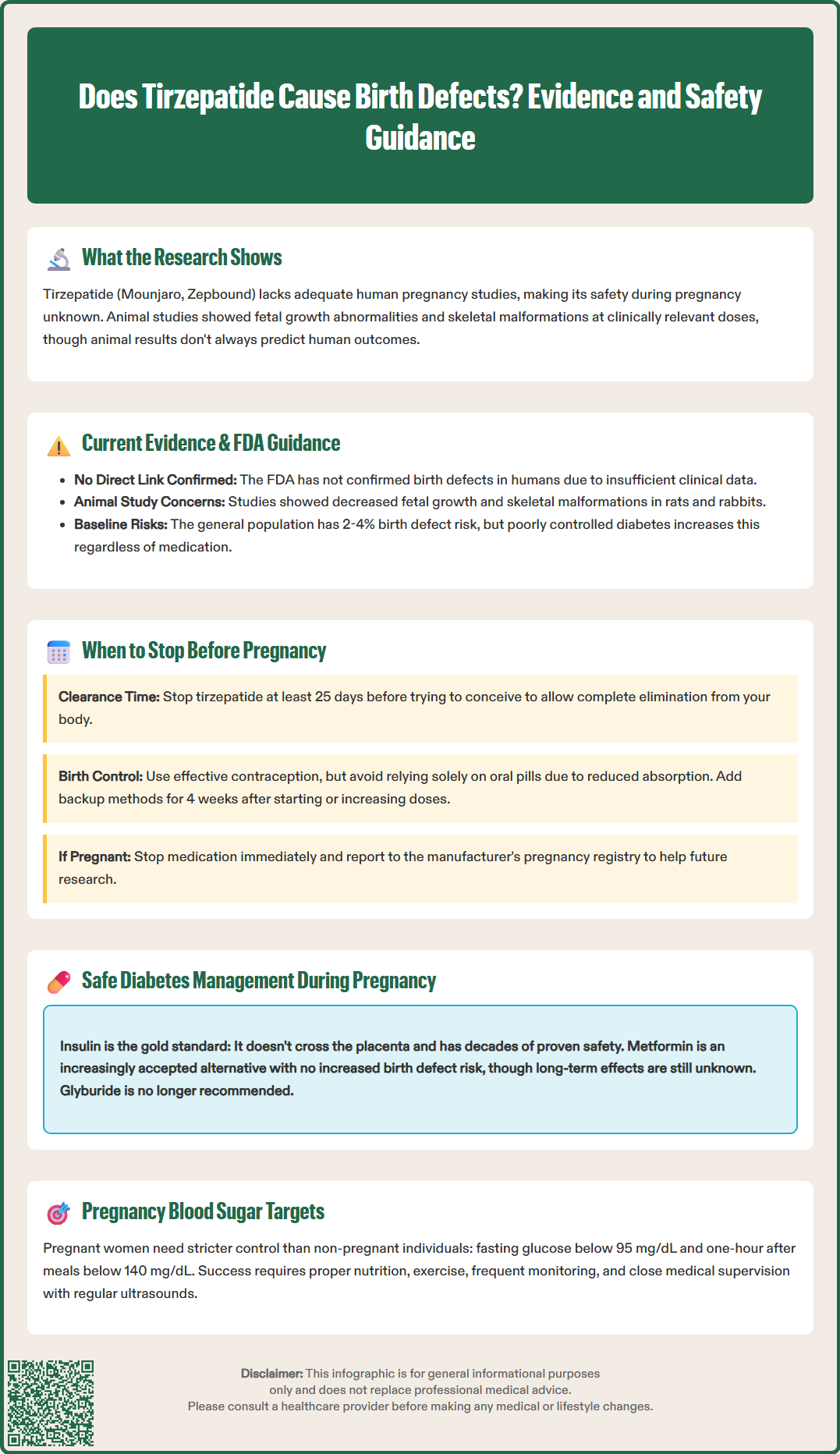
Tirzepatide has an elimination half-life of approximately 5 days. Following standard pharmacokinetic principles, it takes approximately five half-lives for a medication to be substantially eliminated from the body, which equates to roughly 25 days for tirzepatide. Women planning pregnancy should discuss appropriate timing of discontinuation with their healthcare provider based on their individual clinical situation.
The rationale for establishing a washout period relates to the critical period of organogenesis, which occurs during weeks 3-8 of gestation (calculated from the first day of the last menstrual period). Many women do not recognize pregnancy until 4-6 weeks of gestation, making preconception planning essential. By ensuring tirzepatide is cleared from the system before conception, women can minimize potential exposure during the embryo's formation of major organ systems.
Women of childbearing potential should use effective contraception while taking tirzepatide. Importantly, tirzepatide can delay gastric emptying, which may reduce the effectiveness of oral contraceptives. The prescribing information recommends using an alternative contraceptive method or adding a barrier method for 4 weeks after tirzepatide initiation and for 4 weeks after each dose escalation. This precaution is particularly important given the potential for reduced oral contraceptive absorption due to delayed gastric emptying, not due to weight loss itself.
For women with unplanned pregnancies while taking tirzepatide, immediate discontinuation is recommended upon pregnancy confirmation. While exposure during early pregnancy is concerning based on animal data, it does not automatically predict adverse outcomes. These patients should receive prompt referral to maternal-fetal medicine specialists for detailed ultrasound evaluation and ongoing monitoring. Patients should be encouraged to report pregnancies that occur while taking tirzepatide to the manufacturer's pregnancy registry to improve future understanding of tirzepatide's effects during human pregnancy.
Insulin remains the gold standard for diabetes management during pregnancy, with decades of safety data supporting its use across all trimesters. Both rapid-acting insulin analogs (insulin lispro, insulin aspart) and long-acting basal insulins (insulin detemir, insulin glargine) have been studied extensively in pregnant women and are not associated with increased birth defect risks. Insulin does not cross the placenta in clinically significant amounts, making it the preferred choice for achieving tight glycemic control without direct fetal exposure.
The American College of Obstetricians and Gynecologists (ACOG) and the ADA recommend target blood glucose levels during pregnancy of fasting glucose below 95 mg/dL and one-hour postprandial glucose below 140 mg/dL (or two-hour postprandial below 120 mg/dL). For preconception planning, the ADA recommends achieving an A1C of less than 6.5% if this can be accomplished without significant hypoglycemia. These targets are more stringent than non-pregnancy goals because even modest hyperglycemia can affect fetal growth and development. Achieving these targets typically requires multiple daily insulin injections or continuous subcutaneous insulin infusion (insulin pump therapy).
Metformin represents an alternative oral agent with growing evidence for pregnancy safety. While metformin does cross the placenta, multiple studies and meta-analyses have not demonstrated increased risks of major congenital malformations compared to insulin therapy. However, the ADA notes that long-term offspring outcomes remain uncertain. Metformin is increasingly used for gestational diabetes management and may be continued in women with pre-existing type 2 diabetes who become pregnant, though insulin remains first-line. The decision to use metformin should involve shared decision-making between patient and provider, considering individual circumstances and preferences.
Glyburide, a second-generation sulfonylurea, was previously considered for gestational diabetes but has fallen out of favor due to concerns about neonatal hypoglycemia and possible increased birth weight. Most current guidelines recommend against initiating glyburide during pregnancy. Comprehensive diabetes management during pregnancy extends beyond medication selection to include medical nutrition therapy, regular physical activity as tolerated, frequent self-monitoring of blood glucose, and close obstetric surveillance with serial ultrasounds to assess fetal growth and amniotic fluid volume. Women transitioning from tirzepatide to pregnancy-safe alternatives should work closely with endocrinologists and maternal-fetal medicine specialists to ensure optimal glycemic control throughout the preconception period and all stages of pregnancy.
Women planning pregnancy should discuss discontinuation timing with their healthcare provider, typically allowing approximately 25 days (five half-lives) for tirzepatide to be substantially eliminated from the body before conception. This timing helps minimize potential exposure during the critical organogenesis period of weeks 3-8 of gestation.
Insulin remains the gold standard for diabetes management during pregnancy with decades of safety data. It does not cross the placenta in clinically significant amounts and is recommended by both the American Diabetes Association and the American College of Obstetricians and Gynecologists as the preferred agent for glycemic control during pregnancy.
Yes, tirzepatide can delay gastric emptying, which may reduce the effectiveness of oral contraceptives. The prescribing information recommends using an alternative contraceptive method or adding a barrier method for 4 weeks after tirzepatide initiation and for 4 weeks after each dose escalation to ensure adequate contraceptive protection.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.